Brain–body mechanisms contribute to sexual dimorphism in amyotrophic lateral sclerosis
Brain–body mechanisms contribute to sexual dimorphism in amyotrophic lateral sclerosis"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
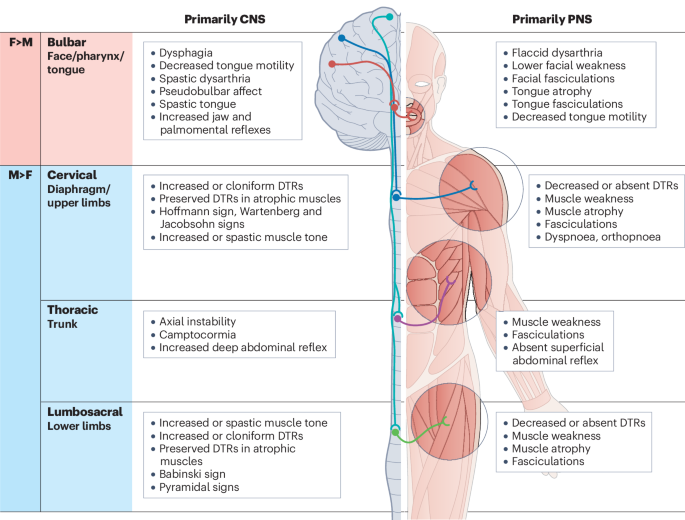
ABSTRACT Amyotrophic lateral sclerosis (ALS) is the most common form of human motor neuron disease. It is characterized by the progressive degeneration of upper and lower motor neurons,
leading to generalized motor weakness and, ultimately, respiratory paralysis and death within 3–5 years. The disease is shaped by genetics, age, sex and environmental stressors, but no cure
or routine biomarkers exist for the disease. Male individuals have a higher propensity to develop ALS, and a different manifestation of the disease phenotype, than female individuals.
However, the mechanisms underlying these sex differences remain a mystery. In this Review, we summarize the epidemiology of ALS, examine the sexually dimorphic presentation of the disease
and highlight the genetic variants and molecular pathways that might contribute to sex differences in humans and animal models of ALS. We advance the idea that sexual dimorphism in ALS
arises from the interactions between the CNS and peripheral organs, involving vascular, metabolic, endocrine, musculoskeletal and immune systems, which are strikingly different between male
and female individuals. Finally, we review the response to treatments in ALS and discuss the potential to implement future personalized therapeutic strategies for the disease. KEY POINTS *
The molecular mechanisms that underlie sex differences in amyotrophic lateral sclerosis (ALS), in particular the higher prevalence and earlier onset in male over female individuals, are
poorly understood. * The disease mechanisms are modulated by age, genetics and environmental factors that interact to produce a wide range of ALS phenotypes with differences in symptom
presentation and disease onset and duration. * Interactions between the nervous systems and peripheral organs and systems that are strikingly different between sexes in terms of molecular
signature and physiology are key to our understanding of sexual dimorphism in ALS. * Harnessing brain–body interactions could allow the identification of biomarkers and offer new avenues for
the treatment of ALS. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution
Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $29.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12
print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be
subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR
CONTENT BEING VIEWED BY OTHERS DISSOCIATION OF DISEASE ONSET, PROGRESSION AND SEX DIFFERENCES FROM ANDROGEN RECEPTOR LEVELS IN A MOUSE MODEL OF AMYOTROPHIC LATERAL SCLEROSIS Article Open
access 29 April 2021 FEMALE SEX MITIGATES MOTOR AND BEHAVIOURAL PHENOTYPES IN TDP-43Q331K KNOCK-IN MICE Article Open access 05 November 2020 MULTIOMIC ALS SIGNATURES HIGHLIGHT SUBCLUSTERS
AND SEX DIFFERENCES SUGGESTING THE MAPK PATHWAY AS THERAPEUTIC TARGET Article Open access 07 June 2024 REFERENCES * Gorelick, P. B. & Alter, M. (eds.) _Handbook of Neuroepidemiology_
(Marcel Dekker, 1994). * McGuire, V., Longstreth, W. T., Koepsell, T. D. & van Belle, G. Incidence of amyotrophic lateral sclerosis in three counties in Western Washington state.
_Neurology_ 47, 571–573 (1996). CAS PubMed Google Scholar * Abhinav, K. et al. Amyotrophic lateral sclerosis in South-East England: a population-based study. _Neuroepidemiology_ 29, 44–48
(2007). CAS PubMed Google Scholar * Chio, A. et al. Epidemiology of ALS in Italy: a 10-year prospective population-based study. _Neurology_ 72, 725–731 (2009). CAS PubMed Google
Scholar * Vázquez, M. C. et al. Incidence and prevalence of amyotrophic lateral sclerosis in Uruguay: a population-based study. _Neuroepidemiology_ 30, 105–111 (2008). PubMed Google
Scholar * Mehta, P. et al. Prevalence of amyotrophic lateral sclerosis — United States, 2015. _MMWR Morb. Mortal. Wkly. Rep._ 67, 1285–1289 (2018). PubMed PubMed Central Google Scholar *
Traynor, B. J. et al. Incidence and prevalence of ALS in Ireland, 1995-1997: a population-based study. _Neurology_ 52, 504 (1999). CAS PubMed Google Scholar * Atsuta, N. et al. Age at
onset influences on wide-ranged clinical features of sporadic amyotrophic lateral sclerosis. _J. Neurol. Sci._ 276, 163–169 (2009). PubMed Google Scholar * Nalini, A., Thennarasu, K.,
Gourie-Devi, M., Shenoy, S. & Kulshreshtha, D. Clinical characteristics and survival pattern of 1153 patients with amyotrophic lateral sclerosis: experience over 30 years from India. _J.
Neurol. Sci._ 272, 60–70 (2008). CAS PubMed Google Scholar * Masrori, P. & Van Damme, P. Amyotrophic lateral sclerosis: a clinical review. _Eur. J. Neurol._ 27, 1918–1929 (2020). CAS
PubMed Google Scholar * Turner, M. R. et al. The diagnostic pathway and prognosis in bulbar-onset amyotrophic lateral sclerosis. _J. Neurol. Sci._ 294, 81–85 (2010). PubMed Google
Scholar * Zhang, H., Chen, L., Tian, J. & Fan, D. Disease duration of progression is helpful in identifying isolated bulbar palsy of amyotrophic lateral sclerosis. _BMC Neurol._ 21, 405
(2021). CAS PubMed PubMed Central Google Scholar * Kiernan, M. C. et al. Amyotrophic lateral sclerosis. _Lancet_ 377, 942–955 (2011). CAS PubMed Google Scholar * Strong, M. J. et al.
Amyotrophic lateral sclerosis-frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. _Amyotroph. Lateral Scler. Front. Degener._ 18, 153–174 (2017). Google Scholar *
Chio, A., Calvo, A., Moglia, C., Mazzini, L. & Mora, G. Phenotypic heterogeneity of amyotrophic lateral sclerosis: a population based study. _J. Neurol. Neurosurg. Psychiatry_ 82,
740–746 (2011). PubMed Google Scholar * Eisen, A. & Krieger, C. _Amyotrophic Lateral Sclerosis: a Synthesis of Research and Clinical Practice_ (Cambridge Univ. Press, 1998). * McCombe,
P. A. & Henderson, R. D. Effects of gender in amyotrophic lateral sclerosis. _Gend. Med._ 7, 557–570 (2010). PubMed Google Scholar * Vlassoff, C. Gender differences in determinants
and consequences of health and illness. _J. Health Popul. Nutr._ 25, 47–61 (2007). PubMed PubMed Central Google Scholar * Taylor, J. P., Brown, R. H. & Cleveland, D. W. Decoding ALS:
from genes to mechanism. _Nature_ 539, 197–206 (2016). PubMed PubMed Central Google Scholar * Pape, J. A. & Grose, J. H. The effects of diet and sex in amyotrophic lateral sclerosis.
_Rev. Neurol._ 176, 301–315 (2020). CAS PubMed Google Scholar * Trojsi, F., D’Alvano, G., Bonavita, S. & Tedeschi, G. Genetics and sex in the pathogenesis of amyotrophic lateral
sclerosis (ALS): is there a link? _Int. J. Mol. Sci._ 21, 3647 (2020). CAS PubMed PubMed Central Google Scholar * Mehta, P. et al. Incidence of amyotrophic lateral sclerosis in the
United States, 2014-2016. _Amyotroph. Lateral Scler. Frontotemporal Degener._ 23, 378–382 (2022). PubMed Google Scholar * Jun, K. Y. et al. Epidemiology of ALS in Korea using nationwide
big data. _J. Neurol. Neurosurg. Psychiatry_ 90, 395–403 (2019). PubMed Google Scholar * Shahrizaila, N. et al. Amyotrophic lateral sclerosis and motor neuron syndromes in Asia. _J.
Neurol. Neurosurg. Psychiatry_ 87, 821–830 (2016). CAS PubMed Google Scholar * Manjaly, Z. R. et al. The sex ratio in amyotrophic lateral sclerosis: a population based study. _Amyotroph.
Lateral Scler._ 11, 439–442 (2010). PubMed PubMed Central Google Scholar * Marin, B., Gil, J., Preux, P. M., Funalot, B. & Couratier, P. Incidence of amyotrophic lateral sclerosis in
the Limousin region of France, 1997–2007. _Amyotroph. Lateral Scler._ 10, 216–220 (2009). PubMed Google Scholar * Wolfson, C., Gauvin, D. E., Ishola, F. & Oskoui, M. Global prevalence
and incidence of amyotrophic lateral sclerosis: a systematic review. _Neurology_ 101, e613–e623 (2023). PubMed Google Scholar * Brown, C. A., Lally, C., Kupelian, V. & Flanders, W. D.
Estimated prevalence and incidence of amyotrophic lateral sclerosis and SOD1 and C9orf72 genetic variants. _Neuroepidemiology_ 55, 342–353 (2021). PubMed Google Scholar * Chiò, A. et al.
Secular trends of amyotrophic lateral sclerosis: the Piemonte and Valle d’Aosta Register. _JAMA Neurol._ 74, 1097–1104 (2017). PubMed PubMed Central Google Scholar * Newell, M. E.,
Adhikari, S. & Halden, R. U. Systematic and state-of the science review of the role of environmental factors in amyotrophic lateral sclerosis (ALS) or Lou Gehrig’s disease. _Sci. Total
Environ._ 817, 152504 (2022). CAS PubMed Google Scholar * Andrew, A. S. et al. Risk factors for amyotrophic lateral sclerosis: a regional United States case-control study. _Muscle Nerve_
63, 52–59 (2021). PubMed Google Scholar * Goutman, S. A. et al. Avocational exposure associations with ALS risk, survival, and phenotype: a Michigan-based case-control study. _J. Neurol.
Sci._ 457, 122899 (2024). PubMed Google Scholar * Walhout, R., Verstraete, E., van den Heuvel, M. P., Veldink, J. H. & van den Berg, L. H. Patterns of symptom development in patients
with motor neuron disease. _Amyotroph. Lateral Scler. Frontotemporal Degener._ 19, 21–28 (2018). PubMed Google Scholar * Feldman, E. L. et al. Amyotrophic lateral sclerosis. _Lancet_ 400,
1363–1380 (2022). CAS PubMed PubMed Central Google Scholar * Swinnen, B. & Robberecht, W. The phenotypic variability of amyotrophic lateral sclerosis. _Nat. Rev. Neurol._ 10, 661–670
(2014). PubMed Google Scholar * Zhang, H. G., Chen, L., Tang, L., Zhang, N. & Fan, D. S. Clinical features of isolated bulbar palsy of amyotrophic lateral sclerosis in Chinese
population. _Chin. Med. J._ 130, 1768–1772 (2017). PubMed PubMed Central Google Scholar * Burrell, J. R., Vucic, S. & Kiernan, M. C. Isolated bulbar phenotype of amyotrophic lateral
sclerosis. _Amyotroph. Lateral Scler._ 12, 283–289 (2011). PubMed Google Scholar * Raymond, J., Mehta, P., Larson, T., Pioro, E. P. & Horton, D. K. Reproductive history and age of
onset for women diagnosed with amyotrophic lateral sclerosis: data from the National ALS Registry: 2010–2018. _Neuroepidemiology_ 55, 416–424 (2021). PubMed Google Scholar * Grassano, M.
et al. Sex differences in amyotrophic lateral sclerosis survival and progression: a multidimensional analysis. _Ann. Neurol_. https://doi.org/10.1002/ana.26933 (2024). * Pinto, S., Gromicho,
M., Oliveira Santos, M. O., Swash, M. & De Carvalho, M. Respiratory onset in amyotrophic lateral sclerosis: clinical features and spreading pattern. _Amyotroph. Lateral Scler.
Frontotemporal Degener._ 24, 40–44 (2023). CAS PubMed Google Scholar * Fayemendy, P. et al. Hypermetabolism is a reality in amyotrophic lateral sclerosis compared to healthy subjects. _J.
Neurol. Sci._ 420, 117257 (2021). PubMed Google Scholar * Steyn, F. J. et al. Hypermetabolism in ALS is associated with greater functional decline and shorter survival. _J. Neurol.
Neurosurg. Psychiatry_ 89, 1016–1023 (2018). PubMed Google Scholar * Ferri, A. & Coccurello, R. What is ‘hyper’ in the ALS hypermetabolism? _Mediators Inflamm._ 2017, 7821672 (2017).
PubMed PubMed Central Google Scholar * Funalot, B., Desport, J. C., Sturtz, F., Camu, W. & Couratier, P. High metabolic level in patients with familial amyotrophic lateral sclerosis.
_Amyotroph. Lateral Scler._ 10, 113–117 (2009). CAS PubMed Google Scholar * Rosenfeld, J. & Strong, M. J. Challenges in the understanding and treatment of amyotrophic lateral
sclerosis/motor neuron disease. _Neurotherapeutics_ 12, 317–325 (2015). CAS PubMed PubMed Central Google Scholar * Rosen, D. R. et al. Mutations in Cu/Zn superoxide dismutase gene are
associated with familial amyotrophic lateral sclerosis. _Nature_ 362, 59–62 (1993). CAS PubMed Google Scholar * Corson, L. B., Strain, J. J., Culotta, V. C. & Cleveland, D. W.
Chaperone-facilitated copper binding is a property common to several classes of familial amyotrophic lateral sclerosis-linked superoxide dismutase mutants. _Proc. Natl Acad. Sci. USA_ 95,
6361–6366 (1998). CAS PubMed PubMed Central Google Scholar * Smeyers, J., Banchi, E. G. & Latouche, M. C9ORF72: what it is, what it does, and why it matters. _Front. Cell. Neurosci._
15, 661447 (2021). CAS PubMed PubMed Central Google Scholar * Balendra, R. & Isaacs, A. M. C9orf72-mediated ALS and FTD: multiple pathways to disease. _Nat. Rev. Neurol._ 14,
544–558 (2018). CAS PubMed PubMed Central Google Scholar * Suk, T. R. & Rousseaux, M. W. C. The role of TDP-43 mislocalization in amyotrophic lateral sclerosis. _Mol. Neurodegener._
15, 45 (2020). CAS PubMed PubMed Central Google Scholar * Prasad, A., Bharathi, V., Sivalingam, V., Girdhar, A. & Patel, B. K. Molecular mechanisms of TDP-43 misfolding and pathology
in amyotrophic lateral sclerosis. _Front. Mol. Neurosci._ 12, 25 (2019). CAS PubMed PubMed Central Google Scholar * Chio, A. et al. Extensive genetics of ALS: a population-based study
in Italy. _Neurology_ 79, 1983–1989 (2012). PubMed PubMed Central Google Scholar * Salmon, K. et al. The importance of offering early genetic testing in everyone with amyotrophic lateral
sclerosis. _Brain_ 145, 1207–1210 (2022). PubMed PubMed Central Google Scholar * Berdyński, M. et al. SOD1 mutations associated with amyotrophic lateral sclerosis analysis of variant
severity. _Sci. Rep._ 12, 103 (2022). PubMed PubMed Central Google Scholar * Bunton-Stasyshyn, R. K. A., Saccon, R. A., Fratta, P. & Fisher, E. M. C. SOD1 function and its
implications for amyotrophic lateral sclerosis pathology: new and renascent themes. _Neuroscientist_ 21, 519–529 (2015). CAS PubMed Google Scholar * Saccon, R. A., Bunton-Stasyshyn, R. K.
A., Fisher, E. M. C. & Fratta, P. Is SOD1 loss of function involved in amyotrophic lateral sclerosis? _Brain_ 136, 2342–2358 (2013). PubMed PubMed Central Google Scholar * Kim, G.,
Gautier, O., Tassoni-Tsuchida, E., Ma, X. R. & Gitler, A. D. ALS genetics: gains, losses, and implications for future therapies. _Neuron_ 108, 822–842 (2020). CAS PubMed PubMed Central
Google Scholar * Yim, M. B. et al. A gain-of-function of an amyotrophic lateral sclerosis-associated Cu,Zn-superoxide dismutase mutant: an enhancement of free radical formation due to a
decrease in Km for hydrogen peroxide. _Proc. Natl Acad. Sci. USA_ 93, 5709–5714 (1996). CAS PubMed PubMed Central Google Scholar * DeJesus-Hernandez, M. et al. Expanded GGGGCC
hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. _Neuron_ 72, 245–256 (2011). CAS PubMed PubMed Central Google Scholar * Renton, A. E. et al.
A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. _Neuron_ 72, 257–268 (2011). CAS PubMed PubMed Central Google Scholar * van Blitterswijk,
M., DeJesus-Hernandez, M. & Rademakers, R. How do C9ORF72 repeat expansions cause amyotrophic lateral sclerosis and frontotemporal dementia. _Curr. Opin. Neurol._ 25, 689–700 (2012).
PubMed PubMed Central Google Scholar * Curtis, A. F. et al. Sex differences in the prevalence of genetic mutations in FTD and ALS. _Neurology_ 89, 1633–1642 (2017). PubMed PubMed Central
Google Scholar * Esselin, F. et al. Clinical phenotype and inheritance in patients with C9ORF72 hexanucleotide repeat expansion: results from a large French cohort. _Front. Neurosci._ 14,
316 (2020). PubMed PubMed Central Google Scholar * Wiesenfarth, M. et al. Clinical and genetic features of amyotrophic lateral sclerosis patients with C9orf72 mutations. _Brain Commun._
5, fcad087 (2023). PubMed PubMed Central Google Scholar * Laaksovirta, H. et al. ALS in Finland: major genetic variants and clinical characteristics of patients with and without the
C9orf72 hexanucleotide repeat expansion. _Neurol. Genet._ 8, e665 (2022). PubMed PubMed Central Google Scholar * Yusipov, I. et al. Age-related DNA methylation changes are sex-specific: a
comprehensive assessment. _Aging_ 12, 24057–24080 (2020). CAS PubMed PubMed Central Google Scholar * Kovtun, I. V., Therneau, T. M. & McMurray, C. T. Gender of the embryo
contributes to CAG instability in transgenic mice containing a Huntington’s disease gene. _Hum. Mol. Genet._ 9, 2767–2775 (2000). CAS PubMed Google Scholar * Trojsi, F. et al. Comparative
analysis of C9orf72 and sporadic disease in a large multicenter ALS population: the effect of male sex on survival of C9orf72 positive patients. _Front. Neurosci._ 13, 485 (2019). PubMed
PubMed Central Google Scholar * Rooney, J. et al. C9orf72 expansion differentially affects males with spinal onset amyotrophic lateral sclerosis. _J. Neurol. Neurosurg. Psychiatry_ 88, 281
(2017). PubMed Google Scholar * Murphy, N. A. et al. Age-related penetrance of the C9orf72 repeat expansion. _Sci. Rep._ 7, 2116 (2017). PubMed PubMed Central Google Scholar *
Burberry, A. et al. C9orf72 suppresses systemic and neural inflammation induced by gut bacteria. _Nature_ 582, 89–94 (2020). CAS PubMed PubMed Central Google Scholar * Burberry, A. et
al. Loss-of-function mutations in the C9ORF72 mouse ortholog cause fatal autoimmune disease. _Sci. Transl. Med._ 8, 347ra93 (2016). PubMed PubMed Central Google Scholar * Ugolino, J. et
al. Loss of C9orf72 enhances autophagic activity via deregulated mTOR and TFEB signaling. _PLoS Genet._ 12, e1006443 (2016). PubMed PubMed Central Google Scholar * Koppers, M. et al.
C9orf72 ablation in mice does not cause motor neuron degeneration or motor deficits. _Ann. Neurol._ 78, 426–438 (2015). CAS PubMed PubMed Central Google Scholar * Cook, C. N. et al.
C9orf72 poly(GR) aggregation induces TDP-43 proteinopathy. _Sci. Transl. Med._ 12, eabb3774 (2020). CAS PubMed PubMed Central Google Scholar * Verdone, B. M. et al. A mouse model with
widespread expression of the C9orf72-linked glycine–arginine dipeptide displays non-lethal ALS/FTD-like phenotypes. _Sci. Rep._ 12, 5644 (2022). CAS PubMed PubMed Central Google Scholar
* Liu, Y. et al. C9orf72 BAC mouse model with motor deficits and neurodegenerative features of ALS/FTD. _Neuron_ 90, 521–534 (2016). CAS PubMed Google Scholar * Podcasy, J. L. &
Epperson, C. N. Considering sex and gender in Alzheimer disease and other dementias. _Dialogues Clin. Neurosci._ 18, 437–446 (2016). PubMed PubMed Central Google Scholar * Pengo, M. et
al. Sex influences clinical phenotype in frontotemporal dementia. _Neurol. Sci._ 43, 5281–5287 (2022). PubMed PubMed Central Google Scholar * McDonald, K. K. et al. TAR DNA-binding
protein 43 (TDP-43) regulates stress granule dynamics via differential regulation of G3BP and TIA-1. _Hum. Mol. Genet._ 20, 1400–1410 (2011). CAS PubMed Google Scholar * Buratti, E.
Nuclear factor TDP-43 and SR proteins promote in vitro and in vivo CFTR exon 9 skipping. _EMBO J._ 20, 1774–1784 (2001). CAS PubMed PubMed Central Google Scholar * Junttila, A. et al.
Cerebrospinal fluid TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis patients with and without the C9ORF72 hexanucleotide expansion. _Dement. Geriatr. Cogn. Dis.
Extra_ 6, 142–149 (2016). PubMed PubMed Central Google Scholar * Lombardi, M. et al. Variability in clinical phenotype in TARDBP mutations: amyotrophic lateral sclerosis case description
and literature review. _Genes_ 14, 2309 (2023). Google Scholar * Wegorzewska, I., Bell, S., Cairns, N. J., Miller, T. M. & Baloh, R. H. TDP-43 mutant transgenic mice develop features
of ALS and frontotemporal lobar degeneration. _Proc. Natl Acad. Sci. USA_ 106, 18809–18814 (2009). CAS PubMed PubMed Central Google Scholar * Watkins, J. et al. Female sex mitigates
motor and behavioural phenotypes in TDP-43Q331K knock-in mice. _Sci. Rep._ 10, 19220 (2020). CAS PubMed PubMed Central Google Scholar * Martin, S., Battistini, C. & Sun, J. A gut
feeling in amyotrophic lateral sclerosis: microbiome of mice and men. _Front. Cell. Infect. Microbiol._ 12, 839526 (2022). CAS PubMed PubMed Central Google Scholar * Guo, Y. et al. HO-1
induction in motor cortex and intestinal dysfunction in TDP-43 A315T transgenic mice. _Brain Res._ 1460, 88–95 (2012). CAS PubMed Google Scholar * Esmaeili, M. A., Panahi, M., Yadav, S.,
Hennings, L. & Kiaei, M. Premature death of TDP-43 (A315T) transgenic mice due to gastrointestinal complications prior to development of full neurological symptoms of amyotrophic lateral
sclerosis. _Int. J. Exp. Pathol._ 94, 56–64 (2013). CAS PubMed PubMed Central Google Scholar * Coughlan, K. S., Halang, L., Woods, I. & Prehn, J. H. M. A high-fat jelly diet
restores bioenergetic balance and extends lifespan in the presence of motor dysfunction and lumbar spinal cord motor neuron loss in TDP-43A315T mutant C57BL6/J mice. _Dis. Model. Mech._ 9,
1029–1037 (2016). CAS PubMed PubMed Central Google Scholar * Khymenets, O. et al. Role of sex and time of blood sampling in SOD1 and SOD2 expression variability. _Clin. Biochem._ 41,
1348–1354 (2008). CAS PubMed Google Scholar * Tang, L., Ma, Y., Liu, X., Chen, L. & Fan, D. Better survival in female SOD1-mutant patients with ALS: a study of SOD1-related natural
history. _Transl. Neurodegener._ 8, 2 (2019). CAS PubMed PubMed Central Google Scholar * Chiò, A. et al. ALS phenotype is influenced by age, sex, and genetics. _Neurology_ 94, e802–e810
(2020). PubMed Google Scholar * Cervetto, C., Frattaroli, D., Maura, G. & Marcoli, M. Motor neuron dysfunction in a mouse model of ALS: gender-dependent effect of P2X7 antagonism.
_Toxicology_ 311, 69–77 (2013). CAS PubMed Google Scholar * Suzuki, M. et al. Sexual dimorphism in disease onset and progression of a rat model of ALS. _Amyotroph. Lateral Scler._ 8,
20–25 (2007). PubMed Google Scholar * Oliván, S. et al. Comparative study of behavioural tests in the SOD1G93A mouse model of amyotrophic lateral sclerosis. _Exp. Anim._ 64, 147–153
(2015). PubMed Google Scholar * Pfohl, S. R., Halicek, M. T. & Mitchell, C. S. Characterization of the contribution of genetic background and gender to disease progression in the SOD1
G93A mouse model of amyotrophic lateral sclerosis: a meta-analysis. _J. Neuromuscul. Dis._ 2, 137–150 (2015). PubMed PubMed Central Google Scholar * Ohta, Y. et al. Sex-dependent effects
of chromogranin B P413L allelic variant as disease modifier in amyotrophic lateral sclerosis. _Hum. Mol. Genet._ 25, 4771–4786 (2016). CAS PubMed PubMed Central Google Scholar * Stam, N.
C. et al. Sex-specific behavioural effects of environmental enrichment in a transgenic mouse model of amyotrophic lateral sclerosis. _Eur. J. Neurosci._ 28, 717–723 (2008). PubMed Google
Scholar * Heiman-Patterson, T. D. et al. Background and gender effects on survival in the TgN(SOD1-G93A)1Gur mouse model of ALS. _J. Neurol. Sci._ 236, 1–7 (2005). CAS PubMed Google
Scholar * Urushitani, M. et al. Chromogranin-mediated secretion of mutant superoxide dismutase proteins linked to amyotrophic lateral sclerosis. _Nat. Neurosci._ 9, 108–118 (2006). CAS
PubMed Google Scholar * Gros-Louis, F. et al. Chromogranin B P413L variant as risk factor and modifier of disease onset for amyotrophic lateral sclerosis. _Proc. Natl Acad. Sci. USA_ 106,
21777–21782 (2009). CAS PubMed PubMed Central Google Scholar * Deng, H.-X. et al. Mutations in UBQLN2 cause dominant X-linked juvenile and adult-onset ALS and ALS/dementia. _Nature_ 477,
211–215 (2011). CAS PubMed PubMed Central Google Scholar * Renaud, L., Picher-Martel, V., Codron, P. & Julien, J. P. Key role of UBQLN2 in pathogenesis of amyotrophic lateral
sclerosis and frontotemporal dementia. _Acta Neuropathol. Commun._ 7, 103 (2019). PubMed PubMed Central Google Scholar * Chua, J. P., De Calbiac, H., Kabashi, E. & Barmada, S. J.
Autophagy and ALS: mechanistic insights and therapeutic implications. _Autophagy_ 18, 254–282 (2022). CAS PubMed Google Scholar * Lin, B. C., Higgins, N. R., Phung, T. H. & Monteiro,
M. J. UBQLN proteins in health and disease with a focus on UBQLN2 in ALS/FTD. _FEBS J._ 289, 6132–6153 (2022). CAS PubMed Google Scholar * Higgins, N., Lin, B. & Monteiro, M. J. Lou
Gehrig’s disease (ALS): UBQLN2 mutations strike out of phase. _Structure_ 27, 879–881 (2019). CAS PubMed PubMed Central Google Scholar * Vengoechea, J., David, M. P., Yaghi, S. R.,
Carpenter, L. & Rudnicki, S. A. Clinical variability and female penetrance in X-linked familial FTD/ALS caused by a P506S mutation in UBQLN2. _Amyotroph. Lateral Scler. Frontotemporal
Degener._ 14, 615–619 (2013). CAS PubMed Google Scholar * Gkazi, S. A. et al. Striking phenotypic variation in a family with the P506S UBQLN2 mutation including amyotrophic lateral
sclerosis, spastic paraplegia, and frontotemporal dementia. _Neurobiol. Aging_ 73, 229.e5–229.e9 (2019). CAS PubMed Google Scholar * Alexander, E. J. et al. Ubiquilin 2 modulates
ALS/FTD-linked FUS-RNA complex dynamics and stress granule formation. _Proc. Natl Acad. Sci. USA_ 115, E11485–E11494 (2018). CAS PubMed PubMed Central Google Scholar * Dao, T. P. et al.
Ubiquitin modulates liquid-liquid phase separation of UBQLN2 via disruption of multivalent interactions. _Mol. Cell_ 69, 965–978.e6 (2018). CAS PubMed PubMed Central Google Scholar *
Gilpin, K. M., Chang, L. & Monteiro, M. J. ALS-linked mutations in ubiquilin-2 or hnRNPA1 reduce interaction between ubiquilin-2 and hnRNPA1. _Hum. Mol. Genet._ 24, 2565–2577 (2015). CAS
PubMed Google Scholar * Picher-Martel, V., Dutta, K., Phaneuf, D., Sobue, G. & Julien, J. P. Ubiquilin-2 drives NF-κB activity and cytosolic TDP-43 aggregation in neuronal cells.
_Mol. Brain_ 8, 71 (2015). PubMed PubMed Central Google Scholar * Picher-Martel, V., Renaud, L., Bareil, C. & Julien, J. P. Neuronal expression of UBQLN2P497H exacerbates TDP-43
pathology in TDP-43G348C mice through interaction with ubiquitin. _Mol. Neurobiol._ 56, 4680–4696 (2019). CAS PubMed Google Scholar * Malik, A. M. & Barmada, S. J. Matrin 3 in
neuromuscular disease: physiology and pathophysiology. _JCI Insight_ 6, e143948 (2021). PubMed PubMed Central Google Scholar * Iradi, M. C. G. et al. Characterization of gene regulation
and protein interaction networks for Matrin 3 encoding mutations linked to amyotrophic lateral sclerosis and myopathy. _Sci. Rep._ 8, 4049 (2018). PubMed PubMed Central Google Scholar *
Johnson, J. O. et al. Mutations in the Matrin 3 gene cause familial amyotrophic lateral sclerosis. _Nat. Neurosci._ 17, 664–666 (2014). CAS PubMed PubMed Central Google Scholar * Cassel,
J. A. & Reitz, A. B. Ubiquilin-2 (UBQLN2) binds with high affinity to the C-terminal region of TDP-43 and modulates TDP-43 levels in H4 cells: characterization of inhibition by nucleic
acids and 4-aminoquinolines. _Biochim. Biophys. Acta_ 1834, 964–971 (2013). CAS PubMed PubMed Central Google Scholar * Strong, M. J. Revisiting the concept of amyotrophic lateral
sclerosis as a multisystems disorder of limited phenotypic expression. _Curr. Opin. Neurol._ 30, 599–607 (2017). PubMed Google Scholar * Oliva, M. et al. The impact of sex on gene
expression across human tissues. _Science_ 369, eaba3066 (2020). CAS PubMed PubMed Central Google Scholar * Ruigrok, A. N. V. et al. A meta-analysis of sex differences in human brain
structure. _Neurosci. Biobehav. Rev._ 39, 34–50 (2014). PubMed PubMed Central Google Scholar * Weis, S. et al. Sex classification by resting state brain connectivity. _Cereb. Cortex_ 30,
824–835 (2020). PubMed Google Scholar * Renga, V. Brain connectivity and network analysis in amyotrophic lateral sclerosis. _Neurol. Res. Int._ 2022, 1838682 (2022). PubMed PubMed Central
Google Scholar * Bede, P., Elamin, M., Byrne, S. & Hardiman, O. Sexual dimorphism in ALS: exploring gender-specific neuroimaging signatures. _Amyotroph. Lateral Scler. Front.
Degener._ 15, 235–243 (2014). Google Scholar * Pfefferbaum, A. et al. Age-related decline in brain white matter anisotropy measured with spatially corrected echo-planar diffusion tensor
imaging. _Magn. Reson. Med._ 44, 259–268 (2000). CAS PubMed Google Scholar * Trojsi, F. et al. Between-sex variability of resting state functional brain networks in amyotrophic lateral
sclerosis (ALS). _J. Neural Transm._ 128, 1881–1897 (2021). PubMed Google Scholar * Workman, M. J. et al. Large-scale differentiation of iPSC-derived motor neurons from ALS and control
subjects. _Neuron_ 111, 1191–1204.e5 (2023). CAS PubMed PubMed Central Google Scholar * Stoklund Dittlau, K. & Freude, K. Astrocytes: the stars in neurodegeneration? _Biomolecules_
14, 289 (2024). CAS PubMed PubMed Central Google Scholar * Xie, M., Pallegar, P. N., Parusel, S., Nguyen, A. T. & Wu, L. J. Regulation of cortical hyperexcitability in amyotrophic
lateral sclerosis: focusing on glial mechanisms. _Mol. Neurodegener._ 18, 75 (2023). PubMed PubMed Central Google Scholar * Yamanaka, K. et al. Astrocytes as determinants of disease
progression in inherited amyotrophic lateral sclerosis. _Nat. Neurosci._ 11, 251–253 (2008). CAS PubMed PubMed Central Google Scholar * Boillée, S. et al. Onset and progression in
inherited ALS determined by motor neurons and microglia. _Science_ 312, 1389–1392 (2006). PubMed Google Scholar * Clement, A. M. et al. Wild-type nonneuronal cells extend survival of SOD1
mutant motor neurons in ALS mice. _Science_ 302, 113–117 (2003). CAS PubMed Google Scholar * Yamanaka, K. et al. Mutant SOD1 in cell types other than motor neurons and oligodendrocytes
accelerates onset of disease in ALS mice. _Proc. Natl Acad. Sci. USA_ 105, 7594–7599 (2008). CAS PubMed PubMed Central Google Scholar * Amateau, S. K. & McCarthy, M. M. Sexual
differentiation of astrocyte morphology in the developing rat preoptic area. _J. Neuroendocrinol._ 14, 904–910 (2002). CAS PubMed Google Scholar * Arias, C. et al. Sex and estrous
cycle-dependent differences in glial fibrillary acidic protein immunoreactivity in the adult rat hippocampus. _Horm. Behav._ 55, 257–263 (2009). CAS PubMed Google Scholar * Collado, P.,
Beyer, C., Hutchison, J. B. & Holman, S. D. Hypothalamic distribution of astrocytes is gender-related in Mongolian gerbils. _Neurosci. Lett._ 184, 86–89 (1995). CAS PubMed Google
Scholar * Conejo, N. M. et al. Influence of gonadal steroids on the glial fibrillary acidic protein‐immunoreactive astrocyte population in young rat hippocampus. _J. Neurosci. Res._ 79,
488–494 (2005). CAS PubMed Google Scholar * Garcia-Segura, L. M., Dueñas, M., Busiguina, S., Naftolin, F. & Chowen, J. A. Gonadal hormone regulation of neuronal-glial interactions in
the developing neuroendocrine hypothalamus. _J. Steroid Biochem. Mol. Biol._ 53, 293–298 (1995). CAS PubMed Google Scholar * Garcia-Segura, L. M. et al. The distribution of glial
fibrillary acidic protein in the adult rat brain is influenced by the neonatal levels of sex steroids. _Brain Res._ 456, 357–363 (1988). CAS PubMed Google Scholar * Kuo, J., Hamid, N.,
Bondar, G., Prossnitz, E. R. & Micevych, P. Membrane estrogen receptors stimulate intracellular calcium release and progesterone synthesis in hypothalamic astrocytes. _J. Neurosci._ 30,
12950–12957 (2010). CAS PubMed PubMed Central Google Scholar * Rasia-Filho, A. A., Xavier, L. L., dos Santos, P., Gehlen, G. & Achaval, M. Glial fibrillary acidic protein
immunodetection and immunoreactivity in the anterior and posterior medial amygdala of male and female rats. _Brain Res. Bull._ 58, 67–75 (2002). CAS PubMed Google Scholar * Suárez, I.,
Bodega, G., Rubio, M. & Fernández, B. Sexual dimorphism in the hamster cerebellum demonstrated by glial fibrillary acidic protein (GFAP) and vimentin immunoreactivity. _Glia_ 5, 10–16
(1992). PubMed Google Scholar * Suárez, I., Bodega, G., Rubio, M. & Fernandez, B. Sexual dimorphism in the distribution of glial fibrillary acidic protein in the supraoptic nucleus of
the hamster. _J. Anat._ 178, 79–82 (1991). PubMed PubMed Central Google Scholar * Dion-Albert, L. et al. Sex differences in the blood–brain barrier: implications for mental health.
_Front. Neuroendocrinol._ 65, 100989 (2022). CAS PubMed Google Scholar * Weber, C. M. & Clyne, A. M. Sex differences in the blood–brain barrier and neurodegenerative diseases. _APL
Bioeng_. 5, 011509 (2021). CAS PubMed PubMed Central Google Scholar * Liu, M., Hurn, P. D., Roselli, C. E. & Alkayed, N. J. Role of P450 aromatase in sex-specific astrocytic cell
death. _J. Cereb. Blood Flow Metab._ 27, 135–141 (2007). CAS PubMed Google Scholar * Humphrey, J. et al. Integrative transcriptomic analysis of the amyotrophic lateral sclerosis spinal
cord implicates glial activation and suggests new risk genes. _Nat. Neurosci._ 26, 150–162 (2023). CAS PubMed Google Scholar * Nave, K. A., Asadollahi, E. & Sasmita, A. Expanding the
function of oligodendrocytes to brain energy metabolism. _Curr. Opin. Neurobiol._ 83, 102782 (2023). CAS PubMed Google Scholar * Yasuda, K. et al. Sex-specific differences in
transcriptomic profiles and cellular characteristics of oligodendrocyte precursor cells. _Stem Cell Res._ 46, 101866 (2020). CAS PubMed Google Scholar * Villa, A., Della Torre, S. &
Maggi, A. Sexual differentiation of microglia. _Front. Neuroendocrinol._ 52, 156–164 (2019). PubMed Google Scholar * Kodama, L. & Gan, L. Do microglial sex differences contribute to
sex differences in neurodegenerative diseases? _Trends Mol. Med._ 25, 741–749 (2019). PubMed Google Scholar * Sala Frigerio, C. et al. The major risk factors for Alzheimer’s disease: age,
sex, and genes modulate the microglia response to Aβ plaques. _Cell Rep._ 27, 1293–1306.e6 (2019). CAS PubMed Google Scholar * Gomes, L. C. et al. Multiomic ALS signatures highlight sex
differences and molecular subclusters and identify the MAPK pathway as therapeutic target. Preprint at _bioRxiv_ https://doi.org/10.1101/2023.08.14.553180 (2023). * Abbott, N. J.
Astrocyte–endothelial interactions and blood–brain barrier permeability. _J. Anat._ 200, 629–638 (2002). CAS PubMed PubMed Central Google Scholar * Daneman, R. & Prat, A. The
blood–brain barrier. _Cold Spring Harb. Perspect. Biol._ 7, a020412 (2015). PubMed PubMed Central Google Scholar * Muldoon, L. L. et al. Immunologic privilege in the central nervous
system and the blood–brain barrier. _J. Cereb. Blood Flow Metab._ 33, 13–21 (2013). CAS PubMed Google Scholar * Prockop, L. D., Naidu, K. A., Binard, J. E. & Ransohoff, J. Selective
permeability of [3H]-D-mannitol and [14C]-carboxyl-inulin across the blood-brain barrier and blood-spinal cord barrier in the rabbit. _J. Spinal Cord Med._ 18, 221–226 (1995). CAS PubMed
Google Scholar * Pan, W., Banks, W. A. & Kastin, A. J. Permeability of the blood-brain and blood-spinal cord barriers to interferons. _J. Neuroimmunol._ 76, 105–111 (1997). CAS PubMed
Google Scholar * Winkler, E. A. et al. Blood-spinal cord barrier disruption contributes to early motor-neuron degeneration in ALS-model mice. _Proc. Natl Acad. Sci. USA_ 111, E1035–E1042
(2014). CAS PubMed PubMed Central Google Scholar * Yoon, H., Walters, G., Paulsen, A. R. & Scarisbrick, I. A. Astrocyte heterogeneity across the brain and spinal cord occurs
developmentally, in adulthood and in response to demyelination. _PLoS ONE_ 12, e0180697 (2017). PubMed PubMed Central Google Scholar * Garbuzova-Davis, S. et al. Ultrastructure of
blood-brain barrier and blood-spinal cord barrier in SOD1 mice modeling ALS. _Brain Res._ 1157, 126–137 (2007). CAS PubMed Google Scholar * Zhong, Z. et al. ALS-causing SOD1 mutants
generate vascular changes prior to motor neuron degeneration. _Nat. Neurosci._ 11, 420–422 (2008). CAS PubMed PubMed Central Google Scholar * Miyazaki, K. et al. Disruption of
neurovascular unit prior to motor neuron degeneration in amyotrophic lateral sclerosis. _J. Neurosci. Res._ 89, 718–728 (2011). CAS PubMed Google Scholar * Steinruecke, M. et al.
Blood-CNS barrier dysfunction in amyotrophic lateral sclerosis: proposed mechanisms and clinical implications. _J. Cereb. Blood Flow Metab._ 43, 642–654 (2023). CAS PubMed PubMed Central
Google Scholar * Garbuzova-Davis, S. et al. Amyotrophic lateral sclerosis: a neurovascular disease. _Brain Res._ 1398, 113–25 (2011). CAS PubMed Google Scholar * Donnenfeld, H., Kascsak,
R. J. & Bartfeld, H. Deposits of IgG and C3 in the spinal cord and motor cortex of ALS patients. _J. Neuroimmunol._ 6, 51–57 (1984). CAS PubMed Google Scholar * Henkel, J. S. et al.
Presence of dendritic cells, MCP-1, and activated microglia/macrophages in amyotrophic lateral sclerosis spinal cord tissue. _Ann. Neurol._ 55, 221–235 (2004). CAS PubMed Google Scholar *
Yamadera, M. et al. Microvascular disturbance with decreased pericyte coverage is prominent in the ventral horn of patients with amyotrophic lateral sclerosis. _Amyotroph. Lateral Scler.
Frontotemporal Degener._ 16, 393–401 (2015). PubMed Google Scholar * Garbuzova-Davis, S. et al. Impaired blood-brain/spinal cord barrier in ALS patients. _Brain Res._ 1469, 114–128 (2012).
CAS PubMed Google Scholar * Dalla, C., Pavlidi, P., Sakelliadou, D. G., Grammatikopoulou, T. & Kokras, N. Sex differences in blood–brain barrier transport of psychotropic drugs.
_Front. Behav. Neurosci._ 16, 844916 (2022). CAS PubMed PubMed Central Google Scholar * Alarcan, H. et al. Implication of central nervous system barrier impairment in amyotrophic lateral
sclerosis: gender-related difference in patients. _Int. J. Mol. Sci._ 24, 11196 (2023). CAS PubMed PubMed Central Google Scholar * Hakim, M. A., Chum, P. P., Buchholz, J. N. &
Behringer, E. J. Aging alters cerebrovascular endothelial GPCR and K+ channel function: divergent role of biological sex. _J. Gerontol. A_ 75, 2064–2073 (2020). CAS Google Scholar *
Bauersachs, J. et al. Nitric oxide attenuates the release of endothelium-derived hyperpolarizing factor. _Circulation_ 94, 3341–3347 (1996). CAS PubMed Google Scholar * Min, J.
17β-Estradiol-stimulated eNOS gene transcriptional activation is regulated through the estrogen-responsive element in eNOS promoter. _Biotechnol. Bioprocess. Eng._ 12, 446–449 (2007). CAS
Google Scholar * Zhang, L., Papadopoulos, P. & Hamel, E. Endothelial TRPV4 channels mediate dilation of cerebral arteries: impairment and recovery in cerebrovascular pathologies related
to Alzheimer’s disease. _Br. J. Pharmacol._ 170, 661–670 (2013). CAS PubMed PubMed Central Google Scholar * Marrelli, S. P., O’Neil, R. G., Brown, R. C. & Bryan, R. M. PLA 2 and
TRPV4 channels regulate endothelial calcium in cerebral arteries. _Am. J. Physiol. Circ. Physiol._ 292, H1390–H1397 (2007). CAS Google Scholar * Longden, T. A., Hill-Eubanks, D. C. &
Nelson, M. T. Ion channel networks in the control of cerebral blood flow. _J. Cereb. Blood Flow Metab._ 36, 492–512 (2016). CAS PubMed Google Scholar * Stoica, R. et al. Ca2+ homeostasis
in brain microvascular endothelial cells. _Int. Rev. Cell Mol. Biol._ 362, 55–110 (2021). CAS PubMed Google Scholar * Gur, R. C. et al. Sex differences in regional cerebral glucose
metabolism during a resting state. _Science_ 267, 528–531 (1995). CAS PubMed Google Scholar * Lerskiatiphanich, T., Marallag, J. & Lee, J. Glucose metabolism in amyotrophic lateral
sclerosis: it is bitter-sweet. _Neural Regen. Res._ 17, 1975 (2022). CAS PubMed PubMed Central Google Scholar * Tefera, T. W., Steyn, F. J., Ngo, S. T. & Borges, K. CNS glucose
metabolism in amyotrophic lateral sclerosis: a therapeutic target? _Cell Biosci._ 11, 14 (2021). CAS PubMed PubMed Central Google Scholar * Clyne, A. M. Endothelial response to glucose:
dysfunction, metabolism, and transport. _Biochem. Soc. Trans._ 49, 313–325 (2021). CAS PubMed PubMed Central Google Scholar * Ahmed, R. M., Steyn, F. & Dupuis, L. Hypothalamus and
weight loss in amyotrophic lateral sclerosis. _Handb. Clin. Neurol._ 180, 327–338 (2021). PubMed Google Scholar * Kawachi, T. et al. Gender differences in cerebral glucose metabolism: a
PET study. _J. Neurol. Sci._ 199, 79–83 (2002). CAS PubMed Google Scholar * Mukai, E., Fujimoto, S. & Inagaki, N. Role of reactive oxygen species in glucose metabolism disorder in
diabetic pancreatic β-cells. _Biomolecules_ 12, 1228 (2022). CAS PubMed PubMed Central Google Scholar * Ventura-Clapier, R. et al. Mitochondria: a central target for sex differences in
pathologies. _Clin. Sci._ 131, 803–822 (2017). CAS Google Scholar * Cacabelos, D. et al. Early and gender-specific differences in spinal cord mitochondrial function and oxidative stress
markers in a mouse model of ALS. _Acta Neuropathol. Commun._ 4, 3 (2016). PubMed PubMed Central Google Scholar * Damiano, M. et al. Neural mitochondrial Ca2+ capacity impairment precedes
the onset of motor symptoms in G93A Cu/Zn-superoxide dismutase mutant mice. _J. Neurochem._ 96, 1349–1361 (2006). CAS PubMed Google Scholar * Lalancette-Hebert, M., Sharma, A.,
Lyashchenko, A. K. & Shneider, N. A. Gamma motor neurons survive and exacerbate alpha motor neuron degeneration in ALS. _Proc. Natl Acad. Sci. USA_ 113, E8316–E8325 (2016). CAS PubMed
PubMed Central Google Scholar * Yadav, A. et al. A cellular taxonomy of the adult human spinal cord. _Neuron_ 111, 328–344.e7 (2023). CAS PubMed PubMed Central Google Scholar *
Pontifex, C. S., Zaman, M., Fanganiello, R. D., Shutt, T. E. & Pfeffer, G. Valosin-containing protein (VCP): a review of its diverse molecular functions and clinical phenotypes. _Int. J.
Mol. Sci._ 25, 5633 (2024). CAS PubMed PubMed Central Google Scholar * Inglis, J. G. & Gabriel, D. A. Sex differences in the modulation of the motor unit discharge rate leads to
reduced force steadiness. _Appl. Physiol. Nutr. Metab._ 46, 1065–1072 (2021). CAS PubMed Google Scholar * Taylor, C. A., Kopicko, B. H., Negro, F. & Thompson, C. K. Sex differences in
the detection of motor unit action potentials identified using high-density surface electromyography. _J. Electromyogr. Kinesiol._ 65, 102675 (2022). PubMed PubMed Central Google Scholar
* Fishman, R. B. & Breedlove, S. M. Local perineal implants of anti-androgen block masculinization of the spinal nucleus of the bulbocavernosus. _Brain Res. Dev. Brain Res._ 70,
283–286 (1992). CAS PubMed Google Scholar * Omar, A., Marwaha, K. & Bollu, P. C. _Physiology, Neuromuscular Junction_ (StatPearls, 2024). * Verma, S. et al. Neuromuscular junction
dysfunction in amyotrophic lateral sclerosis. _Mol. Neurobiol._ 59, 1502–1527 (2022). CAS PubMed Google Scholar * Armon, C. & Brandstater, M. E. Motor unit number estimate-based rates
of progression of ALS predict patient survival. _Muscle Nerve_ 22, 1571–1575 (1999). CAS PubMed Google Scholar * Martineau, É., Di Polo, A., Vande Velde, C. & Robitaille, R.
Sex-specific differences in motor-unit remodeling in a mouse model of ALS. _eNeuro_ 7, https://doi.org/10.1523/ENEURO.0388-19.2020 (2020). * Shefner, J. M. et al. Skeletal muscle in
amyotrophic lateral sclerosis. _Brain_ 146, 4425–4436 (2023). PubMed PubMed Central Google Scholar * Badu-Mensah, A., Guo, X., Nimbalkar, S., Cai, Y. & Hickman, J. J. ALS mutations in
both human skeletal muscle and motoneurons differentially affects neuromuscular junction integrity and function. _Biomaterials_ 289, 121752 (2022). CAS PubMed Google Scholar *
Dobrowolny, G. et al. Muscle expression of SOD1G93A triggers the dismantlement of neuromuscular junction via PKC-theta. _Antioxid. Redox Signal._ 28, 1105–1119 (2018). CAS PubMed Google
Scholar * Steyn, F. J. et al. Altered skeletal muscle glucose-fatty acid flux in amyotrophic lateral sclerosis. _Brain Commun._ 2, fcaa154 (2020). PubMed PubMed Central Google Scholar *
Palamiuc, L. et al. A metabolic switch toward lipid use in glycolytic muscle is an early pathologic event in a mouse model of amyotrophic lateral sclerosis. _EMBO Mol. Med._ 7, 526–546
(2015). CAS PubMed PubMed Central Google Scholar * Haizlip, K. M., Harrison, B. C. & Leinwand, L. A. Sex-based differences in skeletal muscle kinetics and fiber-type composition.
_Physiology_ 30, 30–39 (2015). CAS PubMed PubMed Central Google Scholar * van Wessel, T., de Haan, A., van der Laarse, W. J. & Jaspers, R. T. The muscle fiber type–fiber size
paradox: hypertrophy or oxidative metabolism? _Eur. J. Appl. Physiol._ 110, 665–694 (2010). PubMed PubMed Central Google Scholar * Anderson, E. J. & Neufer, P. D. Type II skeletal
myofibers possess unique properties that potentiate mitochondrial H2O2 generation. _Am. J. Physiol. Cell Physiol._ 290, C844–C851 (2006). CAS PubMed Google Scholar * Pegoraro, V., Merico,
A. & Angelini, C. Micro-RNAs in ALS muscle: differences in gender, age at onset and disease duration. _J. Neurol. Sci._ 380, 58–63 (2017). CAS PubMed PubMed Central Google Scholar *
Gomes, B. C. et al. Differential expression of miRNAs in amyotrophic lateral sclerosis patients. _Mol. Neurobiol._ 60, 7104–7117 (2023). CAS PubMed PubMed Central Google Scholar *
Zhang, Z., Jin, A. & Yan, D. MicroRNA-206 contributes to the progression of steroid-induced avascular necrosis of the femoral head by inducing osteoblast apoptosis by suppressing
programmed cell death 4. _Mol. Med. Rep._ 17, 801–808 (2018). CAS PubMed Google Scholar * Casola, I. et al. Circulating myomiRs in muscle denervation: from surgical to ALS pathological
condition. _Cells_ 10, 2043 (2021). CAS PubMed PubMed Central Google Scholar * Abdelhak, A. et al. In vivo assessment of retinal vessel pathology in amyotrophic lateral sclerosis. _J.
Neurol._ 265, 949–953 (2018). CAS PubMed Google Scholar * Kolde, G., Bachus, R. & Ludolph, A. Skin involvement in amyotrophic lateral sclerosis. _Lancet_ 347, 1226–1227 (1996). CAS
PubMed Google Scholar * Buckley, A. F. & Bossen, E. H. Skeletal muscle microvasculature in the diagnosis of neuromuscular disease. _J. Neuropathol. Exp. Neurol._ 72, 906–918 (2013).
PubMed Google Scholar * Saul, J. et al. Global alterations to the choroid plexus blood-CSF barrier in amyotrophic lateral sclerosis. _Acta Neuropathol. Commun._ 8, 92 (2020). CAS PubMed
PubMed Central Google Scholar * Iadecola, C. The pathobiology of vascular dementia. _Neuron_ 80, 844–866 (2013). CAS PubMed Google Scholar * Iadecola, C. Neurovascular regulation in the
normal brain and in Alzheimer’s disease. _Nat. Rev. Neurosci._ 5, 347–360 (2004). CAS PubMed Google Scholar * Zlokovic, B. V. Neurovascular pathways to neurodegeneration in Alzheimer’s
disease and other disorders. _Nat. Rev. Neurosci._ 12, 723–738 (2011). CAS PubMed PubMed Central Google Scholar * Rosenbohm, A. et al. Cardiac findings in amyotrophic lateral sclerosis:
a magnetic resonance imaging study. _Front. Neurol._ 8, 479 (2017). PubMed PubMed Central Google Scholar * Xu, K., Ji, H. & Hu, N. Cardiovascular comorbidities in amyotrophic lateral
sclerosis: a systematic review. _J. Clin. Neurosci._ 96, 43–49 (2022). PubMed Google Scholar * Hu, N. & Ji, H. Medications on hypertension, hyperlipidemia, diabetes, and risk of
amyotrophic lateral sclerosis: a systematic review and meta-analysis. _Neurol. Sci._ 43, 5189–5199 (2022). PubMed Google Scholar * St. Pierre, S. R., Peirlinck, M. & Kuhl, E. Sex
matters: a comprehensive comparison of female and male hearts. _Front. Physiol._ 13, 831179 (2022). Google Scholar * Gur, R. C. et al. Sex and handedness differences in cerebral blood flow
during rest and cognitive activity. _Science_ 217, 659–661 (1982). CAS PubMed Google Scholar * Rodriguez, G., Warkentin, S., Risberg, J. & Rosadini, G. Sex differences in regional
cerebral blood flow. _J. Cereb. Blood Flow Metab._ 8, 783–789 (1988). CAS PubMed Google Scholar * Satterthwaite, T. D. et al. Impact of puberty on the evolution of cerebral perfusion
during adolescence. _Proc. Natl Acad. Sci. USA_ 111, 8643–8648 (2014). CAS PubMed PubMed Central Google Scholar * Tontisirin, N. et al. Early childhood gender differences in anterior and
posterior cerebral blood flow velocity and autoregulation. _Pediatrics_ 119, e610–e615 (2007). PubMed Google Scholar * Monteiro, J. N. in _Essentials of Neuroanesthesia_ (ed. Prabhakar,
H.) 815–825 (Elsevier, 2017). * Deegan, B. M. et al. Elderly women regulate brain blood flow better than men do. _Stroke_ 42, 1988–1993 (2011). PubMed PubMed Central Google Scholar *
Vavilala, M. S. et al. Gender differences in cerebral blood flow velocity and autoregulation between the anterior and posterior circulations in healthy children. _Pediatr. Res._ 58, 574–578
(2005). PubMed PubMed Central Google Scholar * Schreiber, S. et al. Brain vascular health in ALS is mediated through motor cortex microvascular integrity. _Cells_ 12, 957 (2023). CAS
PubMed PubMed Central Google Scholar * Chen, Y. et al. Difference in leukocyte composition between women before and after menopausal age, and distinct sexual dimorphism. _PLoS ONE_ 11,
e0162953 (2016). PubMed PubMed Central Google Scholar * Murdock, B. J., Goutman, S. A., Boss, J., Kim, S. & Feldman, E. L. Amyotrophic lateral sclerosis survival associates with
neutrophils in a sex-specific manner. _Neurol. Neuroimmunol. Neuroinflamm__._ 8, e953 (2021). PubMed PubMed Central Google Scholar * Lehman, H. K. & Segal, B. H. The role of
neutrophils in host defense and disease. _J. Allergy Clin. Immunol._ 145, 1535–1544 (2020). CAS PubMed PubMed Central Google Scholar * Janeway, C. A. How the immune system protects the
host from infection. _Microbes Infect._ 3, 1167–1171 (2001). CAS PubMed Google Scholar * Bongen, E. et al. Sex differences in the blood transcriptome identify robust changes in immune
cell proportions with aging and influenza infection. _Cell Rep._ 29, 1961–1973.e4 (2019). CAS PubMed PubMed Central Google Scholar * McCombe, P., Greer, J. & Mackay, I. Sexual
dimorphism in autoimmune disease. _Curr. Mol. Med._ 9, 1058–1079 (2009). CAS PubMed Google Scholar * Santiago, J. A., Quinn, J. P. & Potashkin, J. A. Network analysis identifies
sex-specific gene expression changes in blood of amyotrophic lateral sclerosis patients. _Int. J. Mol. Sci._ 22, 7150 (2021). CAS PubMed PubMed Central Google Scholar * Beers, D. R. et
al. ALS patients’ regulatory T lymphocytes are dysfunctional, and correlate with disease progression rate and severity. _JCI Insight_ 2, e89530 (2017). PubMed PubMed Central Google Scholar
* Beers, D. R. & Appel, S. H. Immune dysregulation in amyotrophic lateral sclerosis: mechanisms and emerging therapies. _Lancet Neurol._ 18, 211–220 (2019). CAS PubMed Google Scholar
* Zhao, W., Beers, D. R., Liao, B., Henkel, J. S. & Appel, S. H. Regulatory T lymphocytes from ALS mice suppress microglia and effector T lymphocytes through different
cytokine-mediated mechanisms. _Neurobiol. Dis._ 48, 418–428 (2012). CAS PubMed PubMed Central Google Scholar * Beckmann, L. et al. Regulatory T cells contribute to sexual dimorphism in
neonatal hypoxic-ischemic brain injury. _Stroke_ 53, 381–390 (2022). CAS PubMed PubMed Central Google Scholar * US National Library of Medicine_._ _ClinicalTrials.gov_
https://classic.clinicaltrials.gov/ct2/show/NCT03241784 (2018). * US National Library of Medicine. _ClinicalTrials.gov_ https://clinicaltrials.gov/ct2/show/NCT04055623 (2021). * Boddy, S. L.
et al. The gut microbiome: a key player in the complexity of amyotrophic lateral sclerosis (ALS). _BMC Med._ 19, 13 (2021). PubMed PubMed Central Google Scholar * Sun, J., Huang, T.,
Debelius, J. W. & Fang, F. Gut microbiome and amyotrophic lateral sclerosis: a systematic review of current evidence. _J. Intern. Med._ 290, 758–788 (2021). PubMed Google Scholar *
Mercedes Prudencio. The effects of ALS on the digestive system. _Target ALS_ https://www.targetals.org/2022/08/25/the-effects-of-als-on-the-digestive-system/ (2015). * Toepfer, C.,
Folwaczny, A., Klauser & RL, M. Gastrointestinal dysfunction in amyotrophic lateral sclerosis. _Amyotroph. Lateral Scler. Other Mot. Neuron Disord._ 1, 15–19 (2000). Google Scholar *
Kim, Y. S., Unno, T., Kim, B. Y. & Park, M. S. Sex differences in gut microbiota. _World J. Mens Health_ 38, 48 (2020). PubMed Google Scholar * Schroeder, B. O. & Bäckhed, F.
Signals from the gut microbiota to distant organs in physiology and disease. _Nat. Med._ 22, 1079–1089 (2016). CAS PubMed Google Scholar * Martin, C. R., Osadchiy, V., Kalani, A. &
Mayer, E. A. The brain-gut-microbiome axis. _Cell. Mol. Gastroenterol. Hepatol._ 6, 133–148 (2018). PubMed PubMed Central Google Scholar * Thaiss, C. A., Zmora, N., Levy, M. & Elinav,
E. The microbiome and innate immunity. _Nature_ 535, 65–74 (2016). CAS PubMed Google Scholar * Wang, J., Zhu, N., Su, X., Gao, Y. & Yang, R. Gut-microbiota-derived metabolites
maintain gut and systemic immune homeostasis. _Cells_ 12, 793 (2023). CAS PubMed PubMed Central Google Scholar * Cryan, J. F. et al. The microbiota-gut-brain axis. _Physiol. Rev._ 99,
1877–2013 (2019). CAS PubMed Google Scholar * Rizzetto, L., Fava, F., Tuohy, K. M. & Selmi, C. Connecting the immune system, systemic chronic inflammation and the gut microbiome: the
role of sex. _J. Autoimmun._ 92, 12–34 (2018). CAS PubMed Google Scholar * Loh, J. S. et al. Microbiota-gut-brain axis and its therapeutic applications in neurodegenerative diseases.
_Signal Transduct. Target. Ther._ 9, 37 (2024). PubMed PubMed Central Google Scholar * Aburto, M. R. & Cryan, J. F. Gastrointestinal and brain barriers: unlocking gates of
communication across the microbiota-gut-brain axis. _Nat. Rev. Gastroenterol. Hepatol._ 21, 222–247 (2024). PubMed Google Scholar * Mazzini, L. et al. Potential role of gut microbiota in
ALS pathogenesis and possible novel therapeutic strategies. _J. Clin. Gastroenterol._ 52, S68–S70 (2018). CAS PubMed Google Scholar * Kim, H. S. et al. Gut- and oral-dysbiosis
differentially impact spinal- and bulbar-onset ALS, predicting ALS severity and potentially determining the location of disease onset. _BMC Neurol._ 22, 62 (2022). CAS PubMed PubMed
Central Google Scholar * Rowin, J., Xia, Y., Jung, B. & Sun, J. Gut inflammation and dysbiosis in human motor neuron disease. _Physiol. Rep._ 5, e13443 (2017). PubMed PubMed Central
Google Scholar * Blacher, E. et al. Potential roles of gut microbiome and metabolites in modulating ALS in mice. _Nature_ 572, 474–480 (2019). CAS PubMed Google Scholar * Wu, S., Yi, J.,
Zhang, Y., Zhou, J. & Sun, J. Leaky intestine and impaired microbiome in an amyotrophic lateral sclerosis mouse model. _Physiol. Rep._ 3, e12356 (2015). PubMed PubMed Central Google
Scholar * Zhang, Y. et al. Target intestinal microbiota to alleviate disease progression in amyotrophic lateral sclerosis. _Clin. Ther._ 39, 322–336 (2017). CAS PubMed PubMed Central
Google Scholar * Hatzipetros, T. et al. C57BL/6J congenic Prp-TDP43A315T mice develop progressive neurodegeneration in the myenteric plexus of the colon without exhibiting key features of
ALS. _Brain Res._ 1584, 59–72 (2014). CAS PubMed Google Scholar * Guo, K. et al. Gut microbiome correlates with plasma lipids in amyotrophic lateral sclerosis. _Brain_ 147, 665–679
(2023). Google Scholar * Popat, R. A. et al. Effect of reproductive factors and postmenopausal hormone use on the risk of amyotrophic lateral sclerosis. _Neuroepidemiology_ 27, 117–121
(2006). PubMed Google Scholar * Choi, C. I. et al. Effects of estrogen on lifespan and motor functions in female hSOD1 G93A transgenic mice. _J. Neurol. Sci._ 268, 40–47 (2008). CAS
PubMed Google Scholar * Gargiulo-Monachelli, G. et al. Circulating gonadal and adrenal steroids in amyotrophic lateral sclerosis: possible markers of susceptibility and outcome. _Horm.
Metab. Res._ 46, 433–439 (2014). CAS PubMed Google Scholar * Militello, A. et al. The serum level of free testosterone is reduced in amyotrophic lateral sclerosis. _J. Neurol. Sci._ 195,
67–70 (2002). CAS PubMed Google Scholar * Kim, H. J., Magranè, J., Starkov, A. A. & Manfredi, G. The mitochondrial calcium regulator cyclophilin D is an essential component of
oestrogen-mediated neuroprotection in amyotrophic lateral sclerosis. _Brain_ 135, 2865–2874 (2012). PubMed PubMed Central Google Scholar * Groeneveld, G. J. et al. Ovariectomy and
17β-estradiol modulate disease progression of a mouse model of ALS. _Brain Res._ 1021, 128–131 (2004). CAS PubMed Google Scholar * Yoo, Y. E. & Ko, C. P. Dihydrotestosterone
ameliorates degeneration in muscle, axons and motoneurons and improves motor function in amyotrophic lateral sclerosis model mice. _PLoS ONE_ 7, e37258 (2012). CAS PubMed PubMed Central
Google Scholar * McLeod, V. M. et al. Androgen receptor antagonism accelerates disease onset in the SOD1 G93A mouse model of amyotrophic lateral sclerosis. _Br. J. Pharmacol._ 176,
2111–2130 (2019). CAS PubMed PubMed Central Google Scholar * Aggarwal, T. et al. Androgens affect muscle, motor neuron, and survival in a mouse model of SOD1-related amyotrophic lateral
sclerosis. _Neurobiol. Aging_ 35, 1929–1938 (2014). CAS PubMed Google Scholar * Brannvall, K. Estrogen-receptor-dependent regulation of neural stem cell proliferation and differentiation.
_Mol. Cell. Neurosci._ 21, 512–520 (2002). CAS PubMed Google Scholar * Charalampopoulos, I., Remboutsika, E., Margioris, A. N. & Gravanis, A. Neurosteroids as modulators of
neurogenesis and neuronal survival. _Trends Endocrinol. Metab._ 19, 300–307 (2008). CAS PubMed Google Scholar * Garcia-Segura, L. M. & Melcangi, R. C. Steroids and glial cell
function. _Glia_ 54, 485–498 (2006). PubMed Google Scholar * Garcia-Segura, L. M., Diz-Chaves, Y., Perez-Martin, M. & Darnaudéry, M. Estradiol, insulin-like growth factor-I and brain
aging. _Psychoneuroendocrinology_ 32, S57–S61 (2007). CAS PubMed Google Scholar * Brann, D. W., Dhandapani, K., Wakade, C., Mahesh, V. B. & Khan, M. M. Neurotrophic and
neuroprotective actions of estrogen: basic mechanisms and clinical implications. _Steroids_ 72, 381–405 (2007). CAS PubMed PubMed Central Google Scholar * Barron, A. M., Fuller, S. J.,
Verdile, G. & Martins, R. N. Reproductive hormones modulate oxidative stress in Alzheimer’s disease. _Antioxid. Redox Signal._ 8, 2047–2059 (2006). CAS PubMed Google Scholar * Prokai,
L. & Simpkins, J. W. Structure–nongenomic neuroprotection relationship of estrogens and estrogen-derived compounds. _Pharmacol. Ther._ 114, 1–12 (2007). CAS PubMed PubMed Central
Google Scholar * Gayard, M. et al. AMPK alpha 1-induced RhoA phosphorylation mediates vasoprotective effect of estradiol. _Arterioscler. Thromb. Vasc. Biol._ 31, 2634–2642 (2011). CAS
PubMed Google Scholar * Cunha-Oliveira, T. et al. Oxidative stress in amyotrophic lateral sclerosis: pathophysiology and opportunities for pharmacological intervention. _Oxid. Med. Cell.
Longev._ 2020, 5021694 (2020). PubMed PubMed Central Google Scholar * Kakaroubas, N., Brennan, S., Keon, M. & Saksena, N. K. Pathomechanisms of blood-brain barrier disruption in ALS.
_Neurosci. J._ 2019, 2537698 (2019). PubMed PubMed Central Google Scholar * Yan, L. et al. Effects of ovariectomy in an hSOD1-G93A transgenic mouse model of amyotrophic lateral sclerosis
(ALS). _Med. Sci. Monit._ 24, 678–686 (2018). CAS PubMed PubMed Central Google Scholar * Brinton, R. D., Yao, J., Yin, F., Mack, W. J. & Cadenas, E. Perimenopause as a neurological
transition state. _Nat. Rev. Endocrinol._ 11, 393–405 (2015). CAS PubMed PubMed Central Google Scholar * Zhao, L., Mao, Z., Woody, S. K. & Brinton, R. D. Sex differences in metabolic
aging of the brain: insights into female susceptibility to Alzheimer’s disease. _Neurobiol. Aging_ 42, 69–79 (2016). PubMed PubMed Central Google Scholar * Hammond, J. et al.
Testosterone-mediated neuroprotection through the androgen receptor in human primary neurons. _J. Neurochem._ 77, 1319–1326 (2001). CAS PubMed Google Scholar * Byers, J. S. et al.
Neuroprotective effects of testosterone on motoneuron and muscle morphology following spinal cord injury. _J. Comp. Neurol._ 520, 2683–2696 (2012). CAS PubMed PubMed Central Google
Scholar * Hamson, D. K. et al. Androgens increase survival of adult-born neurons in the dentate gyrus by an androgen receptor-dependent mechanism in male rats. _Endocrinology_ 154,
3294–3304 (2013). CAS PubMed Google Scholar * Hayes-Punzo, A. et al. Gonadectomy and dehydroepiandrosterone (DHEA) do not modulate disease progression in the G93A mutant SOD1 rat model of
amyotrophic lateral sclerosis. _Amyotroph. Lateral Scler._ 13, 311–314 (2012). CAS PubMed PubMed Central Google Scholar * Baulieu, E. Neurosteroids: a novel function of the brain.
_Psychoneuroendocrinology_ 23, 963–987 (1998). CAS PubMed Google Scholar * Lyraki, R. & Schedl, A. The sexually dimorphic adrenal cortex: implications for adrenal disease. _Int. J.
Mol. Sci._ 22, 4889 (2021). CAS PubMed PubMed Central Google Scholar * Katsuno, M. et al. Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and
bulbar muscular atrophy. _Neuron_ 35, 843–854 (2002). CAS PubMed Google Scholar * Ishihara, H., Kanda, F., Nishio, H., Sumino, K. & Chihara, K. Clinical features and skewed
X-chromosome inactivation in female carriers of X-linked recessive spinal and bulbar muscular atrophy. _J. Neurol._ 248, 856–860 (2001). CAS PubMed Google Scholar * Mariotti, C. et al.
Phenotypic manifestations associated with CAG-repeat expansion in the androgen receptor gene in male patients and heterozygous females: a clinical and molecular study of 30 families.
_Neuromuscul. Disord._ 10, 391–397 (2000). CAS PubMed Google Scholar * Schmidt, B. J., Greenberg, C. R., Allingham-Hawkins, D. J. & Spriggs, E. L. Expression of X-linked bulbospinal
muscular atrophy (Kennedy disease) in two homozygous women. _Neurology_ 59, 770–772 (2002). PubMed Google Scholar * Hashizume, A. et al. Efficacy and safety of leuprorelin acetate for
subjects with spinal and bulbar muscular atrophy: pooled analyses of two randomized-controlled trials. _J. Neurol._ 266, 1211–1221 (2019). CAS PubMed Google Scholar * Uhart, M., Chong,
R., Oswald, L., Lin, P. & Wand, G. Gender differences in hypothalamic–pituitary–adrenal (HPA) axis reactivity. _Psychoneuroendocrinology_ 31, 642–652 (2006). CAS PubMed Google Scholar
* Heck, A. L. & Handa, R. J. Sex differences in the hypothalamic–pituitary–adrenal axis’ response to stress: an important role for gonadal hormones. _Neuropsychopharmacology_ 44, 45–58
(2019). CAS PubMed Google Scholar * Patacchioli, F. R. et al. Adrenal dysregulation in amyotrophic lateral sclerosis. _J. Endocrinol. Invest._ 26, RC23–RC25 (2003). CAS PubMed Google
Scholar * Feneberg, E. et al. Multicenter evaluation of neurofilaments in early symptom onset amyotrophic lateral sclerosis. _Neurology_ 90, e22–e30 (2018). CAS PubMed Google Scholar *
Skillbäck, T. et al. Sex differences in CSF biomarkers for neurodegeneration and blood-brain barrier integrity. _Alzheimers Dement._ 13, e12141 (2021). Google Scholar * Gaiani, A. et al.
Diagnostic and prognostic biomarkers in amyotrophic lateral sclerosis. _JAMA Neurol._ 74, 525 (2017). PubMed PubMed Central Google Scholar * Verde, F. et al. Phenotypic correlates of
serum neurofilament light chain levels in amyotrophic lateral sclerosis. _Front. Aging Neurosci._ 15, 1132808 (2023). CAS PubMed PubMed Central Google Scholar * Fenton, A. et al.
Glomerular filtration rate: new age- and gender-specific reference ranges and thresholds for living kidney donation. _BMC Nephrol._ 19, 336 (2018). PubMed PubMed Central Google Scholar *
Boylan, K. et al. Immunoreactivity of the phosphorylated axonal neurofilament H subunit (pNF-H) in blood of ALS model rodents and ALS patients: evaluation of blood pNF-H as a potential ALS
biomarker. _J. Neurochem._ 111, 1182–1191 (2009). CAS PubMed Google Scholar * Frutiger, K., Lukas, T. J., Gorrie, G., Ajroud-Driss, S. & Siddique, T. Gender difference in levels of
Cu/Zn superoxide dismutase (SOD1) in cerebrospinal fluid of patients with amyotrophic lateral sclerosis. _Amyotroph. Lateral Scler._ 9, 184–187 (2008). CAS PubMed Google Scholar * Zamani,
A. et al. Impaired glymphatic function in the early stages of disease in a TDP-43 mouse model of amyotrophic lateral sclerosis. _Transl. Neurodegener._ 11, 17 (2022). CAS PubMed PubMed
Central Google Scholar * Hirose, M. et al. Stagnation of glymphatic interstitial fluid flow and delay in waste clearance in the SOD1-G93A mouse model of ALS. _Neurosci. Res._ 171, 74–82
(2021). CAS PubMed Google Scholar * Liu, S. et al. Glymphatic dysfunction in patients with early-stage amyotrophic lateral sclerosis. _Brain_ 147, 100–108 (2024). PubMed Google Scholar
* Shao, C. et al. Comprehensive analysis of individual variation in the urinary proteome revealed significant gender differences. _Mol. Cell. Proteom._ 18, 1110–1122 (2019). CAS Google
Scholar * Sharygin, D., Koniaris, L. G., Wells, C., Zimmers, T. A. & Hamidi, T. Role of CD14 in human disease. _Immunology_ 169, 260–270 (2023). CAS PubMed Google Scholar * Shive, C.
L., Jiang, W., Anthony, D. D. & Lederman, M. M. Soluble CD14 is a nonspecific marker of monocyte activation. _AIDS_ 29, 1263–1265 (2015). CAS PubMed Google Scholar * Rogers, M. L.,
Schultz, D. W., Karnaros, V. & Shepheard, S. R. Urinary biomarkers for amyotrophic lateral sclerosis: candidates, opportunities and considerations. _Brain Commun._ 5, fcad287 (2023).
PubMed PubMed Central Google Scholar * Bogdanov, M. et al. Increased oxidative damage to DNA in ALS patients. _Free Radic. Biol. Med._ 29, 652–658 (2000). CAS PubMed Google Scholar *
Saitoh, Y. & Takahashi, Y. Riluzole for the treatment of amyotrophic lateral sclerosis. _Neurodegener. Dis. Manag._ 10, 343–355 (2020). PubMed Google Scholar * Huang, C. S., Song, J.
H., Nagata, K., Yeh, J. Z. & Narahashi, T. Effects of the neuroprotective agent riluzole on the high voltage-activated calcium channels of rat dorsal root ganglion neurons. _J.
Pharmacol. Exp. Ther._ 282, 1280–1290 (1997). CAS PubMed Google Scholar * Fang, T. et al. Stage at which riluzole treatment prolongs survival in patients with amyotrophic lateral
sclerosis: a retrospective analysis of data from a dose-ranging study. _Lancet Neurol._ 17, 416–422 (2018). CAS PubMed PubMed Central Google Scholar * Chen, L., Liu, X., Tang, L., Zhang,
N. & Fan, D. Long-term use of riluzole could improve the prognosis of sporadic amyotrophic lateral sclerosis patients: a real-world cohort study in China. _Front. Aging Neurosci._ 8,
246 (2016). PubMed PubMed Central Google Scholar * Sanderink, G. J., Bournique, B., Stevens, J., Petry, M. & Martinet, M. Involvement of human CYP1A isoenzymes in the metabolism and
drug interactions of riluzole in vitro. _J. Pharmacol. Exp. Ther._ 282, 1465–1472 (1997). CAS PubMed Google Scholar * Ou‐Yang, D. et al. Phenotypic polymorphism and gender‐related
differences of CYP1A2 activity in a Chinese population. _Br. J. Clin. Pharmacol._ 49, 145–151 (2000). PubMed PubMed Central Google Scholar * Guengerich, F. P. & Shimada, T. Oxidation
of toxic and carcinogenic chemicals by human cytochrome P-450 enzymes. _Chem. Res. Toxicol._ 4, 391–407 (1991). CAS PubMed Google Scholar * Armon, C. Smoking may be considered an
established risk factor for sporadic ALS. _Neurology_ 73, 1693–1698 (2009). PubMed PubMed Central Google Scholar * Higgins, S. T. et al. A literature review on prevalence of gender
differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. _Prev. Med._ 80, 89–100 (2015). PubMed PubMed Central Google Scholar * Bruno, R.
et al. Population pharmacokinetics of riluzole in patients with amyotrophic lateral sclerosis. _Clin. Pharmacol. Ther._ 62, 518–526 (1997). CAS PubMed Google Scholar * Miller, T. M. et
al. Trial of antisense oligonucleotide tofersen for SOD1 ALS. _N. Engl. J. Med._ 387, 1099–1110 (2022). CAS PubMed Google Scholar * Steinacker, P. et al. Neurofilaments in the diagnosis
of motoneuron diseases: a prospective study on 455 patients. _J. Neurol. Neurosurg. Psychiatry_ 87, 12–20 (2016). PubMed Google Scholar * Thompson, A. G. et al. Multicentre appraisal of
amyotrophic lateral sclerosis biofluid biomarkers shows primacy of blood neurofilament light chain. _Brain Commun._ 4, fcac029 (2022). PubMed PubMed Central Google Scholar * Benatar, M.
et al. Validation of serum neurofilaments as prognostic and potential pharmacodynamic biomarkers for ALS. _Neurology_ 95, e59–e69 (2020). CAS PubMed PubMed Central Google Scholar *
Abu-Rumeileh, S. et al. Diagnostic-prognostic value and electrophysiological correlates of CSF biomarkers of neurodegeneration and neuroinflammation in amyotrophic lateral sclerosis. _J.
Neurol._ 267, 1699–1708 (2020). CAS PubMed Google Scholar * De Schaepdryver, M. et al. Neurofilament light chain and C reactive protein explored as predictors of survival in amyotrophic
lateral sclerosis. _J. Neurol. Neurosurg. Psychiatry_ 91, 436–437 (2020). PubMed Google Scholar * Lu, C. H. et al. Neurofilament light chain: a prognostic biomarker in amyotrophic lateral
sclerosis. _Neurology_ 84, 2247–2257 (2015). CAS PubMed PubMed Central Google Scholar * Verde, F. et al. Neurofilament light chain in serum for the diagnosis of amyotrophic lateral
sclerosis. _J. Neurol. Neurosurg. Psychiatry_ 90, 157–164 (2019). PubMed Google Scholar * Poesen, K. & Van Damme, P. Diagnostic and prognostic performance of neurofilaments in ALS.
_Front. Neurol_. 9, 1167 (2019). PubMed PubMed Central Google Scholar * Bali, T. et al. Defining SOD1 ALS natural history to guide therapeutic clinical trial design. _J. Neurol.
Neurosurg. Psychiatry_ 88, 99–105 (2017). PubMed Google Scholar * Shobeiri, P., Kalantari, A., Teixeira, A. L. & Rezaei, N. Shedding light on biological sex differences and
microbiota-gut-brain axis: a comprehensive review of its roles in neuropsychiatric disorders. _Biol. Sex Differ._ 13, 12 (2022). PubMed PubMed Central Google Scholar * Stachenfeld, N. S.
& Mazure, C. M. Precision medicine requires understanding how both sex and gender influence health. _Cell_ 185, 1619–1622 (2022). CAS PubMed Google Scholar * Bohr, T. et al. The
glymphatic system: current understanding and modeling. _iScience_ 25, 104987 (2022). PubMed PubMed Central Google Scholar * Hablitz, L. M. & Nedergaard, M. The glymphatic system: a
novel component of fundamental neurobiology. _J. Neurosci._ 41, 7698–7711 (2021). CAS PubMed PubMed Central Google Scholar * Yuan, A. & Nixon, R. A. Neurofilament proteins as
biomarkers to monitor neurological diseases and the efficacy of therapies. _Front. Neurosci._ 15, 689938 (2021). PubMed PubMed Central Google Scholar * Beckman, K. B. & Ames, B. N.
Oxidative decay of DNA. _J. Biol. Chem._ 272, 19633–19636 (1997). CAS PubMed Google Scholar * Carmeliet, P. Angiogenesis in life, disease and medicine. _Nature_ 438, 932–936 (2005). CAS
PubMed Google Scholar * Lambrechts, D. & Carmeliet, P. VEGF at the neurovascular interface: therapeutic implications for motor neuron disease. _Biochim. Biophys. Acta Mol. Basis Dis._
1762, 1109–1121 (2006). CAS Google Scholar * Lambrechts, D. et al. Meta-analysis of vascular endothelial growth factor variations in amyotrophic lateral sclerosis: increased susceptibility
in male carriers of the -2578AA genotype. _J. Med. Genet._ 46, 840–846 (2009). CAS PubMed Google Scholar * Ohta, Y. et al. Enhanced oxidative stress and the treatment by edaravone in
mice model of amyotrophic lateral sclerosis. _J. Neurosci. Res._ 97, 607–619 (2019). CAS PubMed Google Scholar * Canadian Agency for Drugs and Technologies in Health. _Sodium
Phenylbutyrate and Ursodoxicoltaurine (Albrioza)_ (CADTH, 2022). Download references ACKNOWLEDGEMENTS The authors are grateful to M. Bankole for the early discussions about this topic, and
to B. Belanger for designing the original figures. Original work in the laboratories of the authors is supported by grants from the Canadian Institutes of Health Research (CIHR, to K.A.S.
(FRN148380) and M.D.N. (FRN159591)), the K-Brain Project of the National Research Foundation (NRF, to S.H.K. (RS-2023-00265515)), the Krembil Foundation (to M.D.N.), the CIHR/International
Development Research Centre (CIHR/IDRC 109927 to G.P.), the ALS Society of Canada (to M.D.N. and G.P.), the Barry Barrett Foundation (to M.D.N. and G.P.) and the Rose Family Foundation (to
M.D.N. and G.P.). S.S.L. was a recipient of an Alberta Graduate Excellence Scholarship, a CIHR Master’s Scholarship, a Faculty of Graduate Studies Master’s Research Scholarship from the
University of Calgary, and a Donald Burns and Louise Berlin Graduate Award in Dementia from the Hotchkiss Brain Institute. S.M.J. was a recipient of an Alberta Graduate Excellence
Scholarship and Spinal Cord, Nerve Injury & Pain Scholarship from the University of Calgary Hotchkiss Brain Institute. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Hotchkiss Brain
Institute, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Sarah M. Jacob, Sukyoung Lee, Keith A. Sharkey, Gerald Pfeffer & Minh Dang Nguyen * Department of
Clinical Neurosciences, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Sarah M. Jacob, Sukyoung Lee, Gerald Pfeffer & Minh Dang Nguyen * Department of Cell
Biology and Anatomy, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Sukyoung Lee & Minh Dang Nguyen * Department of Biochemistry and Molecular Biology,
Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Sukyoung Lee & Minh Dang Nguyen * Department of Neurology, Hanyang University Hospital, Seoul, South Korea
Seung Hyun Kim * Snyder Institute for Chronic Diseases, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Keith A. Sharkey * Department of Physiology and
Pharmacology, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada Keith A. Sharkey * Department of Medical Genetics, Cumming School of Medicine, University of
Calgary, Calgary, Alberta, Canada Gerald Pfeffer Authors * Sarah M. Jacob View author publications You can also search for this author inPubMed Google Scholar * Sukyoung Lee View author
publications You can also search for this author inPubMed Google Scholar * Seung Hyun Kim View author publications You can also search for this author inPubMed Google Scholar * Keith A.
Sharkey View author publications You can also search for this author inPubMed Google Scholar * Gerald Pfeffer View author publications You can also search for this author inPubMed Google
Scholar * Minh Dang Nguyen View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS S.M.J., S.S.L., G.P., S.H.K., K.A.S. and M.D.N. wrote the
manuscript. All authors critically reviewed the manuscript drafts and approved the final manuscript for submission. CORRESPONDING AUTHORS Correspondence to Gerald Pfeffer or Minh Dang
Nguyen. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. PEER REVIEW PEER REVIEW INFORMATION _Nature Reviews Neurology_ thanks Pamela McCombe and the
other, anonymous, reviewer(s) for their contribution to the peer review of this work. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional
claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under
a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such
publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Jacob, S.M., Lee, S., Kim, S.H. _et al._ Brain–body mechanisms contribute to sexual
dimorphism in amyotrophic lateral sclerosis. _Nat Rev Neurol_ 20, 475–494 (2024). https://doi.org/10.1038/s41582-024-00991-7 Download citation * Accepted: 07 June 2024 * Published: 04 July
2024 * Issue Date: August 2024 * DOI: https://doi.org/10.1038/s41582-024-00991-7 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable
link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Life's a beach on teesside as three towns scoop seaside awardsA trio of Teesside beaches will be flying the flag for the coastline this summer after scooping the Seaside Award 2025. ...
Jeff stelling resigns as takeover update puts hartlepool united future in doubtJeff Stelling has resigned from his role as honorary president of Hartlepool United after the latest takeover update cas...
Mum-of-two michelle's interior design firm busting fears of unleashing colourA mum-of-two has taken the bold decision to give up her university day job and launch her own interior design company. M...
Brute dragged woman by hair and broke her nose in terrifying attackA 'misogynistic' brute broke his victim's nose in a horrific attack as he punched and kicked her in the f...
Glamping burrows venture with views of iconic landmark granted planning permission by councilNewsGlamping burrows venture with views of iconic landmark granted planning permission by councilThe burrows will be bui...
Latests News
Brain–body mechanisms contribute to sexual dimorphism in amyotrophic lateral sclerosisABSTRACT Amyotrophic lateral sclerosis (ALS) is the most common form of human motor neuron disease. It is characterized ...
Map: french property price variations in 2024 by regionONLY ONE REGION SAW HOUSE PRICES INCREASE LAST YEAR Houses fared significantly worse than flats when it came to price dr...
Tar heel family explains why they support trumpWABE’s mission is simple: “Inform, inspire, reflect and empower our greater Atlanta community. ” We do that through the ...
Can shops in france refuse to take payments in cash?THE QUESTION WAS SPARKED BY REPORTS OF SOME FRENCH SHOPS REFUSING TO ACCEPT NOTES AND COINS ON SUNDAYS All shops, festiv...
Is it possible to leave french second home to nephews and not spouse?JOHN KITCHING, A DIRECTOR OF FRENCH LAW CONSULTANCY LIMITED, ANSWERS A READER QUERY Reader Question: I live in the UK an...