Effects of whole blood storage in a polyolefin blood bag on platelets for acute normovolemic hemodilution
Effects of whole blood storage in a polyolefin blood bag on platelets for acute normovolemic hemodilution"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Acute normovolemic hemodilution (ANH) is a potential transfusion method for platelets, as well as for red blood cells. However, previous studies have shown that whole blood storage
in ANH decreases platelet aggregability by 14.7–76.3% and that this decrease is not recovered by reinfusion. We investigated whether a new whole blood storage method for 6 h using a
polyolefin bag, based on the platelet concentrates storage method, would maintain platelet function better than the conventional method using a polyvinyl chloride bag. We demonstrated that
storage of whole blood in a polyolefin bag maintained ADP-induced aggregation rates at more than twofold higher than those in a polyvinyl chloride bag, and also significantly suppressed
P-selectin expression, a platelet activation marker (ADP-induced aggregation rates: 24.6 ± 5.1% vs. 51.7 ± 11.5%, p = 0.002; P-selectin expression; 50.3 ± 8.4MFI vs. 31.6 ± 9.3MFI, p =
0.018). These results could be attributed to the high gas permeability of polyolefin, which lowered PCO2 and maintained a high pH with or without agitation. There were no significant changes
in platelet count and red blood cell parameters due to the storage methods. Our results suggest that ANH using polyolefin bags is advantageous in improving hemostatic function compared to
the conventional method. SIMILAR CONTENT BEING VIEWED BY OTHERS THE EFFECT OF SHORT-TERM REFRIGERATION ON PLATELET RESPONSIVENESS Article Open access 07 October 2022 DIVALENT MAGNESIUM
RESTORES CYTOSKELETAL STORAGE LESIONS IN COLD-STORED PLATELET CONCENTRATES Article Open access 14 April 2022 IMPACT OF G FORCE AND TIMING ON THE CHARACTERISTICS OF PLATELET-RICH FIBRIN
MATRICES Article Open access 16 March 2021 INTRODUCTION Allogeneic blood transfusion is a common treatment for perioperative hemorrhage. Cardiac surgeries use large amounts of blood
products, which consume 10–15% of the U.S. blood supply1. However, even small amounts of allogeneic blood transfusion increase mortality and serious complications2. For this reason and the
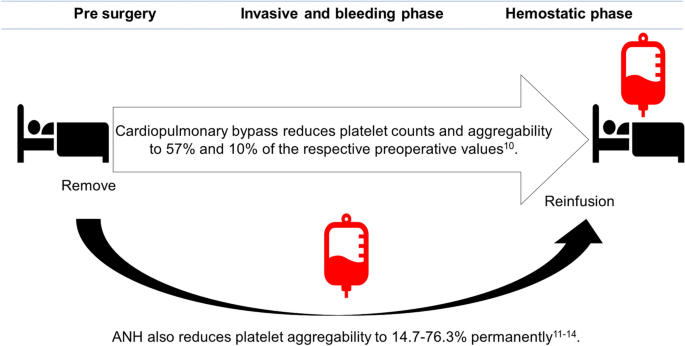
global shortage of blood products3,4, use of allogeneic transfusion needs to be reduced. Acute normovolemic hemodilution (ANH) is a simple and low-cost transfusion method that may be an
alternative option to allogeneic transfusion1. In ANH, 400–1200 mL of whole blood is removed from the patient immediately prior to an operation. The removed blood is mixed with CPDA solution
and is stored without agitation at room temperature at the bedside. The circulating blood of the patient is diluted by crystalloid or colloid solutions, which reduces blood loss during
surgery. At the conclusion of the operation, the stored autologous blood is restored to the patient (Fig. 1). ANH is safer than allogeneic blood transfusion because it does not cause
graft-versus-host disease, infection or transfusion-related acute lung injury1. ANH has been covered by a national health insurance in Japan since 2016. Previous reports have shown that ANH
substantially reduces intraoperative blood loss and allogeneic blood transfusion1,5,6. ANH also reduces platelet and plasma transfusion significantly in cardiac surgeries7. Platelets of
patients during cardiac surgeries are activated and consumed by cardiopulmonary bypass (CPB)8 through mechanisms of bypass- and heparin-induced activation, lack of extrinsic stimulating
factors, and exposure to hypothermia during bypass9. Kotake et al.10 showed that post-CPB platelet counts and ADP-induced aggregability decrease to 57% and 10% of the respective preoperative
values. ANH avoids potential platelet damage in CPB and can provide "fresh" platelets8. If ANH provides platelets with adequate hemostatic function, it can contribute to reduction
in blood loss and allogeneic transfusion volume after CPB. However, several studies have found that the conventional method of ANH severely impairs platelet aggregability assessed by whole
blood aggregometry, multiple electrode aggregometry, and impedance aggregometry (14.7–76.3% compared to pre-surgery) and that the function does not recover after transfusion11,12,13,14 (Fig.
1). Therefore, there is a need to develop a new ANH method with a high hemostatic effect by maintaining high platelet function in surgeries, including cardiac surgeries, in which massive
bleeding can occur. The storage conditions and expiration date of each blood production are shown in Table 11,15,16,17,18,19,20,21,22,23. The major differences in storage for ANH and
platelet concentrates are the bag material and use of agitation. Few studies mention the material of the storage bags used for ANH, but polyvinyl chloride (PVC) storage bags for red blood
cells are generally used because of their excellent durability despite their low gas permeability1,8,13,16,19,21. In contrast, platelet concentrates are stored with agitation in bags made of
highly oxygen-permeable materials such as polyolefin16,22, which provide sufficient oxygen for platelets to maintain aerobic respiration and ensure gas exchange between the storage medium
and the atmosphere24. We hypothesized that use of a PVC bag at rest is responsible for the significant reduction in platelet function in conventional ANH. Therefore, we examined if whole
blood storage in a polyolefin bag with or without agitation could maintain platelet function more effectively than that achieved by the conventional method. RESULTS The results are shown in
Table 2 and Fig. 2 (see "Methods" for the storage groups). First, the pH of venous blood mixed with CPDA before 6 h storage was lower than the normal venous blood pH (7.31–7.41)25
(Table 2 PRE). Compared to PRE, pH and ADP-induced platelet aggregation rates in PVN storage decreased significantly, and lactate and P-selectin increased significantly (Table 2 and Fig. 2
PRE–PVN). These results show that whole blood stored in the conventional ANH method severely impairs platelet function, as previous studies have shown11,12,13,14 (Fig. 1). In contrast, whole
blood storage in polyolefin bags maintained significantly higher pH and ADP-induced platelet aggregation rates and significantly lower PCO2 and P-selectin, compared to those in the PVN
group (Table 2 and Fig. 2 PON–PVN). PO2 in the PON group was relatively high, but not significantly higher than in the PVN group. No parameters in the PVA group differed significantly from
those in the PVN group, and the POA and PON group showed significant differences from PVN in the same parameters. There were no significant changes in platelet count, mean platelet volume,
and red blood cell parameters among all groups. DISCUSSION In this study, we showed that whole blood storage in a polyolefin bag maintained higher ADP-induced platelet aggregation rates and
lower P-selectin expression, compared to the conventional method used in ANH (Table 2 and Fig. 2). The decrease in aggregation rate measured by light transmittance aggregometry correlates
with the amount of bleeding26,27. P-selectin (CD62P) is a membrane protein present in α granules of platelets, and its expression level on the unstimulated platelet surface is a common
measure of platelet activations28. Platelets stored in the container are affected by various factors including duration of storage, temperature, pH, solution, gas permeability of the
container for O2 and CO2 and interruption of agitation29. The platelet injuries associated with extracorporeal storage are called platelet storage lesions (PSLs)30, which lead to platelet
activation via the necrotic and apoptotic processes, resulting the reduction of survival in vivo and hemostatic activity after transfusion29. Thus, decline of agonist-induced aggregation
rates, P-selectin expression, morphological change and increased lactate level are the major manifestations of PSLs. ANH using polyolefin bags is advantageous in reducing PSLs and improving
hemostatic function over the conventional method. Some studies have shown that platelet function of whole blood stored in blood bags markedly decreases and does not recover after transfusion
in ANH. Ramnarine et al. showed that collagen-induced formation of large stable hemostatic aggregates (platelet macroaggregation) were markedly decreased to 29.4% after collecting blood
into a CPDA bag and to 14.7% after 80 min of storage, compared to that before the collection, and that this deterioration was largely irreversible by the reinfusion of ANH12. Scott et al.
showed that blood in bag storage with CPDA for 300 min had significantly reduced platelet function, as measured by thrombin receptor activating peptide stimulation in multiple electrode
aggregometry (Multiplate) analysis and maximum clot formation on ROTEM EXTEM13. Gallandat Huet et al. showed platelet aggregation response measured by Multiplate in ex-vivo stored blood with
heparin decreased compared to the pre-CPB levels11. Therefore, a new preservation method is required to maintain the platelet function in ANH. In our study, storage with highly gas
permeable polyolefin maintained lower PCO2 and higher pH compared to PVN group (Table 2 and Fig. 2). Of ATP production by platelets, 85% is derived from aerobic metabolism24,29. In the
1980s, platelet concentrates were stored in PVC bags, but could not maintain the platelet function because of the accumulation of CO2 and lactate followed by a rapid decrease of pH31. Low pH
generally causes platelet morphological change (below 6.7) and irreversible loss of viability (below 6.2)30,32. The whole blood stored in PVC bags in our study also showed a significant
decrease in pH, but these declines were insufficient to cause the morphological changes. The polyolefin bags currently used for storage of platelet concentrates are 2.2 times more oxygen
permeable and 3.6 times more CO2 permeable than PVC bags22,33. Use of high gas-permeable containers with gentle agitation ensures O2 and CO2 exchange between the storage medium and the
atmosphere, and prevents local hypoxia resulting in lactate production22,24. This storage condition prevents PSLs and increases the ability to stop bleeding after transfusion22,29. However,
it is unclear whether the gas permeability of the bag affected the aerobic metabolism of platelets in our results. Krause et al. showed that just limiting gas exchange in storage bag of
platelet concentrates causes accumulation of PCO2, decreased pH, increased lactate, and increased P-selectin expression34. Similarly, the high gas permeability of the storage bag in our
study may have led to higher aggregation rates and low P-selectin expression, although the underlying biochemical pathway is unknown. Mean platelet volume of platelets generally increases
inversely related to pH, indicating a poor quality of product35, which did not change in this study. In contrast, there were no significant differences caused by agitation (Table 2 and Fig.
2, PVN–PVA, PON–POA). Thomas24 showed that interruption of agitation for several hours did not reduce platelet function. In addition to agitation, the platelet concentration and the surface
area of the storage bag affect the oxygen partial pressure33. The effect of agitation on the platelet count and function may depend on the storage container, agitation speed and other
conditions. Preservative solution and temperature also influence PSLs. CPDA used in ANH is an anticoagulating solution suitable for long term storage of red blood cells in preoperative
autologous blood donation20, but is not optimized for platelet storage. CPDA contains sodium citrate hydrate and dextrose, and the pH is 5.6–5.8. Several studies have reported that citric
acid impairs platelet function even in short-time storage as practiced in ANH12,36. Hyperglycemia can induce hyperreactivity of platelets to high shear stress and increased P-selectin within
4 h37,38. For these reasons, CPDA is not a suitable solution for storage of platelets. The recommended temperature for platelet storage has changed over time. Platelet storage at 4 °C was
performed in the 1970s, but 20–24 °C or room temperature is currently recommended based on reports that platelets stored below 20–24 °C rapidly change irreversibly and lose their viability
after transfusion24,32. Room temperature storage is also recommended in ANH, but the temperature in the operating room during hypothermic CPB often falls below 20 °C, which may impair
platelet function. However, some reports have indicated that cold-stored platelets contribute effectively to hemostasis30,39 and the US Food and Drug Administration recently approved
cold-stored platelets in resuscitation of patients with active bleeding40. Therefore, we are planning the next study to clarify the appropriate preservative solutions and temperature for
ANH, which provide better platelet function and reduce perioperative blood loss. Red blood cell storage lesions are measured with indicators of hemolysis and the ability to deliver oxygen.
There were no significant changes in hemoglobin concentration in all groups in this study. In general, several-hours whole blood storage at room temperature does not cause unacceptable
injury to red blood cell functions41; 6-h whole blood storage at 20 °C with CPD decreases 2.3-DPG to 88%, which is acceptable42. Low pH suppresses the activity of glycolysis system, which in
turn reduces 2,3-DPG required to supply oxygen to peripheral tissues and ATP production required to maintain erythrocyte morphology43, but 2,3-DPG and ATP levels recover in 7–72 h after
transfusion43. High oxygen concentrations may confer oxidative stress, but the appropriate concentration range has not been determined23,43. Blood storage in polyolefin bags for several
weeks are associated with greater red blood cells hemolysis compared to the storage in di-2-ethylhexil phthalate PVC bags17, but storage for several hours in our study had no effect. Mean
corpuscular volume, a parameter of the erythrocyte morphology and storage lesions, tends to increase during storage44,45, but this also did not increase in our study. Red blood cells can be
stored for a longer period than platelets, and the storage conditions such as higher PO2 for several hours may not affect their function44,46. There are several limitations of this study.
First, in order to reduce the burden on the volunteers, the amount of sample blood per bag was set at 20 mL, which is much less than the recommended capacity. Therefore, the surface area,
internal pressure and effect of agitation in our storage bags might not be the same as those in clinical use. Storage with small amounts will allow easier agitation and gas exchange. Our
results should be supplemented by full volume experiments in the future. Second, in addition to the material and gas permeability, the different surface structures and plasticizers between
the two bags used may have influenced the results. Other products may have different effects on blood cells, because the structures of blood bag varies from manufacturer to manufacturer16.
Third, ANH also improves CPB-induced coagulopathy47, but the effects of storage conditions of ANH on coagulation factors were not examined. Coagulation factors, even the most affected factor
VIII, are maintained at more than 70%, which is sufficient for hemostasis, in 24-h whole blood storage at room temperature48. Global hemostasis assay such as thromboelastography or
rotational thromboelastometry should be considered as an additional functional assay. Fourth, as this study was performed in vitro, the hemostatic effect and survival time and hemolysis in
vivo of stored platelets could not be evaluated. Within these limitations, our results show that whole blood stored in a polyolefin bag for 6 h maintains significantly higher platelet
function compared to the conventional method of storage in a PVC bag, while agitation had no effect on the results. METHODS The study was approved by the ethics committee of Kyoto University
Hospital (R0978-1) and carried out according to the guidelines of the Declaration of Helsinki. All methods were performed in accordance with the institutional guidelines and regulations.
Prior written informed consent was obtained from subjects. A study flow chart is shown in Fig. 3. STORAGE GROUPS Four storage methods were examined: at rest in a PVC bag, as in conventional
ANH (PVN); agitation in a PVC bag (PVA); at rest in a polyolefin bag (PON); and agitation in a polyolefin bag (POA). A Karmi CA (200 mL single, Kawasumi Laboratories, Inc., Tokyo, Japan)
made of polyvinyl chloride including di-2-ethylhexyl phthalate plasticizer and containing CPDA solution was used as the PVC bag. A Kawasumi Separation bag PO (1000 mL single. Kawasumi
Laboratories) made of polyolefin without any plasticizer and anticoagulant was used as the polyolefin bag. The O2 permeabilities of the PVC and polyolefin bags are 1.10 ± 0.04 and 2.37 ±
0.30 nmol/min/atm/cm2 and the CO2 permeabilities are 9.8 ± 0.5 and 35.43 ± 6.8 nmol/min/atm/cm2, respectively33. CPDA solution was removed from the PVC bag, and the volume of each PVC and
polyolefin bag was adjusted to 20 mL by rolling the bag up and fixed with metal clips. A horizontal rotatory agitator (Labo Shaker BC-740, Bio Craft, Inc, Tokyo, Japan) was used for
agitation at 60 rpm. CHEMICALS AND DRUGS ADP was purchased from Nacalai Tesque (Kyoto, Japan). Peridinin chlorophyll protein (PerCP)-labeled anti-CD61 antibody, and phycoerythrin
(PE)-labeled anti-CD62P (P-selectin) antibody were obtained from Becton Dickinson (San Diego, CA, USA). The composition of CPDA removed from a PVC bag was citric acid hydrate 0.327 w/v%,
sodium citrate hydrate 2.630 w/v%, monobasic sodium phosphate 0.251 w/v%, dextrose 2.900 w/v% and adenine 0.0275 w/v%. The pH was 5.6–5.8. All other chemicals were of analytical grade. It
was confirmed that all buffers and solvents used for dilution had no effects on the results. BLOOD COLLECTION AND STORAGE A sample of 80 mL of venous blood was collected by venipuncture of
forearm veins from 6 healthy volunteers who had not taken any medication for at least two weeks before blood sampling. The blood was mixed with 11.2 mL of CPDA (8.14 v/v%; the percentage
specified for use of PVC bags currently used in ANH) gently. After removal of 11 mL of blood for testing (sample PRE), the rest of the blood was divided into 20 mL volumes for each of the
four groups. The blood was injected into 4 bags and extra air was removed. PVN and PON bags were set at rest, while PVA and POA bags were placed on a horizontal rotatory agitator at 60 rpm,
with all 4 bags stored at 22 °C in an incubator box for 6 h. After storage, the blood was agitated gently and tested (samples PVN, PVA, PON, POA). COMPLETE BLOOD COUNT AND BLOOD GAS ANALYSIS
Each sample (PRE, PVN, PVA, PON, POA) was tested promptly after collection using the following methods. Complete blood counts and blood gas parameters were measured using an automated
hematology analyzer (Celltac α Nihon Kohden, Tokyo, Japan) and an automated blood gas analyzer (RAPIDPoint 500 or RAPIDLab 1265 Siemens Healthineers, Munich, Germany). MEASUREMENT OF
ADP-INDUCED PLATELET AGGREGATION RATES Platelet-rich plasma (PRP) was prepared by centrifugation of a blood sample at 160_g_ for 10 min at room temperature, followed by collection of the
supernatant. The remaining lower portion was further centrifuged at 1600_g_ for 15 min at room temperature and the clear supernatant was used as platelet-poor plasma (PPP). The platelet
count was adjusted to 3 × 105/μL by dilution with PPP (adjusted PRP). Aggregation induced by ADP was measured with a light transmission aggregometer (MCM Hema Tracer 212; MC Medical, Tokyo,
Japan). Adjusted PRP (3 × 105/μL, 200 μL) was pipetted into a cylindrical cuvette and incubated at 37 °C for 3 min, and then the adjusted PRP was stirred at 37 °C with a magnetic bar at 1000
rpm. A 10-μL volume of 200 μM ADP (final concentration: 9.5 μM) was added to the cylindrical cuvette and ADP-induced platelet aggregation rates was measured for 10 min as a change in light
transmission from that of PPP, which was taken to be 100%. FLOW CYTOMETRY ANALYSIS OF P-SELECTIN Flow cytometry was performed as we have described previously49,50. Adjusted PRP was diluted
tenfold with phosphate-buffered saline (PBS) (pH 7.42) containing 139 mM NaCl, 8.1 mM NaHPO4, 1.5 mM KH2PO4, and 2.7 mM KCl. Samples were fixed with ice-cold 1% formaldehyde for at least 60
min in a refrigerator and washed twice with ice-cold PBS by centrifugation at 1600_g_ for 15 min at 4 °C. The pellet was suspended in 100 μL PBS at 4 °C. 20 μL of the suspension was
coincubated with PerCP-labeled anti-CD61 antibody and PE-labeled anti-CD62P (P-selectin) antibody in a final volume of 100 μL adjusted with PBS for 60 min at room temperature in the dark.
PE-labeled IgG was used to estimate nonspecific binding. The reaction was stopped by adding ice-cold PBS. Samples were analyzed using a fluorescence-activated cell sorting instrument
(FACSCalibur Becton Dickinson, San Jose, CA, USA). For each sample, data from 10,000 platelets were collected. Platelets were identified by forward and side scatter intensity and by CD61
expression. P-selectin levels on activated platelet surface membranes were recorded as the mean fluorescent intensity (MFI) of PE. STATISTICAL ANALYSIS All data are expressed as a mean
(standard deviation: SD) of 6 experiments. Group variances were tested by a Brown-Forsythe test and were statistically equal. All data were compared by one-way ANOVA, followed by a Dunnett
test compared to PVN. All analyses were performed using JMP Pro 15.10 (https://www.jmp.com/ja_jp/software/predictive-analytics-software.html) (SAS Institute Inc., Cary, NC, USA) with _P_
< 0.05 considered significant. REFERENCES * Shander, A. _et al._ Standards and best practice for acute normovolemic hemodilution: Evidence-based consensus recommendations. _J.
Cardiothorac. Vasc. Anesth._ 34, 1755–1760 (2020). Article PubMed Google Scholar * Ferraris, V. A., Davenport, D. L., Saha, S. P., Austin, P. C. & Zwischenberger, J. B. Surgical
outcomes and transfusion of minimal amounts of blood in the operating room. _Arch. Surg._ 147, 49–55 (2012). Article PubMed Google Scholar * Roberts, N., James, S., Delaney, M. &
Fitzmaurice, C. The global need and availability of blood products: A modelling study. _Lancet. Haematol._ 6, e606–e615 (2019). Article PubMed Google Scholar * Ellingson, K. D. _et al._
Continued decline in blood collection and transfusion in the United States—2015. _Transfusion_ 57, 1588–1598 (2017). Article PubMed PubMed Central Google Scholar * Barile, L. _et al._
Acute normovolemic hemodilution reduces allogeneic red blood cell transfusion in cardiac surgery: A systematic review and meta-analysis of randomized trials. _Anesth. Analg._ 124, 743–752
(2017). Article PubMed Google Scholar * Zhou, X., Zhang, C., Wang, Y., Yu, L. & Yan, M. Preoperative acute normovolemic hemodilution for minimizing allogeneic blood transfusion: A
meta-analysis. _Anesth. Analg._ 121, 1443–1455 (2015). Article PubMed Google Scholar * Goldberg, J. _et al._ Greater volume of acute normovolemic hemodilution may aid in reducing blood
transfusions after cardiac surgery. _Ann. Thorac. Surg._ 100, 1581–1587 (2015). Article PubMed PubMed Central Google Scholar * Ferraris, V. A. _et al._ Perioperative blood transfusion
and blood conservation in cardiac surgery: the society of thoracic surgeons and the society of cardiovascular anesthesiologists clinical practice guideline. _Ann. Thorac. Surg._ 83, S27–S86
(2007). Article PubMed Google Scholar * Ortmann, E. _et al._ Point-of-care assessment of hypothermia and protamine-induced platelet dysfunction with multiple electrode aggregometry
(Multiplate) in patients undergoing cardiopulmonary bypass. _Anesth. Analg._ 116, 533–540 (2013). Article CAS PubMed Google Scholar * Kotake, Y. _et al._ Platelet dysfunction during
cardiopulmonary bypass assessed by a novel whole-blood aggregometer. _J. Cardiothorac. Vasc. Anesth._ 20, 536–540 (2006). Article PubMed Google Scholar * Gallandat Huet, R. C. G., de
Vries, A. J., Cernak, V. & Lisman, T. Platelet function in stored heparinised autologous blood is not superior to in patient platelet function during routine cardiopulmonary bypass.
_PLoS One_ 7, 1–4 (2012). Google Scholar * Ramnarine, I. R. _et al._ Autologous blood transfusion for cardiopulmonary bypass: Effects of storage conditions on platelet function. _J.
Cardiothorac. Vasc. Anesth._ 20, 541–547 (2006). Article PubMed Google Scholar * Scott, K. J., Shteamer, J. W., Szlam, F. & Sniecinski, R. M. Platelet function, but not thrombin
generation, is impaired in acute normovolemic hemodilution (ANH) blood. _J. Clin. Anesth._ 58, 39–43 (2019). Article PubMed Google Scholar * Reyher, C. _et al._ Einfluss der akuten
normovolämischen hämodilution auf die primäre hämostase. _Anaesthesist_ 63, 496–502 (2014). Article CAS PubMed Google Scholar * Storch, E. K., Custer, B. S., Jacobs, M. R., Menitove, J.
E. & Mintz, P. D. Review of current transfusion therapy and blood banking practices. _Blood Rev._ 38, 100593 (2019). Article PubMed Google Scholar * Prowse, C. V. _et al._
Commercially available blood storage containers. _Vox Sang._ 106, 1–13 (2014). Article CAS PubMed Google Scholar * Hill, H. R., Oliver, C. K., Lippert, L. E., Greenwalt, T. J. &
Hess, J. R. The effects of polyvinyl chloride and polyolefin blood bags on red blood cells stored in a new additive solution. _Vox Sang._ 81, 161–166 (2001). Article CAS PubMed Google
Scholar * Robinson, S. _et al._ The administration of blood components: A British Society for Haematology Guideline. _Transfus. Med._ 28, 3–21 (2018). Article CAS PubMed Google Scholar
* Udani, D., Porecha, M., Mehta, S., Vaghela, M. & Doshi, D. A comparative study of autologous versus homologous blood transfusion during general surgery. _Internet J. Surg._ 19, 1–6
(2008). Google Scholar * Thomas, M. J. G., Gillon, J. & Desmond, M. J. Preoperative autologous donation. _Transfusion_ 36, 633–639 (1996). Article CAS PubMed Google Scholar *
Vanderlinde, E. S., Heal, J. M. & Blumberg, N. Autologous transfusion. _BMJ_ 324, 772–775 (2002). Article PubMed PubMed Central Google Scholar * Van der Meer, P. F. & de Korte,
D. Platelet preservation: Agitation and containers. _Transfus. Apher. Sci._ 44, 297–304 (2011). Article PubMed Google Scholar * Antonelou, M. H. & Seghatchian, J. Insights into red
blood cell storage lesion: Toward a new appreciation. _Transfus. Apher. Sci._ 55, 292–301 (2016). Article PubMed Google Scholar * Thomas, S. Platelets: Handle with care. _Transfus. Med._
26, 330–338 (2016). Article CAS PubMed Google Scholar * Singh, V., Gupta, P. & Khatana, S. Blood gas analysis for bedside diagnosis. _Natl. J. Maxillofac. Surg._ 4, 136 (2013).
Article PubMed PubMed Central Google Scholar * Jin, L. _et al._ The prognostic value of ADP-induced platelet aggregation for bleeding complications in low—Intermediate risk patients with
acute coronary syndrome taking clopidogrel after percutaneous coronary intervention. _Hear. Lung Circ._ 26, 49–57 (2017). Article Google Scholar * Adeli, E. K., Alavi, S. M.,
Alizadeh-ghavidel, A., Bakhshandeh-Abkenar, H. & Pourfathollah, A. A. Perioperative changes in platelet count and function in patients undergoing cardiac surgery. _Med. J. Islam. Repub.
Iran._ 10, 31–37 (2017). Google Scholar * Dumont, L. J., VandenBroeke, T. & Ault, K. A. Platelet surface P-selectin measurements in platelet preparations: An international collaborative
study. _Transfus. Med. Rev._ 13, 31–42 (1999). Article CAS PubMed Google Scholar * Ohto, H. & Nollet, K. E. Overview on platelet preservation: Better controls over storage lesion.
_Transfus. Apher. Sci._ 44, 321–325 (2011). Article PubMed Google Scholar * Seghatchian, J. & Krailabsiri, P. The platelet storage lesion. _Transfus. Med. Rev._ 11, 130–144 (1997).
Article CAS PubMed Google Scholar * Murphy, S. _et al._ Improved storage of platelets for transfusion in a new container. _Blood_ 60, 194–200 (1982). Article CAS PubMed Google Scholar
* Holme, S. Storage and quality assessment of platelets. _Vox Sang._ 74(Suppl 2), 207–216 (1998). Article CAS PubMed Google Scholar * Torres, R. & Tormey, C. A. Modelling gas
exchange during platelet storage without agitation. _Vox Sang._ 111, 445–448 (2016). Article CAS PubMed Google Scholar * Krause, M., Doescher, A., Zimmermann, B. & Müller, T. H.
Noninvasive pH measurement to monitor changes during suboptimal storage of platelet concentrates. _Transfusion_ 50, 2185–2192 (2010). Article CAS PubMed Google Scholar * Singh, H.,
Chaudhary, R. & Ray, V. Platelet indices as quality markers of platelet concentrates during storage. _Clin. Lab. Haematol._ 25, 307–310 (2003). Article CAS PubMed Google Scholar *
Wallén, N. H., Ladjevardi, M., Albert, J. & Bröijersén, A. Influence of different anticoagulants on platelet aggregation in whole blood; A comparison between citrate, low molecular mass
heparin and hirudin. _Thromb. Res._ 87, 151–157 (1997). Article PubMed Google Scholar * Gaiz, A., Mosawy, S., Colson, N. & Singh, I. Thrombotic and cardiovascular risks in type two
diabetes; Role of platelet hyperactivity. _Biomed. Pharmacother._ 94, 679–686 (2017). Article CAS PubMed Google Scholar * Gresele, P. _et al._ Acute, short-term hyperglycemia enhances
shear stress-induced platelet activation in patients with Type II diabetes mellitus. _J. Am. Coll. Cardiol._ 41, 1013–1020 (2003). Article CAS PubMed Google Scholar * Valeri, C. R.
Circulation and hemostatic effectiveness of platelets stored at 4 C or 22 C: Studies in aspirin-treated normal volunteers. _Transfusion_ 16, 20–23 (1976). Article CAS PubMed Google
Scholar * Stubbs, J. R. _et al._ Cold platelets for trauma-associated bleeding: Regulatory approval, accreditation approval, and practice implementation—Just the “tip of the iceberg”.
_Transfusion_ 57, 2836–2844 (2017). Article CAS PubMed Google Scholar * Thomas, S. Ambient overnight hold of whole blood prior to the manufacture of blood components. _Transfus. Med._
20, 361–368 (2010). Article PubMed Google Scholar * Knutson, F., Lööf, H. & Högman, C. F. Pre-separation storage of whole blood: The effect of temperature on red cell
2,3-diphosphoglycerate and myeloperoxidase in plasma. _Transfus. Sci._ 21, 111–115 (1999). Article CAS PubMed Google Scholar * Yoshida, T., Prudent, M. & D’Alessandro, A. Red blood
cell storage lesion: Causes and potential clinical consequences. _Blood Transfus._ 17, 27–52 (2019). PubMed PubMed Central Google Scholar * Ghezelbash, B. _et al._ Comparative evaluation
of biochemical and hematological parameters of pre-storage leukoreduction during RBC storage. _Int. J. Hematol. Stem Cell Res._ 12, 35–42 (2018). Google Scholar * Kim, S. J., Lee, E. Y.,
Song, Y. J. & Song, J. The instability of commercial control materials in quality control of mean corpuscular volume. _Clin. Chim. Acta_ 434, 11–15 (2014). Article CAS PubMed Google
Scholar * Yoshida, T., AuBuchon, J. P., Tryzelaar, L., Foster, K. Y. & Bitensky, M. W. Extended storage of red blood cells under anaerobic conditions. _Vox Sang._ 92, 22–31 (2007).
Article CAS PubMed Google Scholar * Suzuki, R. _et al._ Effect of autotransfusion using intraoperative predonated autologous blood on coagulopathy during thoracic aortic surgery: A
randomized controlled trial. _Ann. Thorac. Cardiovasc. Surg._ 25, 311–317 (2019). Article PubMed PubMed Central Google Scholar * Cardigan, R. _et al._ Coagulation factor content of
plasma produced from whole blood stored for 24 hours at ambient temperature: Results from an international multicenter BEST Collaborative study. _Transfusion_ 51, 50S-57S (2011). Article
CAS PubMed Google Scholar * Murata, Y., Kawamoto, S. & Fukuda, K. Rocuronium has a suppressive effect on platelet function via the P2Y12 receptor pathway in vitro that is not reversed
by sugammadex. _Int. J. Med. Sci._ 21, 1–10 (2020). Google Scholar * Kawamoto, S., Hirakata, H., Sugita, N. & Fukuda, K. Bidirectional effects of dexmedetomidine on human platelet
functions in vitro. _Eur. J. Pharmacol._ 766, 122–128 (2015). Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS This work was supported by Grant-in-Aid for
Scientific Research (KAKENHI), Grant Number 19K18293. AUTHOR INFORMATION Author notes * These authors contributed equally: Yutaka Murata and Eriko Kusudo. AUTHORS AND AFFILIATIONS *
Department of Anesthesia, Kyoto University Hospital, 54 Shogoin Kawahara-cho, Sakyo-ku, Kyoto, 606-8507, Japan Yutaka Murata, Eriko Kusudo, Shuji Kawamoto & Kazuhiko Fukuda Authors *
Yutaka Murata View author publications You can also search for this author inPubMed Google Scholar * Eriko Kusudo View author publications You can also search for this author inPubMed Google
Scholar * Shuji Kawamoto View author publications You can also search for this author inPubMed Google Scholar * Kazuhiko Fukuda View author publications You can also search for this author
inPubMed Google Scholar CONTRIBUTIONS Y.M. and E.K.: data collection, data analysis, and drafting of the paper. S.K.: study conception and design, interpretation of data, and revision of the
manuscript. K.F.: supervising the study and revision of the manuscript. All authors have approved the final version of the paper. CORRESPONDING AUTHOR Correspondence to Shuji Kawamoto.
ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional
claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which
permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to
the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Murata, Y., Kusudo, E., Kawamoto, S. _et al._ Effects of whole blood storage in a
polyolefin blood bag on platelets for acute normovolemic hemodilution. _Sci Rep_ 11, 12201 (2021). https://doi.org/10.1038/s41598-021-91725-y Download citation * Received: 06 March 2021 *
Accepted: 31 May 2021 * Published: 09 June 2021 * DOI: https://doi.org/10.1038/s41598-021-91725-y SHARE THIS ARTICLE Anyone you share the following link with will be able to read this
content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Stranger things star unrecognisable after debuting major change at netflix eventAhead of Stranger Things' much-anticipated final season premiere, one of its stars has undergone a dramatic transfo...
Doctor claims eating cheese at specific part of day could be bad for your healthThe time of day you eat cheese could be negatively impacting your health. Britain is a nation of cheese-lovers, and we&#...
Loose women star shares health scare and says 'my body was shutting down'Loose Women's Charlene White revealed her harrowing health scare on Wednesday's show, confessing that her body...
'i let my toddler watch netflix's ms rachel and now i regret it massively'I became a mum for the first time over two-years-ago and I'm still trying to navigate the tumultuous journey of mot...
Inside UK's most haunted hotel where 'guests leave in the middle of the night'NewsInside UK's most haunted hotel where 'guests leave in the middle of the night'Ye Olde King's Head is said to be one ...
Latests News
Effects of whole blood storage in a polyolefin blood bag on platelets for acute normovolemic hemodilutionABSTRACT Acute normovolemic hemodilution (ANH) is a potential transfusion method for platelets, as well as for red blood...
Westminster prioritises the establishment over the people — Scottish National PartyWestminster prioritises the establishment over the people by the SNP Share this article: 0 Facebook Share Twitter Share ...
Inside UK's most haunted hotel where 'guests leave in the middle of the night'NewsInside UK's most haunted hotel where 'guests leave in the middle of the night'Ye Olde King's Head is said to be one ...
Loose women star shares health scare and says 'my body was shutting down'Loose Women's Charlene White revealed her harrowing health scare on Wednesday's show, confessing that her body...
Doctor claims eating cheese at specific part of day could be bad for your healthThe time of day you eat cheese could be negatively impacting your health. Britain is a nation of cheese-lovers, and we&#...