Prenatal tobacco exposure modulated the association of genetic variants with diagnosed adhd and its symptom domain in children: a community based case–control study
Prenatal tobacco exposure modulated the association of genetic variants with diagnosed adhd and its symptom domain in children: a community based case–control study"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT The purpose of our study was to test the hypothesis that prenatal tobacco smoking exposure (PSE) could modulate the association of genetic variants with ADHD. A community based
case-control study was conducted among Chinese children and 168 ADHD patients and 233 controls were recruited by using combination diagnosis of DSM-IV, SNAP-IV and semi-structured clinical
interview. Logistic regression analysis was performed to estimate the effect of prenatal tobacco smoking exposure and genotype frequencies on ADHD susceptibility individually by adjustment
for potential confounders. Multiplicative and additive interaction analysis were performed to evaluate the interactions between risk genes and PSE with regard to ADHD. Prenatal tobacco smoke
exposure was a significant risk factor of ADHD even after adjusted for other potential confounders. _ADRA2A_ rs553668, _DRD2_ rs1124491 and _SLC6A4_ rs6354 were identified to be associated
with ADHD. A significant multiplicative and additive gene-environment interactions were observed between the PSE and the _ADRA2A_ rs553668 in relation to ADHD and ADHD-ODD. The risk of the
genetic variants in ADHD was increased significantly if the child had prenatal tobacco exposure. The genetic risk for ADHD could be influenced by the presence of environmental risks. The
environmental and the genetic risks are not distinct to each other. More gene-environment interaction studies were needed to reveal the etiology of ADHD. SIMILAR CONTENT BEING VIEWED BY
OTHERS EVALUATION OF THE CAUSAL RELATIONSHIP BETWEEN SMOKING AND SCHIZOPHRENIA IN EAST ASIA Article Open access 09 September 2022 POLYGENIC RISK SCORES FOR LATE SMOKING INITIATION ASSOCIATED
WITH THE RISK OF SCHIZOPHRENIA Article Open access 23 November 2020 THE EFFECTS OF POLYGENIC RISK FOR PSYCHIATRIC DISORDERS AND SMOKING BEHAVIOUR ON PSYCHOTIC EXPERIENCES IN UK BIOBANK
Article Open access 28 September 2020 INTRODUCTION Attention-deficit/hyperactivity disorder (ADHD) is a chronic neurodevelopmental disorder characterized by developmentally inappropriate
level of inattentiveness and hyperactivity. It is one of the most frequently diagnosed disorders among children and adolescents, with the pooled prevalence of 7.2%1 worldwide and 6.26%2 in
China according to the most recent meta-analysis. Previous studies reveal that individuals affected by ADHD frequently lead to various social functional impairment, such as social
communication disorder, bad peer relationships, academic performance difficulties3, develop personality disorder, substance abuse and even criminality4,5. As a complex multi-factorial
disease, exact etiology of ADHD is still elusive. The biologic basis for ADHD is thought to be largely genetic6,7. The genetic architecture of ADHD is complex and numerous single nucleotide
polymorphisms (SNPs) of genes involved in the regulation of neurotransmitter systems are identified to be associated with ADHD8,9,10.Among them, genes involved in the dopaminergic,
serotonergic and noradrenergic pathways are the most common candidate genes for ADHD studies7,11,12,13. Adding to genetic influence, environmental factors are assumed to be co-involved in
the etiology of ADHD14. Some prenatal and perinatal factors are reported to be associated with ADHD, such as younger maternal pregnant age15, caesarean, induced delivery, preterm birth, low
birth weight16, and mother smoking during pregnancy. With regard to prenatal smoking, it is constantly identified to be a risk factor for offspring hyperactivity symptom and ADHD14,17,18,19.
Evidence from epidemiological researches suggests that maternal cigarette smoking and environmental tobacco exposure during pregnancy are all in association with high risk of ADHD. Hyunjoo
Joo20 and his colleagues have described that independent and combined exposure to pre- and postnatal secondhand smoke were associated with ADHD, particularly with the hyperactivity symptom
domain. A large population-based birth cohort have provided that maternal smoking during pregnancy was associated with children hyperactivity symptom19. Although large numbers of studies
demonstrated a relationship between maternal smoking exposure during pregnancy and ADHD, most of previous studies have investigated the effect of smoking exposure only and there were few
studies on gene–environment interactions which were more likely to play the real role in the etiology of ADHD21. Importantly, the environmental risk is not distinct to the genetic
influence21, but it may be required to uncover the genetic liability14. The studies about the G ene× Environment studies of gene and smoking exposure on ADHD are limited. A gene-environment
interplay study reports that the co-exist group of prenatal smoking exposure and 10 R/10 R genotype of _DAT_ gene showed a higher mean scores of hyperactivity-impulsivity and inattentiveness
than other groups22. But the findings remain speculative since the participants are lack of a clinical diagnosis of ADHD, and the ADHD scores of the participants was derived from the
Conners’ Parent Rating Scale which will lead to the overdiagnosis of the ADHD. Developing of novel technologies have made it more common in identifying genetic risk factors of ADHD, however,
proved the genetic architecture of ADHD to be far more complex, since the genetic influences expressed only additional risks to disease susceptibility23. Therefore, gene and environment
interaction research will be an inevitable way to explore the etiologic mechanisms of ADHD. However, studies about the joint effects of gene and environmental factors on ADHD is limited14.
To fill the knowledge gap, we conducted the case-control study to elucidate the potential synergistic effect of the prenatal tobacco exposure during pregnancy and children genetic variants
on children diagnosed ADHD and its symptom domains. RESULTS CHARACTERISTICS OF PARTICIPANTS The study involved 168 ADHD patients and 233 controls. A higher proportion of males was noted with
the 5.2:1 boys/girls ratio. Compared with the controls, ADHD children were more likely to have younger mother (_p_ < 0.05). There were no significant difference between ADHD patients and
controls in terms of family history of neural system diseases, parental marital status, preterm birth (pregnancy < 37weeks), Low birth weight(birth weight <2500 g) and delivery mode,
levels of blood lead and postnatal tobacco exposure. Meanwhile, ADHD children scored higher of SNAP-IV scales (Inattention domain, hyperactive domain and ODD domain) and of CBCL total scores
than controls (Table 1). ASSOCIATIONS BETWEEN THE _ADRA2A_, _DRD2_, AND _SLC6A4_ GENETIC VARIANTS AND ADHD SUSCEPTIBILITY A total of 22 SNPs were detected. The genotype distributions of
_SLC6A4_ rs25533 and rs2020923, and _SLC6A3_ rs2975226 in the controls deviated from Hardy–Weinberg equilibrium (P < 0.05). Thus they were excluded from further analysis. Consequently, a
total of 19 SNPs remained in the subsequent analysis In individual SNP association analysis, _ADRA2A_ rs553668, _DRD2_ rs1124491 and _SLC6A4_ rs6354 were nominally significant at the
uncorrected 0.05 significance level with adjustment for age and gender. Among these SNPs, _ADRA2A_ rs553668G allele was associated with an increased risk of ADHD in the additive model, and
_SLC6A4_ rs6354 (GG + GT) was associated with an increased risk of ADHD, whereas _DRD2_ rs1124491 (AA) was associated with a decreased risk of ADHD. After FDR adjustment, _SLC6A4_ rs6354
remained statistically significant (_P_ = 0.019, Table S1). As the Table 2 illuminated, the detected SNPs were not associated with all symptom domains of ADHD. After adjusting for age and
gender, individuals carrying the _ADRA2A_ rs553668 GG or AG genotype showed an increased risk of ADHD compared with those carrying AA genotype (adjusted OR = 1.76, 95% CI = 1.12–2.77, _P_ =
0.013), but the SNP was not associated with ADHD-ODD. Additionally, individuals who carried _DRD2_ rs1124491 AG or GG genotype displayed a risk association with inattention symptom compared
to AA genotype (adjusted OR = 2.22, 95% CI = 1.11–4.46, _P_ = 0.022). Compared with those carrying TT genotype, the risk association with ADHD-ODD was increased significantly in individuals
carrying the _SLC6A4_ rs6354 GT or GG genotype (adjusted OR = 2.18, 95% CI = 1.04–4.56, _P_ = 0.034), but no association was observed in other ADHD symptom domains. The ORs and 95% CIs
changed slightly in different adjustment model (Model 1, 2, 3, Table 2). PRENATAL TOBACCO SMOKE EXPOSURE (PSE) AS A RISK FACTOR FOR ADHD The prenatal tobacco smoke exposure (PSE) showed a
risk association with ADHD and all symptom domains, and slight change of the OR and 95% CI was observed in different adjustment model (Model1, 2, 3). The strong association was shown in ODD
symptom domain (OR = 2.80, 95% CI = 1.39–5.66) and in the hyperactivity symptom domain (OR = 2.12, 95% CI = 1.23–3.60, Table 3). INTERACTION BETWEEN PRENATAL TOBACCO SMOKING EXPOSURE AND
GENETIC VARIANTS The MDR analysis revealed that the three-factor model including rs553668, rs1124491 and prenatal tobacco smoking exposure was the best predictor for ADHD risk (Table 4).
Furthermore, we calculated the multiplicative and additive interactions between _ADRA2A_ rs553668, _DRD2_ rs1124491, _SLC6A4_ rs6354 and prenatal tobacco smoking exposure after adjustment of
age of the child, gender, pregnancy age of mother, and postnatal smoking exposure. A significant additive interaction between PSE and _ADRA2A_ rs553668 polymorphisms is detected. The AP due
to interaction was 0.48(95% CI = 0.09–0.87), and RERI was 1.88(95% CI = 0.06–4.12), Meanwhile, multiplicative interaction was displayed in this group (_P_mul = 0.003). The multiplicative
and additive interactions were found in all symptom domain of ADHD. However, no multiplicative and additive interactions were detected between _DRD2_ rs1124491 polymorphism and PSE, nor
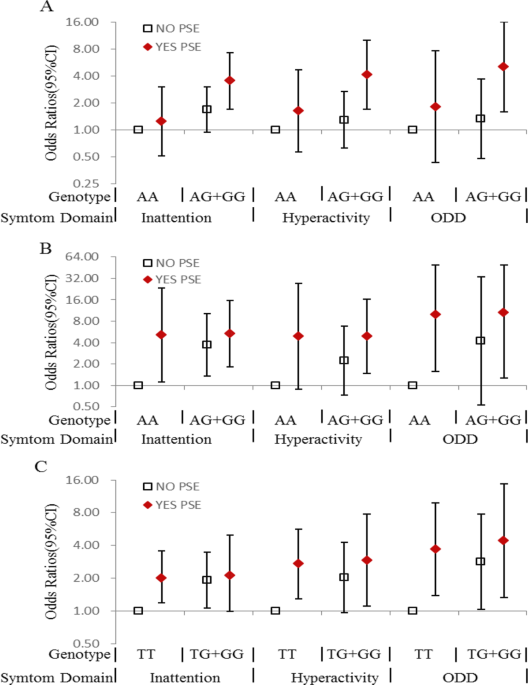
between _SLC6A4_ rs6354 polymorphism and PSE (Table 5). Figure 1 described the ORs and the 95% CIs for the only unfavorable genotype exposure, the only prenatal tobacco smoking exposure and
the joint effect of them with regard to ADHD and all symptom domains. Most of the risk genotypes showed an increased risk association with ADHD when co-existed with PSE compared with
individuals without PSE. The risk association of ADHD in _ADRA2A_ rs553668 GG or AG carrier without PSE was moderately increased (OR = 1.65, 95% CI = 0.93–2.90, _P_ = 0.084), compared with
AA carrier without PSE. But the OR for the rs553668 GG or AG carriers with PSE, was significantly increased to 3.54(95% CI: 1.73–7.25, _P_ = 0.001 Table S2). The group of _DRD2_ rs1124491
AG/GG genotype with PSE also showed a significant association with ADHD compare with whose without PSE (OR = 6.04, 95% CI = 2.07–17.65, _P_ = 0.001, Table S3). And _SLC6A4_ rs6354 GT/GG
genotype carriers with PSE also showed an increased association in hyperactivity and ADHD-ODD symptoms (hyperactivity domain: OR = 2.92, 95% CI = 1.10–7.75, _p_ = 0.031; ODD domain: OR =
4.42 95% CI = 1.32–14.79, _p_ = 0.016.Table S4). DISCUSSION The current case-control study demonstrated a significantly association of prenatal tobacco exposure with all ADHD subtype and
ADHD concurring with ODD(ADHD-ODD) in children, especially a strong association with hyperactivity and ADHD-ODD, and the effect size did not diminished even after adjusted by potential
environmental influencing covariates. In addition, the study found three SNPs of _ADRA2A_, _DRD2_ and _SLC6A4_ genes associated with ADHD, but the association disappeared in some ADHD
subtypes after adjusted by potential environmental covariates. Interestingly, when grouped with prenatal tobacco exposure, however, the association of the genetic variants and ADHD
reappeared although there are no multiplicative and additive interaction between _DRD2_, _SLC6A4_ genes and PSE. With regard to the findings in the genetic analysis, the results of risk
association with ADHD in the children carrying _ADRA2A_ rs553668 GG or AG genotype were in concordance with the findings of several studies, and indicated that rs553668, being known as the
DraI site in the 3′-untranslated region of _ADRA2A_ gene, A-to-G variant increased the risk of ADHD24,25. Meanwhile, the findings showed the _DRD2_ rs1124491 in the significant association
with inattention type of ADHD. _DRD2_ gene (Dopamine Receptor D2 gene), encodes the D2 subtype of the dopamine receptor. A population-based birth cohort have reported an association of
_DRD2_ rs1124491 with ADHD in males and low persistence in female ADHD patients26,27. Moreover, a common variant _SLC6A4_ rs6354 was identified to be in association with ADHD-ODD. _SLC6A4_
rs6354 located in the untranslated(exon 2) 5′-UTR region of _SLC6A4_ gene—a potential module of exonic splicing enhancer or silencer by bioinformatics prediction— and may affect the
expression level or exonic splicing of serotonin28. Evidences show that one repeat length polymorphism-STin2 located in the untranslated exon 2 of _SLC6A4_ gene may be significantly
associated with major depressive disorder and suicide29. A limited number of G × E studies have shown that genetic factors interact with maternal smoking to heighten risk for ADHD. Anita
Thapar30 and his colleagues found maternal smoking during pregnancy was shown a significant association with offspring ADHD symptom scores in twins study after adjustment by genetic factors,
although the main effect of cigarette exposure was small. One gene-environment interaction study evaluated maternal smoking and the _DAT_ gene. In the cases with co-exist of maternal
smoking during pregnancy and 10 R/10 R genotype of _DAT_ gene, the mean score of hyperactivity-impulsivity and inattentiveness derived from the Conners’ Parent Rating Scale were higher than
other groups22. The findings in the current study infer that the susceptibility of ADHD for the unfavorable ADHD genotypes carriers might increase when the children having the history of
in-utero exposure to cigarette smoking. However, the molecular mechanisms responsible for the interaction remain unknown. Nicotine, the main psychoactive component of tobacco, can
accumulated in human brain fast when they are smoking31. The neurotoxic effects of nicotine exposure on human fetal brain development have not been studied directly. However, a large number
of animal studies have found that nicotine has obvious neurotoxic effects on fetal brain development32. Animal models confident that the nicotine can readily cross the placental barrier into
fetal circulation, and the blood-brain barrier, which protects the adult brain from toxic chemicals, is not fully formed until about six months after birth33. So, nicotine can cross the
blood-brain barrier and specifically binds to nicotinic acetylcholine receptors (nAChRs) in the fetal brain34, and nAChRs have an important role in regulating synaptic plasticity and brain
development. Concerning of animal models, chronic nicotine exposure to animal brain developmentally leads to long-term changes of decreasing presynaptic nAChRs function, which cause altering
nicotine-stimulated release of those neurotransmitters and the altering continues for a long time even after nicotine exposure has been removed35,36. And neurotransmitters dysregulation of
acetylcholine, dopamine and serotonin are assumed to be the reason of ADHD21. The decreased presynaptic nAChRs function may increase the risks of dysfunctions of dopaminergic, serotonergic
and noradrenergic neurotransmission caused by genetic variants. That may explain the strong joint effects of prenatal tobacco exposure and genetic variants on all ADHD subtypes. But the
exact reasons of the increasing risks require more extensive research. Lead is a heavy metal that exists in the environment in nature, and it is a most widely used neurotoxicants. Many
studies have shown that high blood lead levels (≥10 µg/dL) are harmful to children neurodevelopment37,38. Moreover, evidences support that longer term low level exposure (<10 µg/dL)
associated with intellectual impairment39,40. Unfortunately, the effects of lead exposure on ADHD are less clear. In the current study, no statistically significant association was found
between low blood lead levels (<10 µg/dL) and diagnosed ADHD and all the symptoms. A growing body of evidence now support that low level exposure (<5 µg/dL) also associated with
cognitive impairment, suggesting that there is no threshold for developmental neurotoxicity37,41,42. Stephani Kim5 and his colleagues examined the relationship between blood lead levels and
ADHD in children, and found that the odds ratios for the risk of ADHD is 4.63 (95% CI: 1.36–15.72) in the “≥2 mg/dL” group and the odds ratios increased to 7.25 (1.66–31.67) in the “≥3
mg/dL” group. However, some studies reported that the association between blood lead levels and ADHD did not exhibit a dose-response relationship43. To the best of our knowledge, this paper
is the first G × E interaction research about SNPs and prenatal tobacco smoke exposure in association to ADHD and all the subtypes. The major strength of this study is the standardized
procedures of ADHD assessment in children and the precise and rigorous diagnosis21, aiming to minimize the overdiagnosis or underdiagnosis. However, several limitations have to be considered
during interpretation of the findings. The major limitation of this study is that the small sample size has decreased the power to detect the effects of the SNPs and the gene-environment
interactions. One inherent methodologic problem in this case-control design is that the retrospective assessment of PSE might introduce systematic error in the calculation of the association
between PSE and ADHD because of recall bias. In order to diminish the recall bias, we recruited the new diagnosed patients from the community survey. Although the regression model
controlled for important confounding variables such as age, gender, mother and father education, and postnatal smoke exposure status, it did not take into account other possible
environmental pollutants, such as manganese, mercury, arsenic and bisphenol A and phthalates5,44,45, which can be a focus of future research. Psychological and social environment are also
the important for child psychological development, but those did not measured in our study. This is a weakness of the study. The participants in our study were enrolled from one city of
China, which limited the results interpretation in general populations. Finally, its cross-sectional nature limits explication about the causal effects of G × E interactions. Future research
may focus on a longitudinal study to confirm the causality. METHODS PARTICIPANTS This study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science
and Technology, and all methods were performed in accordance with the approved guidelines and regulations. Informed consent was obtained from all participants and their parents. Children who
were diagnosed for ADHD by pediatric psychiatrists were recruited as the cases in the Liuzhou Women and Children Healthcare Hospital, and 6–12-year-old healthy children from 2 elementary
schools in Liuzhou City were also recruited as the controls. The exclusion criteria for both groups were: 1) a history of mental retardation, autism spectrum disorders, bipolar disorder,
language disorders or learning disabilities, pervasive developmental disorder; 2) a history of brain disease, seizure disorder, or other neurological disorders; 3) intelligence quotient (IQ)
< 70; and 4) the presence of any chronic physical disease; 5) a blood lead concentration ≥10(µg/dL). Permissions were given for the eligible patients and controls to participate in the
study, and those children whose parents could not be contacted or denied consent for participation were excluded. As a result, a total of 168 cases and 233 controls (6–12 years of age) were
recruited. ASSESSMENTS OF CHILDREN ADHD The status of both the case and control subjects were confirmed with a semi-structured clinical interview with the parents and children that was
conducted according to the DSM-IV ADHD Rating Scale by a pediatric psychiatrist. Additionally, diagnoses were made that included both in categories and severity ratings using the 26-item
Chinese version of SNAP-IV scale46. The 4-point response is scored 0–3 (Not at All = 0, Just A Little = 1, Quite a Bit = 2, and Very Much = 3) on SNAP-IV scale. Subscale scores are
calculated by summing the scores on the items in the specific symptom domains (inattention, hyperactive and ODD), in which average score 0–1 means no features, 1.1–1.5 means subclinical,
1.6–2.0 means significant, and >2.1 means very severe. We defined oppositional defiant disorder as the ODD symptom domain score ≥1.6. The Child Behavior Checklist (CBCL) scale was
conducted to evaluate child potential behavior problems and the Wechsler Intelligence Scale for Children (WISC) was used to evaluate full-scale IQ of all participants. All instruments used
in the current study are validated Chinese versions. MEASUREMENT OF BLOOD LEAD CONCENTRATIONS To measure lead concentrations in blood, 2–3 mL of whole blood was drawn from each child and
kept it in heparin-containing tubes. Blood lead level in whole blood was measured using graphite furnace atomic absorption spectrometry (Spectral AA-240FS, Varian, American). The limit of
detection for blood lead was 0.1 µg/dL. None of the blood samples showed below the limit of detection. DNA EXTRACTION AND GENOTYPING Genomic DNA was extracted from peripheral blood
leukocytes using the TIANamp® Blood DNA Kit DP318 (TIANGEN BIOTECH CO., LTD., Beijing, China). The candidate genes within the dopamine, norepinephrine and serotonin neurotransmitter pathways
were selected based on recent findings47, and included 7 genes (i.e., _SLC6A3_, _SLC6A4_, _DRD2_, _ANKK1_, _DRD4_, _ADRA2A_, _SNAP25_). The screening procedure for the candidate single
nucleotide polymorphism(SNP) was as follow: First, we searched the F-SNP database (http://compbio.cs.queensu.ca/F-SNP) to retrieve information about the predictive functions of the SNPs
within these genes and those of potential effects on splicing, transcription, translation, and post translation processes were selected. Second, we filtered the SNPs by the MAF of CHB (minor
allele frequency for Han Chinese in Beijing) in the database of 1000 genomes (https://www.ncbi.nlm.nih.gov/variation/tools/1000genomes/) and selected SNPs with MAFs > 5% for the next
step. Third, we tested the linkage disequilibrium (LD) among selected SNPs using SNAP Pairwise LD (http://www.broadinstitute.org/mpg/snap/ldsearchpw.php), and only one was reserved if
several SNPs were in strong LD with each other (_r_2 ≥ 0.80). Consequently, a total of 16 SNPs were retained. High-quality genotyping was performed on the Sequenom MassARRAY platform (San
Diego, USA) by BIO MIAO BIOLOGICAL TECHNNOLOGY (Beijing, China) following the standard experimental procedures from the manufacturer. In addition, samples with a call rate <80% or
Hardy-Weinberg equilibrium (HWE) < 0.05 in the control group were removed. DETERMINATION OF TOBACCO EXPOSURE Tobacco exposure status was obtained from the children’s parents by a
questionnaire. The questions were constructed in two parts: mother tobacco exposure and child secondhand smoke exposure. Firstly, we asked whether the mother smoked before pregnancy or not
(>100 cigarettes) and whether she smoked during pregnancy. If yes, we then asked how many cigarette expensed per day. Only three of the mothers reported being an ex-smoker or having
smoked during pregnancy. Besides, we inquired whether or not she was exposed to secondhand smoke during pregnancy at home or in the workplace and how long she stayed in the smoking
circumstance per day/week. Secondly, we investigated whether any family members smoked at home after the child birth and how many cigarette the members expensed per day/week. CONFOUNDERS AND
COVARIATES A face-to-face questionnaire survey was administered for their parents by a trained interviewer to collect socio-demographic variables, prenatal and perinatal characteristics.
Socio-demographic variables included age, gender, and parental marital status (categorized as married, or single, separated, divorced and widowed). Prenatal and perinatal characteristics
included birth weight, pregnancy age of mother, preterm birth and the mode of delivery (cesarean section or vaginal delivery). The family history of neural system diseases and ADHD were
asked additionally, but no participant declared of ADHD family history in their families. STATISTICAL ANALYSIS Differentials in the distribution of socio-demographic variables, prenatal and
perinatal characteristics between patients and controls were compared by chi-squared test or _t_ test, when appropriate. Hardy-Weinberg equilibrium (HWE) for genotypes was calculated in
controls by a goodness-of-fit chi-squared test. Logistic regression analysis was used to estimate the effect of PSE and genotype frequencies on ADHD susceptibility by computing odds ratios
(ORs) and 95% confidence intervals (95% CIs). Four inheritance models (codominant, dominant, additive and recessive models) were estimated for each SNP. Meanwhile, the statistical power to
detect the effects of the SNPs was calculated by Power v3.0.048,49, and for SNPs with MAF of 0.11(rs6354), 0.43(rs1124491), and 0.44(rs553668), for example, we calculated that the power for
our sample size to detect an OR of 1.50 was 43.6, 74.1 and 74.8%, respectively. The Multifactor Dimensionality Reduction (MDR) 2.0 beta 8.1 program (https://sourceforge.net/projects/mdr/)
was used to assess the gene-environment interactions between risk genes and the environmental risks. The details analytic protocol was described in the previous study50,51. Furthermore,
multiplicative and additive interactions were computed. Multiplicative interaction was evaluated by the interaction term of logistic regression model. Synergy index (SI), attributable
proportion due to interaction (AP), and relative excess risk due to interaction (RERI) and their corresponding 95% CIs were calculated by additive interaction analysis, as suggested by Tomas
Andersson52. If there is no additive interaction, RERI and AP are equal to 0, or SI are equal to 1. The multiplicative and additive interaction analyses were adjusted for age of the child,
gender, pregnancy age of mother, and postnatal smoking exposure. Since a higher proportion of males and younger ADHD children(<9 years old) was noted in our study. All analysis were
performed using SPSS version 22.0 software (SPSS Inc., Chicago, Illinois, USA). All tests were two-tailed, and statistical significance was defined at _P_ < 0.05. REFERENCES * Thomas, R.,
Sanders, S., Doust, J., Beller, E. & Glasziou, P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. _Pediatrics_ 135, e994–1001,
https://doi.org/10.1542/peds.2014-3482 (2015). Article PubMed Google Scholar * Wang, T. _et al_. Prevalence of attention deficit/hyperactivity disorder among children and adolescents in
China: a systematic review and meta-analysis. _BMC Psychiatry_ 17, 32, https://doi.org/10.1186/s12888-016-1187-9 (2017). Article PubMed PubMed Central Google Scholar * Jin, J. _et al_.
The divergent impact of COMT Val158Met on executive function in children with and without attention-deficit/hyperactivity disorder. _Genes, brain, and behavior_ 15, 271–279,
https://doi.org/10.1111/gbb.12270 (2016). Article CAS PubMed Google Scholar * Harpin, V. A. The effect of ADHD on the life of an individual, their family, and community from preschool to
adult life. _Arch Dis Child_ 90(Suppl 1), i2–7, https://doi.org/10.1136/adc.2004.059006 (2005). Article PubMed PubMed Central Google Scholar * Kim, S. _et al_. Lead, mercury, and
cadmium exposure and attention deficit hyperactivity disorder in children. _Environ Res_ 126, 105–110, https://doi.org/10.1016/j.envres.2013.08.008 (2013). Article CAS PubMed Google
Scholar * Faraone, S. V. _et al_. Molecular genetics of attention-deficit/hyperactivity disorder. _Biol Psychiatry_ 57, 1313–1323, https://doi.org/10.1016/j.biopsych.2004.11.024 (2005).
Article CAS PubMed Google Scholar * Faraone, S. V. & Mick, E. Molecular genetics of attention deficit hyperactivity disorder. _The Psychiatric clinics of North America_ 33, 159–180,
https://doi.org/10.1016/j.psc.2009.12.004 (2010). Article PubMed PubMed Central Google Scholar * Yang, L. _et al_. Polygenic transmission and complex neuro developmental network for
attention deficit hyperactivity disorder: genome-wide association study of both common and rare variants. _American journal of medical genetics. Part B, Neuropsychiatric genetics: the
official publication of the International Society of Psychiatric Genetics_ 162B, 419–430, https://doi.org/10.1002/ajmg.b.32169 (2013). Article CAS Google Scholar * Brookes, K. _et al_.
The analysis of 51 genes in DSM-IV combined type attention deficit hyperactivity disorder: association signals in DRD4, DAT1 and 16 other genes. _Molecular Psychiatry_ 11, 934–953,
https://doi.org/10.1038/sj.mp.4001869 (2006). Article CAS PubMed Google Scholar * Lasky-Su, J. _et al_. Genome-wide association scan of quantitative traits for attention deficit
hyperactivity disorder identifies novel associations and confirms candidate gene associations. _American journal of medical genetics. Part B, Neuropsychiatric genetics: the official
publication of the International Society of Psychiatric Genetics_ 147B, 1345–1354, https://doi.org/10.1002/ajmg.b.30867 (2008). Article CAS Google Scholar * Lundwall, R. A. &
Dannemiller, J. L. Genetic contributions to attentional response time slopes across repeated trials. _BMC neuroscience_ 16, 66, https://doi.org/10.1186/s12868-015-0201-3 (2015). Article CAS
PubMed PubMed Central Google Scholar * Bissonette, G. B. & Roesch, M. R. Editorial: Neural Circuitry of Behavioral Flexibility: Dopamine and Related Systems. _Frontiers in
behavioral neuroscience_ 10, 6, https://doi.org/10.3389/fnbeh.2016.00006 (2016). Article PubMed PubMed Central Google Scholar * Ettinger, U., Merten, N. & Kambeitz, J. Meta-analysis
of the association of the SLC6A3 3′-UTR VNTR with cognition. _Neuroscience and biobehavioral reviews_ 60, 72–81, https://doi.org/10.1016/j.neubiorev.2015.09.021 (2016). Article CAS PubMed
Google Scholar * Swanson, J. M. _et al_. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine
hypothesis. _Neuropsychol Rev_ 17, 39–59, https://doi.org/10.1007/s11065-007-9019-9 (2007). Article PubMed Google Scholar * Hvolgaard Mikkelsen, S., Olsen, J., Bech, B. H. & Obel, C.
Parental age and attention-deficit/hyperactivity disorder (ADHD). _International journal of epidemiology_ 46, 409–420, https://doi.org/10.1093/ije/dyw073 (2016). Article Google Scholar *
Halmoy, A., Klungsoyr, K., Skjaerven, R. & Haavik, J. Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. _Biol Psychiatry_ 71, 474–481,
https://doi.org/10.1016/j.biopsych.2011.11.013 (2012). Article PubMed Google Scholar * Ruisch, I. H., Dietrich, A., Glennon, J. C., Buitelaar, J. K. & Hoekstra, P. J. Maternal
substance use during pregnancy and offspring conduct problems: A meta-analysis. _Neurosci Biobehav Rev_, https://doi.org/10.1016/j.neubiorev.2017.08.014 (2017). * Goodwin, R. D. _et al_.
Serious Psychological Distress and Smoking During Pregnancy in the United States: 2008–2014. _Nicotine Tob Res_ 19, 605–614, https://doi.org/10.1093/ntr/ntw323 (2017). Article PubMed
PubMed Central Google Scholar * Kotimaa, A. J. _et al_. Maternal Smoking and Hyperactivity in 8-Year-Old Children. _Journal of the American Academy of Child & Adolescent Psychiatry_
42, 826–833, https://doi.org/10.1097/01.CHI.0000046866.56865.A2 (2003). Article Google Scholar * Joo, H. _et al_. Secondhand Smoke Exposure and Low Blood Lead Levels in Association With
Attention-Deficit Hyperactivity Disorder and Its Symptom Domain in Children: A Community-Based Case-Control Study. _Nicotine Tob Res_ 19, 94–101, https://doi.org/10.1093/ntr/ntw152 (2017).
Article CAS PubMed Google Scholar * Thapar, A. & Cooper, M. Attention deficit hyperactivity disorder. _The Lancet_ 387, 1240–1250, https://doi.org/10.1016/s0140-6736(15)00238-x
(2016). Article Google Scholar * Kahn, R. S., Khoury, J., Nichols, W. C. & Lanphear, B. P. Role of dopamine transporter genotype and maternal prenatal smoking in childhood
hyperactive-impulsive, inattentive, and oppositional behaviors. _The Journal of Pediatrics_ 143, 104–110, https://doi.org/10.1016/s0022-3476(03)00208-7 (2003). Article PubMed Google
Scholar * Asherson, P. & Consortium, I. Attention-Deficit Hyperactivity Disorder in the post-genomic era. _European child & adolescent psychiatry_ 13(Suppl 1), I50–70,
https://doi.org/10.1007/s00787-004-1006-6 (2004). Article Google Scholar * Unal, D., Unal, M. F., Alikasifoglu, M. & Cetinkaya, A. Genetic Variations in Attention Deficit Hyperactivity
Disorder Subtypes and Treatment Resistant Cases. _Psychiatry Investig_ 13, 427–433, https://doi.org/10.4306/pi.2016.13.4.427 (2016). Article PubMed PubMed Central Google Scholar * Cho,
S. C. _et al_. Possible association of the alpha-2A-adrenergic receptor gene with response time variability in attention deficit hyperactivity disorder. _Am J Med Genet B Neuropsychiatr
Genet_ 147B, 957–963, https://doi.org/10.1002/ajmg.b.30725 (2008). Article CAS PubMed Google Scholar * Nyman, E. S. _et al_. ADHD Candidate Gene Study in a Population-Based Birth Cohort:
Association with DBH and DRD2. _Journal of the American Academy of Child & Adolescent Psychiatry_ 46, 1614–1621, https://doi.org/10.1097/chi.0b013e3181579682 (2007). Article Google
Scholar * Nyman, E. S. _et al_. Sex-specific influence of DRD2 on ADHD-type temperament in a large population-based birth cohort. _Psychiatr Genet_ 22, 197–201,
https://doi.org/10.1097/YPG.0b013e32834c0cc8 (2012). Article CAS PubMed Google Scholar * Lovejoy, E. A., Scott, A. C., Fiskerstrand, C. E., Bubb, V. J. & Quinn, J. P. The serotonin
transporter intronic VNTR enhancer correlated with a predisposition to affective disorders has distinct regulatory elements within the domain based on the primary DNA sequence of the repeat
unit. _The European journal of neuroscience_ 17, 417–420 (2003). Article CAS Google Scholar * Rao, S. _et al_. Resequencing three candidate genes discovers seven potentially deleterious
variants susceptibility to major depressive disorder and suicide attempts in Chinese. _Gene_ 603, 34–41, https://doi.org/10.1016/j.gene.2016.12.006 (2017). Article CAS PubMed Google
Scholar * Anita Thapar _et al_. Maternal Smoking During Pregnancy and Attention Deficit Hyperactivity Disorder Symptoms in Offspring. _Am J Psychiatry_ 160, 1985–1989 (2003). Article
Google Scholar * Rose, J. E. _et al_. Kinetics of brain nicotine accumulation in dependent and nondependent smokers assessed with PET and cigarettes containing 11C-nicotine. _Proc Natl Acad
Sci USA_ 107, 5190–5195, https://doi.org/10.1073/pnas.0909184107 (2010). Article ADS PubMed Google Scholar * King, E., Campbell, A., Belger, A. & Grewen, K. Prenatal Nicotine
Exposure Disrupts Infant Neural Markers of Orienting. _Nicotine Tob Res_, https://doi.org/10.1093/ntr/ntx177 (2017). * Luck, W., Nau, H., Hansen, R. & Steldinger, R. Extent of nicotine
and cotinine transfer to the human fetus, placenta and amniotic fluid of smoking mothers. _Developmental pharmacology and therapeutics_ 8, 384–395 (1985). Article CAS Google Scholar *
Carter, S., Paterson, J., Gao, W. & Iusitini, L. Maternal smoking during pregnancy and behaviour problems in a birth cohort of 2-year-old Pacific children in New Zealand. _Early Hum Dev_
84, 59–66, https://doi.org/10.1016/j.earlhumdev.2007.03.009 (2008). Article PubMed Google Scholar * Damborsky, J. C., Griffith, W. H. & Winzer-Serhan, U. H. Neonatal nicotine
exposure increases excitatory synaptic transmission and attenuates nicotine-stimulated GABA release in the adult rat hippocampus. _Neuropharmacology_ 88, 187–198,
https://doi.org/10.1016/j.neuropharm.2014.06.010 (2015). Article CAS PubMed Google Scholar * Gold, A. B., Keller, A. B. & Perry, D. C. Prenatal exposure of rats to nicotine causes
persistent alterations of nicotinic cholinergic receptors. _Brain Res_ 1250, 88–100, https://doi.org/10.1016/j.brainres.2008.10.076 (2009). Article CAS PubMed Google Scholar * Kim, Y.
_et al_. Association between blood lead levels (<5 mug/dL) and inattention-hyperactivity and neurocognitive profiles in school-aged Korean children. _Sci Total Environ_ 408, 5737–5743,
https://doi.org/10.1016/j.scitotenv.2010.07.070 (2010). Article ADS CAS PubMed Google Scholar * Nicolescu, R. _et al_. Environmental exposure to lead, but not other neurotoxic metals,
relates to core elements of ADHD in Romanian children: performance and questionnaire data. _Environ Res_ 110, 476–483, https://doi.org/10.1016/j.envres.2010.04.002 (2010). Article CAS
PubMed Google Scholar * Lanphear, B. P. & Bearer, C. F. Biomarkers in paediatric research and practice. _Arch Dis Child_ 90, 594–600, https://doi.org/10.1136/adc.2003.048819 (2005).
Article CAS PubMed PubMed Central Google Scholar * Heyer, D. B. & Meredith, R. M. Environmental toxicology: Sensitive periods of development and neurodevelopmental disorders.
_Neurotoxicology_ 58, 23–41, https://doi.org/10.1016/j.neuro.2016.10.017 (2017). Article CAS PubMed Google Scholar * Nigg, J., Nikolas, M. & Burt, S. A. Measured gene-by-environment
interaction in relation to attention-deficit/hyperactivity disorder. _J Am Acad Child Adolesc Psychiatry_ 49, 863–873, https://doi.org/10.1016/j.jaac.2010.01.025 (2010). Article PubMed
PubMed Central Google Scholar * Cho, S. C. _et al_. Effect of environmental exposure to lead and tobacco smoke on inattentive and hyperactive symptoms and neurocognitive performance in
children. _J Child Psychol Psychiatry_ 51, 1050–1057, https://doi.org/10.1111/j.1469-7610.2010.02250.x (2010). Article PubMed Google Scholar * Huang, S. _et al_. Childhood Blood Lead
Levels and Symptoms of Attention Deficit Hyperactivity Disorder (ADHD): A Cross-Sectional Study of Mexican Children. _Environ Health Perspect_ 124, 868–874,
https://doi.org/10.1289/ehp.1510067 (2016). Article CAS PubMed Google Scholar * Liu, W. _et al_. S100beta in heavy metal-related child attention-deficit hyperactivity disorder in an
informal e-waste recycling area. _Neurotoxicology_ 45, 185–191, https://doi.org/10.1016/j.neuro.2014.10.013 (2014). Article CAS PubMed Google Scholar * Hu, D. _et al_. Associations of
phthalates exposure with attention deficits hyperactivity disorder: A case-control study among Chinese children. _Environ Pollut_ 229, 375–385, https://doi.org/10.1016/j.envpol.2017.05.089
(2017). Article CAS PubMed Google Scholar * Swanson, J. M. _et al_. Clinical Relevance of the Primary Findings of the MTA: Success Rates Based on Severity of ADHD and ODD Symptoms at the
End of Treatment. _Journal of the American Academy of Child & Adolescent Psychiatry_ 40, 168–179, https://doi.org/10.1097/00004583-200102000-00011 (2001). Article CAS Google Scholar
* Kamradt, J. M., Nigg, J. T., Friderici, K. H. & Nikolas, M. A. Neuropsychological performance measures as intermediate phenotypes for attention-deficit/hyperactivity disorder: A
multiple mediation analysis. _Development and psychopathology_, 1–14, https://doi.org/10.1017/S0954579416000195 (2016). * Foppa, I. & Spiegelman, D. Power and sample size calculations
for case-control studies of gene-environment interactions with a polytomous exposure variable. _American journal of epidemiology_ 146, 596–604 (1997). Article CAS Google Scholar *
Garcia-Closas, M. & Lubin, J. H. Power and sample size calculations in case-control studies of gene-environment interactions: comments on different approaches. _American journal of
epidemiology_ 149, 689–692 (1999). Article CAS Google Scholar * Hahn, L. W., Ritchie, M. D. & Moore, J. H. Multifactor dimensionality reduction software for detecting gene-gene and
gene-environment interactions. _Bioinformatics (Oxford, England)_ 19, 376–382 (2003). Article CAS Google Scholar * Das, M. _et al_. Role of gene-gene/gene-environment interaction in the
etiology of eastern Indian ADHD probands. _Progress in neuro-psychopharmacology & biological psychiatry_ 35, 577–587, https://doi.org/10.1016/j.pnpbp.2010.12.027 (2011). Article CAS
Google Scholar * Andersson, T., Alfredsson, L., Källberg, H., Zdravkovic, S. & Ahlbom, A. Calculating measures of biological interaction. _European Journal of Epidemiology_ 20, 575–579,
https://doi.org/10.1007/s10654-005-7835-x (2005). Article PubMed Google Scholar Download references ACKNOWLEDGEMENTS We thank the study participants and their parents. We also
acknowledge the collaboration of the staff of the Liuzhou maternal and child care hospital. This work was supported by the Fundamental Research Funds for the Central Universities (Grand
number:lzujbky-2017–87). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Maternal and Child Health, School of Public Health, Tongji Medical College, Huazhong University of
Science and Technology, Wuhan, Hubei, P. R. China Yanni Wang, Wenjing Chen & Yukai Du * Department of Child Health Care, Hospital of Maternal and Child Health of Dalian, Dalian,
Liaoning, P. R. China Dan Hu * Department of Maternal, Child and Adolescent Health, School of Public Health, Lanzhou University, Lanzhou, Gansu, P. R. China Yanni Wang & Hongli Xue
Authors * Yanni Wang View author publications You can also search for this author inPubMed Google Scholar * Dan Hu View author publications You can also search for this author inPubMed
Google Scholar * Wenjing Chen View author publications You can also search for this author inPubMed Google Scholar * Hongli Xue View author publications You can also search for this author
inPubMed Google Scholar * Yukai Du View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS All authors in the manuscript who have made substantial
contributions to the work. Yanni Wang designed the study did the statistical analysis, and drafted the initial manuscript. Dan Hu helped to design the study, collected the data. Wenjing Chen
assisted with data collection, Hongli Xue did the lab work. Yukai Du designed the study, directed the statistical analysis, and reviewed the manuscript. CORRESPONDING AUTHOR Correspondence
to Yukai Du. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY TABLE RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a
Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit
to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are
included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and
your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this
license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Wang, Y., Hu, D., Chen, W. _et al._ Prenatal Tobacco Exposure
Modulated the Association of Genetic variants with Diagnosed ADHD and its symptom domain in children: A Community Based Case–Control Study. _Sci Rep_ 9, 4274 (2019).
https://doi.org/10.1038/s41598-019-40850-w Download citation * Received: 14 June 2018 * Accepted: 25 February 2019 * Published: 12 March 2019 * DOI:
https://doi.org/10.1038/s41598-019-40850-w SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Jonathan majors’ former girlfriend granted full temporary order of protectionby CEDRIC 'BIG CED' THORNTON April 28, 2023 ------------------------- In the latest development of the domesti...
5 tips to figure out if a tech company on the stock market is an ethical investmentThe authors do not work for, consult, own shares in or receive funding from any company or organisation that would benef...
cody ellingham captures the nocturnal neon cityscape of bangkok in photography seriesduring the auspicious july heat of the buddhist holiday ‘asalha puja’, new zealand photographer cody ellingham landed in...
Cma letter to santander on ppi annual review statementsCorrespondence CMA LETTER TO SANTANDER ON PPI ANNUAL REVIEW STATEMENTS Letter to Santander UK plc about its non-complian...
AARP Works to Protect Women’s Retirement SavingsAARP; (Getty Images 2) Facebook Twitter LinkedIn Women often earn less money than men throughout their careers and are m...
Latests News
Prenatal tobacco exposure modulated the association of genetic variants with diagnosed adhd and its symptom domain in children: a community based caseABSTRACT The purpose of our study was to test the hypothesis that prenatal tobacco smoking exposure (PSE) could modulate...
Everything going to the dogs? Keep calm and carry on — like the queen | thearticleEvents, dear boy? No: it’s all about trends. Harold Macmillan’s gnomic (and apocryphal) saying has been firmly knocked o...
Why luxury branded residences are booming in apac and beyondThe branded residence juggernaut continues unabated, bringing more privileges to the well-heeled in ever more diverse lo...
St Petersburg Ballet coming to The Venetian in MacauAdvertisementCultureSt Petersburg Ballet coming to The Venetian in Macau Dancer Irina Kolesnikova is behind the success ...
Massive online open courses see exponential growth during covid-19 pandemicMassive open online classes, or MOOCs, have seen a surge in enrollments since March. Enrollment at Coursera – an online ...