Using chads2 and cha2ds2-vasc scores for mortality prediction in patients with chronic kidney disease
Using chads2 and cha2ds2-vasc scores for mortality prediction in patients with chronic kidney disease"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Chronic kidney disease (CKD) is a public health issue and is associated with high morbidity and mortality. How to identify the high-risk CKD patients is very important to improve
the long-term outcome. CHADS2 and CHA2DS2-VASc scores are clinically useful scores to evaluate the risk of stroke in patients with atrial fibrillation. However, there was no literature
discussing about the usefulness of CHADS2 and CHA2DS2-VASc scores for cardiovascular (CV) and all-cause mortality prediction in CKD patients. This longitudinal study enrolled 437 patients
with CKD. CHADS2 and CHA2DS2-VASc scores were calculated for each patient. CV and all-cause mortality data were collected for long-term outcome prediction. The median follow-up to mortality
was 91 (25th–75th percentile: 59–101) months. There were 66 CV mortality and 165 all-cause mortality. In addition to age and heart rate, CHADS2 and CHA2DS2-VASc scores (both _P_ value <
0.001) were significant predictors of CV and all-cause mortality in the multivariate analysis. Besides, in direct comparison of multivariate model, basic model + CHA2DS2-VASc score had a
better additive predictive value for all-cause mortality than basic model + CHADS2 score (_P_ = 0.031). In conclusion, our study showed both of CHADS2 and CHA2DS2-VASc scores were
significant predictors for long-term CV and all-cause mortality in CKD patients and CHA2DS2-VASc score had a better predictive value than CHADS2 score for all-cause mortality in direct
comparison of multivariate model. Therefore, using CHADS2 and CHA2DS2-VASc scores to screen CKD patients may be helpful in identifying the high-risk group with increased mortality. SIMILAR
CONTENT BEING VIEWED BY OTHERS THE ROLE OF KIDNEY DYSFUNCTION IN COVID-19 AND THE INFLUENCE OF AGE Article Open access 23 May 2022 THE OPTIMAL CUT-OFF VALUES OF KLOTHO FOR PREDICTING
ALL-CAUSE AND CARDIOVASCULAR MORTALITY AMONG CHRONIC KIDNEY DISEASE: RESULTS FROM NHANES Article Open access 26 February 2024 ASSOCIATION OF SERUM URIC ACID WITH ALL-CAUSE AND CARDIOVASCULAR
MORTALITY IN CARDIOVASCULAR DISEASE PATIENTS Article Open access 04 November 2024 INTRODUCTION Chronic kidney disease (CKD), including end-stage renal disease (ESRD), is a public health
issue in the world and is associated with high morbidity and mortality1,2,3,4. Cardiovascular (CV) disease is one of the leading causes of mortality in this population. Therefore, there are
many programs of quality care and medical therapies developed to control the growing incidence, prevalence, and mortality for the patients with CKD5,6. CHADS2 score is a useful scoring
system to evaluate the risk of stroke in patients with atrial fibrillation (AF). In AF patients, there is a strong association between the CHADS2 score and the annual risk of stroke7,8. In
addition, CHADS2 score was used to predict CV outcomes in the patients without AF9,10,11. Nevertheless, in recent years, CHA2DS2-VASc score has become a more useful score than CHADS2 score
for prediction of stroke and systemic embolization in AF patients12,13,14. This new scoring system was also used to predict future CV outcome including mortality in non-AF patients15,16,17.
However, there was no literature discussing about the usefulness of CHADS2 and CHA2DS2-VASc scores for CV and all-cause mortality prediction in the patients with CKD. Therefore, our study
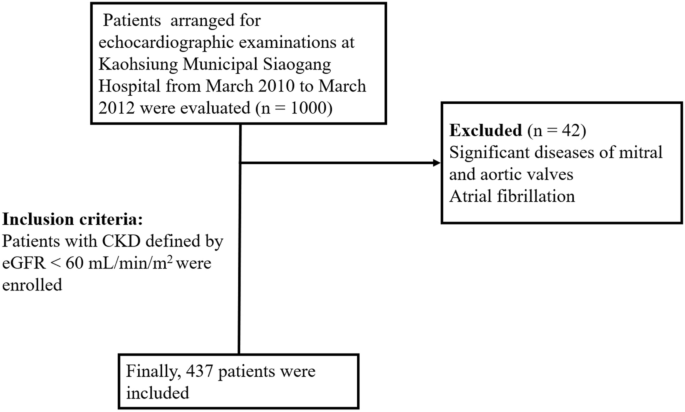
was aimed to evaluate the issue. METHODS STUDY POPULATION We evaluated a group of patients (n = 1000) arranged for echocardiographic examinations at Kaohsiung Municipal Siaogang Hospital
from March 2010 to March 2012 because of suspecting coronary artery disease, hypertension, heart failure, abnormal cardiac physical examination, and survey for dyspnea. We excluded 42
subjects with significant atrial fibrillation and diseases of mitral and aortic valves. Patients with CKD defined by estimated glomerular filtration rate (eGFR) < 60 mL/min/m2 were
enrolled. Finally, 437 patients were included (Fig. 1). This study was approved by the institutional review board committee of the Kaohsiung Medical University Hospital (KMUH-IRB). We
acquired informed consents from the patients and conducted our study according to the declaration of Helsinki. We obtained medical and demographic data from the medical records. ASSESSMENT
OF CHADS2 SCORE AND CHA2DS_2_-VASC SCORE We calculated CHADS2 score based on the scoring system as following: 1 point was assigned for age ≧ 75 years, the presence of hypertension, diabetes
mellitus, and congestive heart failure, and 2 points were assigned for transient ischemic attack or a history of stroke7,8. In addition, we calculated CHA2DS2-VASc score based on the scoring
system as following: 1 point was assigned for congestive heart failure, hypertension, age between 65 and 74 years, diabetes mellitus, female sex, and vascular disease, and 2 points were
assigned for a history of stroke and age ≥ 75 years. CKD was defined by eGFR < 60 mL/min/m2 and classified as stages 3, 4, and 5 based on eGFR level (30 to 59, 15 to 29, and < 15
mL/min/1.73 m2) with kidney damage lasting for more than 3 months. DEFINITION OF MORTALITY We followed our patients till December 2018 and acquired survival information and causes of death
from the official death certificate and final confirmation by the Ministry of Health and Welfare. The causes of death were classified by the International Classification of Diseases 9th
Revision. Causes of CV mortality were defined deaths due to cerebral vascular disease, ischemic heart disease, myocardial infarction, heart failure, valvular heart disease and
atherosclerotic vascular disease. The detailed method was the same as our previous published paper18. STATISTICAL ANALYSIS SPSS 22.0 was used to perform the statistical analyses. Our data
was shown as percentage or mean ± standard deviation. Categorical variables were compared by Chi-square test. Continuous variables were compared by independent samples t-test. We selected
significant variables in our univariate analysis into multivariate analysis. We adjusted significant variables and time to mortality by Cox regression analysis. In addition, we also
performed multivariate analysis using full model with all variables to predict the CV and all-cause mortality. We calculated the improvement of global chi-square to evaluate the additive
value of CHADS2 score and CHA2DS2-VASc score over basic model for long-term CV and all-cause mortality prediction. Subgroup analysis by age, gender, CKD stages, hypertension, diabetes,
stroke/transient ischemic attack (TIA), heart failure, and vascular disease were also performed to estimate CHADS2 and CHA2DS2-VASc score for all-cause mortality. All tests were 2-sided and
the level of significance was established as _P_ < 0.05. RESULTS CV and all-cause mortality data were collected up to December 2018. Mortality data were obtained from the Collaboration
Center of Health Information Application (CCHIA), Ministry of Health and Welfare, Executive Yuan, Taiwan. The follow-up period to mortality events was 91 (25th–75th percentile: 59–101)
months in all patients. Mortality events were documented during the follow-up period, including CV mortality (n = 66) and all-cause mortality (n = 165). CLINICAL CHARACTERISTICS BETWEEN
PATIENTS WITH CKD STAGE 3, 4, AND 5 Among the 437 subjects, mean age was 68 ± 12 years. Clinical characteristics between patients with CKD stage 3, 4, and 5 were shown in Table 1. There were
significant difference between different CKD stage in prevalence of diabetes (_P_ = 0.001), hypertension (_P_ = 0.002), stroke/TIA (_P_ = 0.014), CHADS2 score (1.63 ± 1.15 versus 2.00 ±
1.07 versus 2.34 ± 1.30, _P_ = 0.001), CHA2DS2-VASc score (2.97 ± 1.59 versus 3.46 ± 1.76 versus 3.54 ± 1.87, _P_ = 0.029), calcium channel blocker use (_P_ = 0.003), and diuretic use (_P_ =
0.002). PREDICTORS OF CV AND ALL-CAUSE MORTALITY IN THE UNIVARIATE ANALYSIS Several parameters were evaluated in our study to predict the CV and all-cause mortality. These parameters
included age, gender, dyslipidemia, smoking, heart rate, body mass index, CHADS2 score, CHA2DS2-VASc scores, and medication use such as aspirin, beta blocker, calcium channel blocker,
angiotensin converting enzyme inhibitor, angiotensin II receptor blocker, and diuretic. The predictors of CV and all-cause mortality using Cox proportional hazards model in the univariate
analysis were shown in Table 2. For prediction of CV mortality, age, heart rate, body mass index, CHADS2 score, and CHA2DS2-VASc score (both _P_ value < 0.001) were significant
predictors. For prediction of all-cause mortality, age, heart rate, body mass index, CHADS2 score, and CHA2DS2-VASc score (both _P_ value < 0.001), and diuretic use were significant
predictors. PREDICTORS OF CV MORTALITY IN THE MULTIVARIATE ANALYSIS We selected significant variables in our univariate analysis into multivariate analysis and used Cox proportional hazards
model to evaluate the predictors of CV mortality. We tried to evaluate the predictive value of CHADS2 score and CHA2DS2-VASc score in two different models, respectively. Data was shown in
Table 3. Model 1 included the significant variables in the univariate analysis except CHA2DS2-VASc score, including age, heart rate, body mass index, and CHADS2 score. Model 2 included the
significant variables in the univariable analysis except CHADS2 score, including age, heart rate, body mass index, and CHA2DS2-VASc score. In model 1, age, heart rate, and CHADS2 score
(hazard ratio [HR] = 1.574; 95% confidence interval [CI]: 1.264–1.961; _P_ < 0.001) were significant predictors after multivariate analysis. In model 2, age, heart rate, and CHA2DS2-VASc
score (HR 1.511; 95% CI 1.266–1.804; _P_ < 0.001) were significant predictors after multivariate analysis. PREDICTORS OF ALL-CAUSE MORTALITY IN THE MULTIVARIATE ANALYSIS We further used
Cox proportional hazards model to evaluate the predictors of all-cause mortality and the data was shown in Table 4. Similar methodology was used as in Table 3. Model 1 included the
significant variables in the univariable analysis except CHA2DS2-VASc score, including age, heart rate, body mass index, diuretic use, and CHADS2 score. Model 2 included the significant
variables in the univariable analysis except CHADS2 score, including age, heart rate, body mass index, diuretic use, and CHA2DS2-VASc score. In model 1, age, heart rate, and CHADS2 score (HR
1.470; 95% CI 1.276–1.693; _P_ < 0.001) were significant predictors after multivariable analysis. In model 2, age, heart rate, and CHA2DS2-VASc score (HR 1.421; 95% CI 1.266–1.596; _P_
< 0.001) were significant predictors after multivariable analysis. PREDICTORS OF CV AND ALL-CAUSE MORTALITY USING FULL MODEL WITH ALL VARIABLES IN MULTIVARIATE ANALYSIS In addition to use
significant variables in the univariate analysis to perform multivariate analysis, we also performed a full model with all variables presented in Table 1 to evaluate the predictors of CV
and all-cause mortality and the data were shown in Table 5. For prediction of CV mortality, after adjusting all variables, age, male gender, hypertension, heart failure, and CHA2DS2-VASc
score (HR 1.600; 95% CI 1.254–2.040; _P_ < 0.001) were significant predictors of CV mortality. CHADS2 score became non-significant after multivariate analysis (_P_ 0.260). For prediction
of all-cause mortality, after adjusting all variables, age, male gender, heart failure, CHA2DS2-VASc score (HR 1.503; 95% CI 1.300–1.739; _P_ < 0.001), and ARB use were significant
predictors of all-cause mortality. CHADS2 score became non-significant after multivariate analysis (_P_ = 0.607). SUBGROUP ANALYSIS IN ESTIMATING CHADS2 AND CHA2DS2-VASC SCORE FOR ALL-CAUSE
MORTALITY We further used subgroup analysis to estimate CHADS2 and CHA2DS2-VASc score for all-cause mortality (Table 6). Several subgroup analysis were performed, including age (age < 65
year or ≥ 65 year), gender (male or female), CKD stage (stage 3 or stage 4–5), hypertension (yes or No), diabetes (yes or no), stroke/TIA (yes or no), heart failure (yes or no), and vascular
disease (yes or no). CHADS2 score only showed non-significant finding in subgroup with stroke/TIA and subgroup with heart failure. CHA2DS2-VASc score only showed non-significant finding in
subgroup with stroke/TIA. However, these non-significant findings might be related to small subgroup sample size. There were only 34 patients with stroke/TIA and 54 patients with heart
failure. In addition, for subgroup of CKD stage, we combined CKD stage 4 (n = 50) and stage 5 (n = 35) because of small sample size (Table 6). NESTED COX MODEL FOR CV MORTALITY AND ALL-CAUSE
MORTALITY PREDICTION We used Nested Cox model for CV mortality (Fig. 2A) and all-cause mortality (Fig. 2B) prediction. We calculated the improvement of global chi-square to evaluate the
additive value of CHADS2 score and CHA2DS2-VASc score over basic model for long-term CV and all-cause mortality prediction. The basic model in Fig. 2A included age, heart rate, and body mass
index. After adding CHADS2 score and CHA2DS2-VASc score into the basic model respectively, we found both of basic model + CHADS2 score and basic model + CHA2DS2-VASC score had a better
predictive value for CV mortality than basic model itself (both _P_ < 0.001). However, there was no significant difference between basic model + CHADS2 score and basic model +
CHA2DS2-VASc score (_P_ = 0.062). The basic model in Fig. 2B included age, heart rate, body mass index, and diuretic use. After adding CHADS2 score and CHA2DS2-VASc score into the basic
model respectively, we found both of basic model + CHADS2 score and basic model + CHA2DS2-VASc score had a better predictive value for all-cause mortality than basic model itself (both _P_
< 0.001). In addition, basic model + CHA2DS2-VASc score had a better predictive value for all-cause mortality than basic model + CHADS2 score (_P_ = 0.031). THE KAPLAN–MEIER CURVES OF
DIFFERENT CKD STAGES FOR ALL-CAUSE MORTALITY-FREE SURVIVAL PREDICTION We further compared the different CKD stages (CKD stage 3, 4, and 5) for all-cause mortality prediction (Fig. 3, _P_
< 0.001). HR of CKD stage 4 versus stage 3 was 1.849 (95% CI 1.528–3.523; _P_ < 0.001) and HR of CKD stage 5 versus stage 3 was 3.221 (95% CI 2.064–5.029; _P_ < 0.001) for
prediction of all-cause mortality. DISCUSSION Our study was aimed to evaluate the usefulness of CHADS2 and CHA2DS2-VASc scores on the prediction of CV and all-cause mortality in CKD
patients. There were several major findings in the present study. First, both of CHADS2 and CHA2DS2-VASc scores were significant predictors of CV and all-cause mortality after multivariable
analysis. Second, both of CHADS2 and CHA2DS2-VASc scores had an additive value than conventional parameters for prediction of CV and all-cause mortality. Furthermore, in direct comparison of
multivariate model, CHA2DS2-VASc score had a better value than CHADS2 score for prediction of all-cause mortality, but not CV mortality. Third, higher stage of CKD was associated with
higher all-cause mortality in CKD patients. CKD was associated with accelerated risk and high event rate of CV disease, and was considered as a CV disease equivalent19. Patients with CKD had
several risk factors that were related to atherosclerosis, such as hypertension, diabetes mellitus, dyslipidemia, smoking, and so on20. These risk factors could cause remodeling of the
myocardium and blood vessels and lead to arterial stiffness and atherosclerosis, cardiomyopathy, and subsequently to ischemic heart disease, heart failure, CV death, rapid deterioration of
renal function, and finally progression to ESRD19. The mortality rates associated with CKD were striking. According to the literature, mortality in patients with CKD was 56% greater than
that in patients without CKD, the risk was even much higher in patients with CKD stages 4–5. For the patients with ESRD, the 5-year survival rate was only 35% in the United States21.
Therefore, how to identify the high-risk CKD patients with increased mortality was very important to improve the long-term outcome. Both of CHADS2 and CHA2DS2-VASc scores were practical and
useful scoring system to evaluate the risk of stroke in AF patients7,8,12,13,14. However, CHA2DS2-VASc score had recently become a more useful score and outperformed CHADS2 score for
prediction of stroke and systemic embolization12,14. In addition, both of CHADS2 and CHA2DS2-VASc scores were also used to predict CV outcomes in non-AF patients9,10,11,15,16,17. Chen et al.
reported that CHADS2 and CHA2DS2-VASc scores could be used to predict 1-year all-cause mortality in patients with systolic heart failure15. Hoshino T et al. showed that CHADS2 and
CHA2DS2-VASc scores were useful in predicting functional status after stroke in patients with coronary artery disease16. Svendsen JH et al. also revealed that CHADS2 and CHA2DS2-VASc scores
were associated with increased risk of stroke and death in patients paced for sick sinus syndrome17. However, there was no literature discussing about the usefulness of CHADS2 and
CHA2DS2-VASc scores for CV and all-cause mortality prediction in the patients with CKD. Our study was the first study tried to investigate the issue. In our study, both of CHADS2 and
CHA2DS2-VASc scores were associated with increased CV and all-cause mortality in univariable and multivariable analyses. In addition, we found that CHA2DS2-VASc score had a better value than
CHADS2 score for prediction of all-cause mortality in direct comparison of multivariate model (_P_ = 0.031), but this finding was not found in CV mortality (_P_ = 0.062). Our study also
showed that increased CKD stage was associated with higher all-cause mortality, which was reasonable as our clinical practice. STUDY LIMITATIONS First, non-fatal events were not evaluated in
this study. Second, CV medications might affect the study results; however, we already adjusted the medications in our multivariate analysis as possible as we can to avoid the influence of
medications. Because we initially excluded the patients with atrial fibrillation, we did not collect the information of oral anticoagulant use in our study. CONCLUSIONS Our study was the
first study to evaluate the usefulness of CHADS2 and CHA2DS2-VASc scores in CKD patients for prediction of long-term CV and all-cause mortality. Our study showed both of CHADS2 and
CHA2DS2-VASc scores were significant predictors for long-term CV and all-cause mortality in CKD patients and CHA2DS2-VASc score had a better predictive value than CHADS2 score for all-cause
mortality in direct comparison of multivariate model. Therefore, using CHADS2 and CHA2DS2-VASc scores to screen CKD patients may help physicians to identify the high-risk group with
increased mortality. REFERENCES * Vlachopoulos, C. _et al._ Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. _JAMA Netw. Open_ 2, e1912831.
https://doi.org/10.1001/jamanetworkopen.2019.12831 (2019). Article PubMed PubMed Central Google Scholar * Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic
kidney disease and the risks of death, cardiovascular events, and hospitalization. _N. Engl. J. Med._ 351, 1296–1305. https://doi.org/10.1056/NEJMoa041031 (2004). Article CAS PubMed
Google Scholar * Hwang, S. J., Tsai, J. C. & Chen, H. C. Epidemiology, impact and preventive care of chronic kidney disease in Taiwan. _Nephrology (Carlton)_ 15(Suppl 2), 3–9.
https://doi.org/10.1111/j.1440-1797.2010.01304.x (2010). Article Google Scholar * Tonelli, M. _et al._ Chronic kidney disease and mortality risk: a systematic review. _J. Am. Soc.
Nephrol._ 17, 2034–2047. https://doi.org/10.1681/ASN.2005101085 (2006). Article PubMed Google Scholar * Whittaker, C. F., Miklich, M. A., Patel, R. S. & Fink, J. C. Medication safety
principles and practice in CKD. _Clin. J. Am. Soc. Nephrol._ 13, 1738–1746. https://doi.org/10.2215/CJN.00580118 (2018). Article PubMed PubMed Central Google Scholar * Lin, M. Y. _et
al._ Effect of national pre-ESRD care program on expenditures and mortality in incident dialysis patients: a population-based study. _PLoS ONE_ 13, e0198387.
https://doi.org/10.1371/journal.pone.0198387 (2018). Article CAS PubMed PubMed Central Google Scholar * Gage, B. F. _et al._ Selecting patients with atrial fibrillation for
anticoagulation: stroke risk stratification in patients taking aspirin. _Circulation_ 110, 2287–2292. https://doi.org/10.1161/01.CIR.0000145172.55640.93 (2004). Article CAS PubMed Google
Scholar * Gage, B. F. _et al._ Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. _JAMA_ 285, 2864–2870.
https://doi.org/10.1001/jama.285.22.2864 (2001). Article CAS PubMed Google Scholar * Poci, D. _et al._ Role of the CHADS2 score in acute coronary syndromes: risk of subsequent death or
stroke in patients with and without atrial fibrillation. _Chest_ 141, 1431–1440. https://doi.org/10.1378/chest.11-0435 (2012). Article PubMed Google Scholar * Welles, C. C. _et al._ The
CHADS2 score predicts ischemic stroke in the absence of atrial fibrillation among subjects with coronary heart disease: data from the Heart and Soul Study. _Am. Heart J._ 162, 555–561.
https://doi.org/10.1016/j.ahj.2011.05.023 (2011). Article PubMed PubMed Central Google Scholar * Li, Y., Wang, J., Lv, L., Xu, C. & Liu, H. Usefulness of the CHADS2 and R2CHADS2
scores for prognostic stratification in patients with coronary artery disease. _Clin. Interv. Aging_ 13, 565–571. https://doi.org/10.2147/CIA.S156208 (2018). Article CAS PubMed PubMed
Central Google Scholar * Lip, G. Y., Nieuwlaat, R., Pisters, R., Lane, D. A. & Crijns, H. J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial
fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. _Chest_ 137, 263–272. https://doi.org/10.1378/chest.09-1584 (2010). Article PubMed
Google Scholar * January, C. T. _et al._ 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of
Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. _Circulation_ 130, 2071–2104. https://doi.org/10.1161/CIR.0000000000000040 (2014).
Article PubMed Google Scholar * Kirchhof, P. _et al._ 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. _Eur. Heart J._ 37, 2893–2962.
https://doi.org/10.1093/eurheartj/ehw210 (2016). Article PubMed Google Scholar * Chen, Y. L. _et al._ Mortality prediction using CHADS2/CHA2DS2-VASc/R2CHADS2 scores in systolic heart
failure patients with or without atrial fibrillation. _Medicine (Baltimore)_ 96, e8338. https://doi.org/10.1097/MD.0000000000008338 (2017). Article Google Scholar * Hoshino, T., Ishizuka,
K., Shimizu, S. & Uchiyama, S. CHADS2, CHA2DS2-VASc, and R2CHADS2 scores are associated with 3-month functional outcome of stroke in patients with prior coronary artery disease. _Circ.
J._ 78, 1481–1485. https://doi.org/10.1253/circj.cj-14-0038 (2014). Article CAS PubMed Google Scholar * Svendsen, J. H. _et al._ CHADS2 and CHA2DS2-VASc score to assess risk of stroke
and death in patients paced for sick sinus syndrome. _Heart_ 99, 843–848. https://doi.org/10.1136/heartjnl-2013-303695 (2013). Article CAS PubMed Google Scholar * Hsu, P. C. _et al._
Upstroke time per cardiac cycle as a novel parameter for mortality prediction in patients with acute myocardial infarction. _J. Clin. Med._ 9, E904. https://doi.org/10.3390/jcm9040904
(2020). Article PubMed Google Scholar * Briasoulis, A. & Bakris, G. L. Chronic kidney disease as a coronary artery disease risk equivalent. _Curr. Cardiol. Rep._ 15, 340.
https://doi.org/10.1007/s11886-012-0340-4 (2013). Article PubMed Google Scholar * Chen, S. C. _et al._ Prognostic cardiovascular markers in chronic kidney disease. _Kidney Blood Press
Res._ 43, 1388–1407. https://doi.org/10.1159/000492953 (2018). Article PubMed Google Scholar * Ghaderian, S. B., Hayati, F., Shayanpour, S. & Beladi-Mousavi, S. S. Diabetes and
end-stage renal disease; a review article on new concepts. _J. Renal Injury Prev._ 4, 28–33. https://doi.org/10.2861/jrip.2015.07 (2015). Article CAS Google Scholar Download references
ACKNOWLEDGEMENTS Mortality data were provided by the Collaboration Center of Health Information Application, Ministry of Health and Welfare, Executive Yuan. FUNDING Funding was provided by
Kaohsiung Medical University Chung-Ho Memorial Hospital (Grant No. KMUH97-7G36). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Division of Cardiology, Department of Internal Medicine,
Kaohsiung Medical University Hospital, Kaohsiung, Taiwan Po-Chao Hsu, Wen-Hsien Lee, Ying-Chih Chen, Chun-Yuan Chu, Tsung-Hsien Lin, Wen-Chol Voon, Wen-Ter Lai, Sheng-Hsiung Sheu &
Ho-Ming Su * Division of Nephrology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan Szu-Chia Chen & Yi-Chun Tsai * Faculty of Medicine, College
of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan Po-Chao Hsu, Wen-Hsien Lee, Szu-Chia Chen, Yi-Chun Tsai, Chun-Yuan Chu, Tsung-Hsien Lin, Wen-Chol Voon, Wen-Ter Lai,
Sheng-Hsiung Sheu & Ho-Ming Su * Department of Internal Medicine, Kaohsiung Municipal Siaogang Hospital, Kaohsiung Medical University, 482, Shan-Ming Rd., Hsiao-Kang Dist., Kaohsiung,
812, Taiwan, ROC Wen-Hsien Lee, Szu-Chia Chen, Ying-Chih Chen & Ho-Ming Su Authors * Po-Chao Hsu View author publications You can also search for this author inPubMed Google Scholar *
Wen-Hsien Lee View author publications You can also search for this author inPubMed Google Scholar * Szu-Chia Chen View author publications You can also search for this author inPubMed
Google Scholar * Yi-Chun Tsai View author publications You can also search for this author inPubMed Google Scholar * Ying-Chih Chen View author publications You can also search for this
author inPubMed Google Scholar * Chun-Yuan Chu View author publications You can also search for this author inPubMed Google Scholar * Tsung-Hsien Lin View author publications You can also
search for this author inPubMed Google Scholar * Wen-Chol Voon View author publications You can also search for this author inPubMed Google Scholar * Wen-Ter Lai View author publications You
can also search for this author inPubMed Google Scholar * Sheng-Hsiung Sheu View author publications You can also search for this author inPubMed Google Scholar * Ho-Ming Su View author
publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS P.-C.H., W.-H.L., and H.-M.S. drafted the manuscript. S.-C.C., Y.-C.C., M.-K.L. and C.-Y.C. prepared
tables and assisted with the statistical analysis. T.-H.L., W.-C.V., W.-T.L., S.-H.S., and H.-M.S. conceived of the study and participated in its design and coordination. All authors have
read and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Ho-Ming Su. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL
INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as
long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third
party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the
article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the
copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Hsu, PC., Lee, WH., Chen,
SC. _et al._ Using CHADS2 and CHA2DS2-VASc scores for mortality prediction in patients with chronic kidney disease. _Sci Rep_ 10, 18942 (2020). https://doi.org/10.1038/s41598-020-76098-y
Download citation * Received: 20 April 2020 * Accepted: 21 October 2020 * Published: 03 November 2020 * DOI: https://doi.org/10.1038/s41598-020-76098-y SHARE THIS ARTICLE Anyone you share
the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative
Trending News
Preserving the dignity of our aging parentsPROVIDE CHOICES "Being able to offer an array of options regarding the small, daily things is essential,” says Trac...
China only evacuated taiwanese who were 'chinese'China's embassy only evacuated the Taiwanese tourists stranded in Japan by Typhoon Jebi who identified as Chinese, ...
Taiwan tries to smooth china's ruffled feathersWASHINGTON — Taiwan sought Monday to defuse a diplomatic row over its president’s call for an independence vote, saying ...
When remote learning goes wrong: zoom classes for preschoolers can be extra burdens on parents who just want refunds2010-11 (Combined average): 6.19%Best year: 2007 (9.23%)Worst year: 2009 (3.15%)When the recession was at its worst, the...
Taiwan’s kuomintang picks new taipei city mayor as presidential candidateTaiwan’s Kuomintang picks New Taipei City mayor as presidential candidate | WTVB | 1590 AM · 95.5 FM | The Voice of Bran...
Latests News
Using chads2 and cha2ds2-vasc scores for mortality prediction in patients with chronic kidney diseaseABSTRACT Chronic kidney disease (CKD) is a public health issue and is associated with high morbidity and mortality. How ...
The page you were looking for doesn't exist.You may have mistyped the address or the page may have moved.By proceeding, you agree to our Terms & Conditions and our ...
Rod Connolly – The ConversationProfile Articles Activity I am Professor in Marine Science at Griffith University in southeast Queensland, Australia. Re...
The page you were looking for doesn't exist.You may have mistyped the address or the page may have moved.By proceeding, you agree to our Terms & Conditions and our ...
The page you were looking for doesn't exist.You may have mistyped the address or the page may have moved.By proceeding, you agree to our Terms & Conditions and our ...