Visual simulators replicate vision with multifocal lenses
Visual simulators replicate vision with multifocal lenses"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Adaptive optics (AO) visual simulators based on deformable mirrors, spatial light modulators or optotunable lenses are increasingly used to simulate vision through different
multifocal lens designs. However, the correspondence of this simulation with that obtained through real intraocular lenses (IOLs) tested on the same eyes has not been, to our knowledge,
demonstrated. We compare through-focus (TF) optical and visual quality produced by real multifocal IOLs (M-IOLs) -bifocal refractive and trifocal diffractive- projected on the subiect’s eye
with those same designs simulated with a spatial light modulator (SLM) or an optotunable lens working in temporal multiplexing mode (SimVis technology). Measurements were performed on 7
cyclopleged subjects using a custom-made multichannel 3-active-optical-elements polychromatic AO Visual Simulator in monochromatic light. The same system was used to demonstrate performance
of the real IOLs, SLM and SimVis technology simulations on bench using double-pass imaging on an artificial eye. Results show a general good correspondence between the TF performance with
the real and simulated M-IOLs, both optically (on bench) and visually (measured visual acuity in patients). We demonstrate that visual simulations in an AO environment capture to a large
extent the individual optical and visual performance obtained with real M-IOLs, both in absolute values and in the shape of through-focus curves. SIMILAR CONTENT BEING VIEWED BY OTHERS
SIMULATION OF DAILY SOFT MULTIFOCAL CONTACT LENSES USING SIMVIS GEKKO: FROM IN-VITRO AND COMPUTATIONAL CHARACTERIZATION TO CLINICAL VALIDATION Article Open access 13 April 2024 ANALYSIS AND
COMPARISON OF MONOFOCAL, EXTENDED DEPTH OF FOCUS AND TRIFOCAL INTRAOCULAR LENS PROFILES Article Open access 23 May 2022 OPTICAL AND CLINICAL SIMULATED PERFORMANCE OF A NEW REFRACTIVE
EXTENDED DEPTH OF FOCUS INTRAOCULAR LENS Article Open access 05 April 2024 INTRODUCTION Adaptive Optics (AO), a technology originally developed to image stellar objects with ground-based
telescopes eliminating the degrading effects of the atmospheric turbulence1, has more recently expanded applications into microscopy2 and ophthalmology3,4. Fundus cameras and scanning laser
ophthalmoscopes provided with AO have allowed imaging of individual photoreceptor cells and microscopic structures in the retina. Conversely, AO has allowed probing the visual system under
manipulated optics5,6,7,8, either with fully corrected optical aberrations9, through the optical aberrations of another subject or scaled versions of their own10,11, or a phase pattern
simulating a given correction (i.e. an intraocular lens, contact lens or a corneal treatment)5,12. AO visual simulators are particularly attractive to test vision in patients with new
optical designs6,13 prior to delivering surgical corrections to the patient or even manufacturing the lenses. Simulations of new corrections with adaptive optics primarily serve to
investigate interactions between the patient’s optics and a given correction, to investigate differences across corrections, and eventually to select the correction that optimizes perceived
visual quality and performance in patients5,12,14. Providing patients the visual experience before implanting an intraocular lens or fitting a contact lens is particularly relevant for
multifocal corrections for presbyopia (the age-related loss of the ability to dynamically focus near and far objects)15. Multifocal corrections work under the principle of simultaneous
vision, projecting simultaneously focused and defocused images on the retina. These corrections generally provide multifocality at the expense of reducing optical quality at all distances.
There are several multifocal designs, working on refractive or diffractive principles, including refractive bifocal concentric or angular designs, diffractive bifocal and trifocal designs,
and extended depth of focus designs with smooth refractive profiles or hybrid refractive-diffractive designs16. Visual simulators allow undertaking systematic studies of visual performance
testing multiple lens designs (programmable in the adaptive optics active element), which can be directly compared by the patient. As clinical instruments, AO visual simulators can help
demonstrating the patient the experience of multifocality and can guide the patient and eye care practitioner in the selection of the most suitable correction. In AO-based visual simulators,
an active optical element (deformable mirror, spatial light modulator, or optotunable lens) reproduces the equivalent phase map of a certain optical design in a plane conjugate to the
subject’s pupil plane, while the observer is looking at a visual stimulus. Deformable Mirrors (DM) allow simulating smooth optical designs, or to induce certain amounts of aberrations, while
controlling the aberrations of the subject. DMs have been used, for example, to evaluate the effects of inducing spherical aberration17,18, or combinations of astigmatism and coma on
through-focus (TF) visual performance19. In contrast, spatial light modulators (SLMs)5,20,21,22, generally liquid crystal-based on silicon (LCoS)-SLMs devices, are capable of reproducing
abrupt phase maps due to their high spatial resolution, and to increase the effective phase range through the use of wrapped phase representations23,24. In prior work, we have studied
perceived visual quality at far, intermediate and near distances with SLMs simulating bifocal, trifocal and tetrafocal, angular and radially segmented corrections5,12,25. Other studies have
also used SLMs to simulate the effect of corneal inlays26 and to map diffractive optics9,27. Reflective-DM or SLM-based visual simulators are mostly limited to experimental environments,
given their relatively high complexity and dimensions, although some have made their way into commercial products28,29. In these devices the visual experience is limited to stimuli projected
in a display, subtending a relatively small (typically <2 degree) visual field, in many cases monocularly3. Ideal visual simulators in a clinical environment should be see-through,
allowing a direct view of the real world and should display a larger visual field. Visual simulators of bifocal corrections, with two optical channels superimposing two images using a
transmission SLM to simulate different pupillary masks, have been used on clinical subjects13, but still remain in a laboratory setting. Deformable multi-actuator lenses have been recently
released, which may be suitable to reproduce smooth surface-varying multifocal optics, although, to our knowledge, they have not been yet used in visual simulators30, and won’t be capable of
mapping diffractive or segmented optics. An interesting novel approach to simultaneous vision simulation is the use of optotunable lenses working in temporal multiplexing mode, a technology
developed by our group (SimVis technology), described in detail in previous publications14,31. The tunable lens scans multiple foci to provide superimposed images on the retina, all of them
with the same position and magnification, but corresponding to different planes in focus. These custom electronically driven lenses can produce fast periodic foci variations at speeds
greater than the flicker fusion threshold of the human visual system, delivering seemingly static images on the subject’s retina that emulate the effect of the multifocal correction. The
simulation of multifocal corrections relies on evaluating the TF energy distribution of the correction, from the knowledge of the spatially varying pupillary power distribution, and
programming in the optotunable lens the corresponding time-varying focus changes. The simulated multifocal correction is tuned to match the TF optical quality (in terms of Visual Strehl)32
of real existing multifocal lenses. It is an optimization of the electrical input signal driving the tunable lens and, consequently, of the SimVis technology TF optical quality31. Real
multifocal intraocular lens (M-IOL) designs are therefore temporally mapped by evaluating the corresponding temporal profile of the optical power of a tunable lens that results in a TF
optical quality matching the TF optical quality of the M-IOL. While symmetric MIOL designs can be fully captured using a temporal pattern, some limitations are expected for asymmetric
complex designs. The goal of this study is to compare on real subjects, for the first time to our knowledge, TF optical and visual quality produced by real M-IOLs and visual simulations of
those multifocal designs using two different active optical elements, a spatial light modulator (SLM) and temporal multiplexing with optotunable lenses (SimVis technology), all of them
incorporated in a polychromatic AO Visual Simulator. RESULTS TF optical quality (double-pass aerial retinal point images and E-letter stimulus images, on-bench) and visual acuity (VA), in 7
patients, were measured with two M-IOLs: a bifocal refractive segmented IOL, Bi-R, and a trifocal diffractive IOL, Tri-D. Those corrections, of complex design, were tested in a polychromatic
AO visual simulator for 3 different conditions: the real lens, simulations in a SLM, and simulations using SimVis technology. All measurements were performed monocularly, in green light
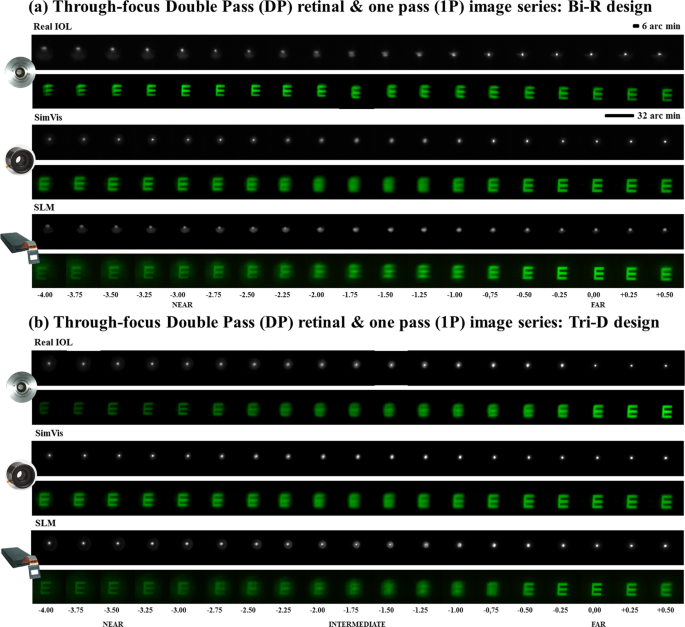
(555 nm) and for 5-mm pupils. ON-BENCH TESTS Figure 1(a,b) shows TF double-pass (DP) aerial images and E-letter images (1P) obtained on-bench with the three simulating conditions, real IOL,
SimVis technology and SLM, for (a) bifocal refractive segmented lens, Bi-R, and (b) the trifocal diffractive lens, Tri-D. Qualitatively, the replication of the images with the simulators is
highest around the foci for both simulators. Also, the asymmetric bifocal design (Bi-R) produces an asymmetry in the PSF (reminiscent of vertical coma33), which is apparent with real IOL and
SLM, but cannot be reproduced with SimVis. Figure 2 shows TF optical quality metrics obtained from the on-bench images series: (a) full width at half-maximum (FWHM) for the double-pass
images and (b) image correlation metric for the TF E-letter images, with the different multifocal designs (Blue lines: real IOL; red lines: SimVis; yellow lines: SLM)). In addition, the TF
curve obtained from on-bench image series for a monofocal condition (no multifocal design) are shown (grey lines) for the TF DP and the 1P image series. TF DP images were normalized to the 0
D monofocal image series, so that FWHM = 1 at 0.0 D for the monofocal curve, while 1P image series were correlated to the image of 0.0 D of the monofocal TF range, where image correlation
was 1 for the monofocal image at 0.0 D. There is a good correspondence between both the double-pass images and 1P image series across all simulating conditions in the position of best near
and far focus (Bifocal: 0.0 D for far vision, +3.00 D addition for near vision; Trifocal: 0.0 D for far vision, +1.75 D addition for intermediate vision and +3.50 D addition for near
vision). RMS TF difference in the TF curves (5-D range) between the real multifocal IOL and the simulation was taken as a metric for the quality of the simulation. Figure 3 compares the RMS
TF difference for SimVis technology (red bars) and SLM (yellow bars) for the two analyzed optical quality metrics: TF DP aerial retinal image curves (a) –data from Fig. 2a, and for TF 1P
E-optotype image (b) correlation curves –data from Fig. 2b. In both cases, the RMS TF difference is below 0.07, and as low as 0.01-0.02 in some conditions. When comparing both simulating
techniques, the RMS TF difference between SLM and SimVis technology TF curves is statistically significant only for Tri-D design with both TF optical quality metrics (paired-samples t-test:
TF 1P, t = 2.70, p = 0.014; TF DP, t = −2.90, p = 0.008). When comparing both designs, the RMS TF difference between Bi-R and Tri-D TF curves is significantly different for SLM (TF 1P;
paired-samples t-test: t = −4.10, p = 0.01) and for SimVis technology (TF DP; paired-samples t-test: t = −2.40, p = 0.025), while there is no significant differences between them for SimVis
technology (TF 1P) and SLM (TF DP). THROUGH FOCUS VISUAL ACUITY Figure 4 shows the TF decimal VA for the 7 subjects participating in the study and the 4 conditions measured (no lens, real
IOL, SimVis technology, and SLM) for the two simulated designs: (a) Bi-R and (b) Tri-D in a 5.00 D range. The last plot in each panel represents the averaged data across subjects (bottom,
right. VA measurements are highly repeatable (averaged standard deviation: 0.03 ± 0.005). TF VA curves showed individual similarity across simulations (either using SimVis technology or SLM)
and real IOLs in all 7 subjects. VA obtained through the real IOLs correlated statistically with those obtained through SimVis technology (r = 0.71 and r = 0.46; p < 0.05 across
subjects, for Bi-R and Tri-D, respectively) and SLM (r = 0.46 and r = 0.56; p < 0.05 across subjects for Bi-R and Tri-D, respectively). Averaged data showed a good agreement between the
TF curves. A mixed model analysis for repeated measurements was performed to investigate differences in outcomes for the two simulation techniques in comparison with Real IOLs TF
performance, for both designs (Bi-R & Tri-D). The analysis showed no significant differences for any of the simulators when using as factors the TF performance and the simulator for both
designs (Bi-R p = 0.911 & Tri-D p = 0.504), indicating that while there may be differences between the curves point by point, the general shape of the TF curves is preserved. Figure 5
shows the RMS TF difference between the TF curves for the real IOL and both SimVis technology and SLM. The average RMS TF difference of the simulated Bi-R design with respect to the real
Bi-R IOL was 0.11 ± 0.02 for the SimVis technology & 0.11 ± 0.02 for the SLM. The average RMS TF difference for Tri-D was 0.13 ± 0.016 for the SimVis technology & 0.13 ± 0.02 for the
SLM, respectively. The differences across simulators are not statistically different (paired-samples t-test: Bi-R, t = −0.81, p = 0.46; Tri-D, t = −0.45, p = 0.67). The differences between
both designs (Bi-R and Tri-D) for real IOLs and the different simulations are statistically different for the SimVis technology (paired-samples t-test: t = −2.29, p = 0.04), but not for the
SLM. On average, RMS TF difference in subjects was higher for Tri-D than for Bi-R, in line with results from the on-bench measurements previously described. On the other hand, different
multifocal designs produce different TF performances on the same subject (average RMS TF difference of 0.11 ± 0.01, 0.14 ± 0.04, and 0.12 ± 0.02 for real IOLs, SimVis technology and SLM,
respectively between the two IOL designs). DISCUSSION AO visual simulators based on different active optical elements are increasingly used to simulate vision through different multifocal
lens designs. However, the correspondence of this simulation with the vision obtained through the physically manufactured real IOLs tested on the same eyes had not been, to our knowledge,
demonstrated. In this study, we compared for the first time TF optical and visual quality produced by real M-IOLs with visual simulations using a spatial light modulator (SLM) or an
optotunable lens working in temporal multiplexing mode (SimVis technology), in monochromatic light. We found a general good correspondence between the through-focus performance with the real
and simulated M-IOLs, both optically (on bench) and visually (measured VA in patients). We did not find a bias for higher reproducibility of the TF performance towards a particular type of
simulator, although the very different principles of operation may favor one or the other depending on the design of the lens or the stimuli. For example, the temporal patterns for SimVis
technology are programmed using the TF Visual Strehl performance of the theoretical lens as a target, and the results on patients demonstrate that it captures adequately the TF visual
performance (and the optical image quality using a FWHM metric). However, as SimVis technology is limited to represent symmetric patterns, the blur produced on the images is invariably
symmetric, which may be the reason for the discrepancies in the appearance of the E-optotype images (particularly those between foci) in the SimVis technology simulation (showing symmetric,
more degrading, blur) compared to the real IOL or the SLM (where the asymmetric blur appears to be less noticeable) Fig. 1(a)31. Also, measurements were performed monochromatically. While
SimVis technology is not affected by chromatic aberration and the temporal patterns could be programmed to modify the effects of chromatic aberration on the TF visual Strehl curve that
serves as a template for SimVis technology, SLMs are largely affected by chromatic artifacts34, as the phase map is in fact only representative of one single wavelength. This is of great
importance in novel diffractive M-IOL designs, where chromatic aberration is used to generate the multifocal component of the lens35, thus the SLM pattern and SimVis technology signal would
need to be modified accordingly. Since capturing the specific chromatic effects of the diffractive lenses pose a challenge in SLM-based simulators, it is likely that measurements with
polychromatic stimuli (instead of the green stimuli as used in this study) would result in lower performance for the SLM. Our results also support the use of visual simulators in the clinic.
TF performance with the same IOL largely varies across individuals, indicating that the visual experience of a multifocal correction is rather unique to the patient and therefore valuable
to be demonstrated to a patient prior to implantation. We found lower differences in TF performance across patients with the same IOL (0.10 ± 0.02 RMS TF difference) than in different IOLs
on the same patient (0.13 ± 0.02 RMS TF difference). Visual simulators can help identifying those patients whose visual quality will be largely affected by a multifocal correction. For
example, patient S#6 experiences a large drop in VA with both multifocal corrections (44.6% for the Bi-R and 48.5% for the Tri-F compared to the monofocal performance at far), and while
depth-of-focus is enlarged, VA remains low for a large range. On the other hand, most patients experience minimal changes in VA for far (average multifocal VA/monofocal VA at far, 1.05 for
the Bi-R and 0.95 for the Tri-F) and exhibit functional VA at a near (average VA for near, 0.60 for the Bi-R and 0.53 for the Tri-F), and even an intermediate peak/range for the Tri-F. The
significant differences in TF performance of the same IOL across subjects are likely associated to the different interactions between the subjects native aberrations and the IOL optics5,6,
and to a lesser extent, to neural factors and adaptation of the subject to native aberrations. While in the current study, measurements were done under natural aberrations (and these were
not included as a variable in the study) it is interesting to note that the AO instrument in this study allows measurement and correction of these aberrations. An interesting open question
is whether the TF performance would have been more similar across subjects had the native aberrations of the eye been corrected. On the other hand, despite the contribution of the subject’s
aberrations to the effective TF, there are clear observable features in the TF curves attributable to the lens design. For example, TF VA with the trifocal IOL in patient S#7 reveals clearly
three best foci (both with the real and simulated IOL). The ability of visual simulators to capture the performance of the specific IOL designs supports their clinical utility not only to
demonstrate multifocality to a prospective patient, but also to demonstrate differences across different commercial lenses. The ultimate utility of the visual simulators relies on their
application on patients prior to intraocular lens implantation. The tested intraocular lenses are designed to replace the natural crystalline lens. Visual simulators are designed generally
to be used on phakic eyes, while a post-operative validation of the real IOL will not include the contribution of the crystalline lens (except for phakic IOLs). As the cornea is the major
contributor to the ocular aberrations we expect the crystalline lens contribution to pre-operative measurements to be secondary, particularly in the presence of a multifocal correction.
Furthermore, a cataractous crystalline lens will produce an overall decrease of visual performance. While a direct pre- and post-operative comparison of TF visual quality with simulators and
real IOL is only possible for clear crystalline lens, we expect (particularly with zonal segmented corrections) SimVis technology to be generally less affected by opacities, as due to the
temporal multiplexing the simultaneous image will be projected on the retina bypassing opacities31. The current study demonstrates that visual simulations in an AO system capture to a large
extent the optical and visual performance obtained with real IOLs, both in absolute values and the shape of TF curves when compared, for the first time, on the same individual patients.
Visual simulators based on different technologies (real IOLs, SLMs, SimVis technology) are useful programmable tools to predict visual performance with M-IOLs. METHODS TF optical and visual
quality, produced by real M-IOLs, was compared with visual simulations using two different active optical elements, a phase-only reflective LCoS-SLM and SimVis technology (temporal
multiplexing of an optotunable lens), in a custom-made polychromatic Adaptive Optics (AO) Visual Simulator. Vision was tested on seven cyclopleged subjects, through two real multifocal IOLs
(bifocal refractive and trifocal diffractive) projected on the subject’s pupil plane and their corresponding simulations with SLM and SimVis technology. The experiments were performed in a
multi-channel polychromatic AO visual simulator, with the DM correcting the optical aberrations of the system. All channels shared a similar display where the visual stimuli were shown. The
same system was used to demonstrate performance of the real IOLs, SLM and SimVis technology simulations on bench, using double-pass retinal imaging and an artificial eye. AO-BASED VISUAL
SIMULATOR On-bench measurements and visual tests were performed in a custom-developed polychromatic AO system at the Visual Optics and Biophotonics Lab (Institute of Optics, Spanish National
Research Council, IO-CSIC, Madrid, Spain), described partially in previous publications5,8,12. In this AO system, the visual stimulus is seen through 3 different active optical elements:
(1) a reflective deformable mirror (DM), used in this study to correct the subject and the system aberrations; (2) a reflective phase-only spatial light modulator (LCoS-SLM), and (3) a
simultaneous vision simulator (SimVis technology) based on temporal multiplexing of a opto-tunable lens, both used to simulate the multifocal designs; and for the purposes of the current
study, real multifocal IOLs placed in a cuvette. The DM, SLM, SimVis technology and real IOLs were placed in conjugate pupil planes of the system. The current configuration of the system,
shown in a schematic diagram in Fig. 6, is formed by 8 different channels: * (1) The _Illumination-Channel_, contains a supercontinuum laser source (SCLS, SC400 femtopower 1060
supercontinuum laser, Fianium Ltd, United Kingdom), in combination with a dual acousto‐optic tunable filter (AOTF) module (Gooch & Housego, United Kingdom), operated by RF drivers, to
automatically select the wavelengths in the different channels (visible 450–700 nm or near infrared light 700–1100 nm, in our system configuration). The output is a collimated beam coupled
to two independent multimode fibers. Illumination coming from the two independent fiber-channels of the SCLS enters the system collinearly by means of a hot mirror (HM), allowing wavefront
sensing and retinal aerial imaging with visible (VIS) and near infrared (NIR) light. The 2-mm diameter beam entering the eye is slightly (1 mm) decentered with respect to the pupil center to
avoid corneal reflections in the Hartmann-Shack images. Illumination coming from the VIS multimode fiber (BS5) is also used to monochromatically illuminate the visual stimuli. In this
study, a visible wavelength (555 nm) was used to illuminate the visual display. Aberration and double-pass retinal images were collected in NIR (827 nm). The laser power measured at the
corneal plane ranged between 0.5 and 50 μW, which was one order of magnitude below the ANSI standards safety limits at all tested wavelengths36. * (2) The _AO-Channel_ consists of a
Hartmann-Shack wavefront sensor (microlens array 40 × 32, 3.6 mm effective diameter, centered at 1062 nm; HASO 32 OEM, Imagine Eyes, France) and an electromagnetic deformable mirror (DM) (52
actuators, 15-mm effective diameter, 50-µm stroke; MIRAO, Imagine Eyes, France), to measure and correct subjects and system aberrations, respectively. * (3) The _SLM-Channel_ that consists
of a reflective phase-only LCoS-SLM (SLM; VIS; Resolution: 1920 × 1080; Pixel pitch: 8.0 µm; Holoeye Photonics AG, Germany) is used to generate the multifocal designs. * (4) The
_Testing-Channel_, placed in a conjugate pupil plane of the system, allows evaluating the simultaneous vision simulator (SimVis technology), as well as, the real IOLs. A custom-developed
cuvette was used to place the real IOLs, which was composed by two assembled metal pieces with transparent windows and an internal support to set the real IOL in the proper plane and
orientation. Expansion joints provided watertight seal so that the cuvette can be filled with distilled water. The DM, the wavefront sensor, the SLM and the testing plane (real IOLs and
SimVis technology) are conjugate to the pupil by different relays of lenses. Magnification from the pupil is 2x to the DM, 1x to the SLM and the testing plane, and 0.5x to the wavefront
sensor. * (5) The _Retinal imaging-Channel_ allows capturing retinal images of a 250 µm point source, and consists of a CCD camera (Retiga 1300, CCD Digital Camera, 12-bit, Monochrome, 6.7 ×
6.7 µm pixel size, 1024 × 1280 pixels; QImaging, Canada), a collimating lens (L9, 50-mm focal length) and a camera lens (L16, 135-mm focal length) in the double-pass retinal imaging
channel. The laser beam is filtered before entering the eye by means of a spatial filter (Fig. 6) composed of a microscope objective (20x), a 25 μm-pinhole and a 50 mm lens. This channel
acts in fact as a “one-and-a half pass”, with the aerial image being the autocorrelation37 of the image of the laser spot with a 2-mm entry beam and that with a 1-mm exit beam. * (6) The
_Psychophysical-Channel_, placed in a conjugate retinal plane, consists of a Digital Micro-Mirror Device (DMD) (DLP® Discovery™ 4100 0.7 XGA, Texas Instruments, USA), and allows displaying
visual stimuli with a 1.62 deg angular subtend. The DMD is monochromatically illuminated with light coming from the SCLS, 555 nm in this experiment. A holographic diffuser (HD) placed in the
beam path breaks the coherence of the laser beam providing a uniform illumination of the stimulus. * (7) The _Pupil Monitoring-Channel_, which allows monitoring of pupil size and subject
position during measurements, consists of a camera (DCC1545M, High Resolution USB2.0 CMOS Camera, Thorlabs GmbH, Germany) conjugated to the eye’s pupil (by means of a 105-mm focal length
objective lens (L12)). * (8) The _Badal optometer-Channel_ corrects for defocus in AO-, SLM-, Testing- and Psychophysical-Channels and allows TF psychophysical testing. Two automatized
shutters allow simultaneous illumination of the eye (S1) and the stimulus (S2). All optoelectronic and mechanical elements of the AO set-up were automatically controlled and synchronized
using custom-built software (Visual C++ and C# (Microsoft). The custom-developed routines make use of the manufacturer’s Software Development Kit for Hartmann-Shack centroiding detection and
wave aberration polynomial fitting. MULTIFOCAL DESIGNS: BIFOCAL REFRACTIVE AND TRIFOCAL DIFFRACTIVE Two M-IOLs (bifocal non-rotationally symmetric refractive, Bi-R, and trifocal
diffractive, Tri-D) were projected on the eye’s pupil, and also mapped in the SLM (as a spatial phase map) and on SimVis technology (as a temporal profile), shown in Fig. 7. The bifocal
non-rotationally symmetric refractive (Bi-R) IOL design mimics the Lentis MPlus LS-313 MF30 (Oculentis, Berlin, Germany), a multifocal acrylic refractive IOL, made out of hydrosmart, a
copolymer consisting of acrylates with hydrophobic surface, UV absorbing (n = 1.46). The optical design consists of an aspherical surface with a posterior sector shaped near vision segment,
which provides 2 useful focal distances: 0.0 D for far-vision, and +3.00 D addition for near-vision. The trifocal diffractive (Tri-D) design corresponds to the POD F (FINeVision, PhysIOL,
Liege, Belgium), a hydrophilic (26% hydrophilic acrylic) aspheric multifocal diffractive IOL built with a combination of two bifocal diffractive patterns, of which one is for far and
near-vision and the other for far and intermediate-vision38,39. The combination of the two diffractive structures provides 3 useful focal distances: 0.0 D for far-vision, +1.75 D addition
for intermediate-vision and +3.50 D addition for near-vision38. REAL IOLS Two 0-D M-IOLs with the Bi-R and Tri-D designs (provided by the manufacturers) were inserted in a cuvette filled
with distilled water, placed in a conjugate pupil plane, and projected on the eye’s pupil of the subjects. Calculated TF curves (Fig. 7, right plots) show distinct bifocal and trifocal
performance. SPATIAL LIGHT MODULATOR (SLM) The multifocal phase maps (Bi-R and Tri-D) were extracted in pseudophakic computer eye models from the knowledge of the surface height profiles of
the lenses, provided by the respective manufacturers, as described in a previous publication33. Matlab routines were used to numerically simulate the multifocal phase designs, the Bi-R and
Tri-D, which were later programmed in a reflective phase-only LCoS-SLM. The SLM addressable phase maps (Φ) were evaluated from the multifocal phase maps by performing 2π-wrapping such that,
Φ = X [mod 2π], where X represents the unwrapped phase map. and Φ is the wrapped phase map. The generated phase pattern is a grey-scale image, where each level of grey corresponds to a
certain phase difference in the interval [0 2π] (Fig. 7, central plots). The images were generated for a 5-mm pupil. SIMVIS TECHNOLOGY & TEMPORAL MULTIPLEXING Both multifocal designs
were mapped using SimVis technology with a temporal profile, as shown in Fig. 7. The TF optical quality of the two multifocal designs in terms of Visual Strehl (VS)32 was estimated for a 5
mm pupil diameter at 555 nm. The corresponding SimVis temporal profile that provides an equivalent TF VS was determined31. The temporal profiles were addressed with SimVis technology as
shown in Fig. 7, right plots. ON-BENCH TESTING TF optical quality for the three conditions, real IOLs, SLM and SimVis technology, was evaluated on bench in the same AO system using TF
double-pass retinal images and TF retinal images of an E-optotype from an artificial eye. Focus shifts were achieved by moving a Badal optometer from +1.00 D to −4.50 D in 0.25 D-steps,
around the best foci for far. _TF DP aerial retinal_ images (DP) were obtained for an artificial eye in place of the human eye (consisting of a 50.8-mm focal length achromatic doublet lens
and a rotating diffuser as an artificial retina) for the real IOL and the two simulations with the SLM and SimVis technology. Images of a “point-source” were obtained at 555 nm for a 5-mm
pupil exit pupil diameter. _TF retinal images of an E-optotype_ (1.62-deg subtend) (1P) were collected on an artificial eye provided with an objective lens (50.8 mm) and a CCD camera
(DCC1545M, High Resolution USB2.0 CMOS Camera, Thorlabs GmbH, Germany) acting as a “retina”, in place of the subject’s eye. The stimuli were displayed in the Digital Micro-Mirror Device
(DMD), illuminated with 555 nm light from the SCLS, for 5-mm pupil diameter. PATIENTS Seven subjects were monocularly tested in the system under cycloplegia. Subjects were non-presbyopic (35
± 3 years old) and nearly emmetropic (spherical error: −0.85 ± 0.90 D, astigmatism <0.50 D in all cases). The RMS for 3rd and higher order aberrations (5-mm pupil diameter) in the
subjects ranged from 0.19 to 0.59 um. All protocols met the tenets of the Declaration of Helsinki and had been previously approved by the Spanish National Research Council (CSIC) Bioethical
Committee. All participants were acquainted with the nature and possible consequences of the study and provided written informed consent. THROUGH-FOCUS VISUAL ACUITY VA was measured using an
8-Alternative Forced Choice (8AFC)40 procedure with Tumbling E letters and a QUEST (Quick Estimation by Sequential Testing) algorithm programmed with the Psychtoolbox package41 to calculate
the sequence of the presented stimulus (letter size and orientation) in the test following the subject’s response. Measurements were performed at different positions of the Badal Optometer
ranging from −1.00 to +4.00 D, for the two lenses and the SLM and SimVis technology simulations. After looking for their best subjective focus without a multifocal correction and prior to
measurements, subjects were shown the whole TF range with the corresponding design, so that they could identify the approximate position of their best focus for the different visual
distances (far, intermediate and near). After that, measurements were performed at different positions of the TF range with higher sampling around the identified foci, which varied for each
subject. The QUEST routine for each VA measurement consisted of 40 trials, each one presented for 0.5 seconds, where the threshold criterion was set to 75%. The threshold, VA measurement,
was estimated as the average of the 10 last stimulus values. Visual acuity was expressed in terms of decimal acuity (logMAR = −log10[decimal acuity])42. Variability of each VA measurement
was obtained from the standard deviation of the 10 last stimulus values used to estimate the threshold in each measurement. EXPERIMENTAL PROTOCOL ON PATIENTS Subjects were stabilized using a
dental impression and the eye’s pupil was aligned to the optical axis of the instrument (using an x-y-z stage moving a bite bar) using the line of sight as a reference, while the natural
pupil is viewed on the monitor using a pupil camera. To ensure constant pupil diameter during the measurements, a 5-mm artificial pupil was placed in a conjugate pupil plane. Measurements
were performed monocularly, in a darkened room, under cycloplegia (by instillation of Tropicamide 1%, 2 drops 30 minutes prior to the beginning of the study, and 1 drop every 1 hour). The
subject was asked to adjust the Badal system position to achieve best subjective focus. Subjects viewed the psychophysical stimulus generated by the Digital Micro-Mirror Device (DMD),
illuminated monochromatically at 555 nm, through the real IOL, the SLM- or SimVis technology- simulated M-IOLs or the real IOLs and performed the corresponding psychophysical test (TF VA).
The order of the simulation conditions was randomized. Subjects were instructed on the nature of the experiment and performed some trial runs prior to the test. DATA ANALYSIS TF optical
quality was obtained from DP retinal images and images of the E-stimulus on bench. The double-pass image quality metric as defined as the full width at half maximum (FWHM) of the images43,
so the width will be smaller for more focused images. Image series were obtained for each simulator under the same experimental conditions: laser power, pupil diameter, exposure time.
However, due to the different baseline of the different technologies, exposure times were different across simulators and subsequently images were normalized to calculate the image quality
metric, which was normalized to the 0 D image series within each TF image series. The image quality metric for the E-stimulus was obtained from the correlation coefficient (correlation of
the E-letter with a monofocal correction and each collected image in the same conditions: laser power, pupil diameter, exposure time) of the image series, after each image was centered. A
sub-image of the best focused image from the monofocal image series was used in the correlation calculations TF optical quality (on bench) and TF visual quality (in patients) curves were
obtained for the real IOL and SLM and SimVis technology simulations for both the bifocal and trifocal lens designs. The comparison between the real and simulated performances were expressed
in terms of Root-Mean-Square (RMS) difference of the linearly interpolated TF curves (in a 5.00 D range), taking the real IOL as the reference, as metric for the quality of the replication
of the lens design by the simulators. Statistical analysis was performed with SPSS software (IBM) to test differences across results with the different simulators, and optical designs
(paired-samples t-test) in both cases: on-bench and on patients’ results (n = 7). A mixed model analysis for repeated measurements was performed to investigate differences in outcomes for
the two simulation techniques, as a function of the two multifocal designs and the interaction with through focus level. In the model, fixed-effect factors were the TF steps of the TF VA
curve, and the type of simulator, whereas the repeated effect was the combination of both. TF VA curve was the random effect factor in the model in all cases. DATA AVAILABILITY All data
generated or analyzed during this study are included in this published article. The datasets generated during and/or analyzed during the current study are available from the corresponding
author on reasonable request. REFERENCES * Davies, R. & Kasper, M. Adaptive Optics for Astronomy. _Annual Review of Astronomy and Astrophysics_ 50, 305–351,
https://doi.org/10.1146/annurev-astro-081811-125447 (2012). Article ADS CAS Google Scholar * Booth, M. J. Adaptive optical microscopy: the ongoing quest for a perfect image. _Light:
Science & Applications_ 3, https://doi.org/10.1038/lsa.2014.46 (2014). * Marcos, S. _et al_. Vision science and adaptive optics, the state of the field. _Vision Res_ 132, 3–33,
https://doi.org/10.1016/j.visres.2017.01.006 (2017). Article PubMed PubMed Central Google Scholar * Liang, J. & Williams, D. R. Aberrations and retinal image quality of the normal
human eye. _J Opt Soc Am A Opt Image Sci Vis_ 14, 2873–2883 (1997). Article ADS CAS Google Scholar * Vinas, M. _et al_. Testing vision with angular and radial multifocal designs using
Adaptive Optics. _Vision Res_. https://doi.org/10.1016/j.visres.2016.04.011 (2016). Article PubMed Google Scholar * Radhakrishnan, A., Dorronsoro, C. & Marcos, S. Differences in
visual quality with orientation of a rotationally asymmetric bifocal intraocular lens design. _J Cataract Refract Surg_ 42, 1276–1287, https://doi.org/10.1016/j.jcrs.2016.06.034 (2016).
Article PubMed Google Scholar * Vinas, M., Sawides, L., de Gracia, P. & Marcos, S. Perceptual adaptation to the correction of natural astigmatism. _PLoS One_ 7, e46361,
https://doi.org/10.1371/journal.pone.0046361 PONE-D-12-08338 (2012). * Vinas, M., Dorronsoro, C., Cortes, D., Pascual, D. & Marcos, S. Longitudinal chromatic aberration of the human eye
in the visible and near infrared from wavefront sensing, double-pass and psychophysics. _Biomed Opt Express_ 6, 948–962, https://doi.org/10.1364/BOE.6.000948 (2015). Article PubMed PubMed
Central Google Scholar * Marcos, S., Sawides, L., Gambra, E. & Dorronsoro, C. Influence of adaptive-optics ocular aberration correction on visual acuity at different luminances and
contrast polarities. _J Vis_ 8(1), 1–12, https://doi.org/10.1167/8.13.1 (2008). Article PubMed Google Scholar * Artal, P. C. L., Fernandez, E. J., Singer B., Manzanera, S. & Williams,
D. R. Neural compensation for the eye’s optical aberrations. _J Vis_ 4(4), 281–287, https://doi.org/10:1167/4.4.4/4/4/4/ (2004). * Sawides, L., de Gracia, P., Dorronsoro, C., Webster, M. A.
& Marcos, S. Vision is adapted to the natural level of blur present in the retinal image. _PLoS One_ 6, e27031, https://doi.org/10.1371/journal.pone.0027031, PONE-D-11-12870 (2011). *
Vinas, M. _et al_. Comparison of vision through surface modulated and spatial light modulated multifocal optics. _Biomed. Opt. Express_ 8, 2055–2068 (2017). Article Google Scholar *
Dorronsoro, C., Radhakrishnan, A., de Gracia, P., Sawides, L. & Marcos, S. Perceived image quality with different experimentally simulated segmented bifocal corrections. _Biomed. Opt.
Express_ 7, 4388–4399 (2016). Article Google Scholar * Dorronsoro, C. _et al_. Portable simultaneous vision device to simulate multifocal corrections. _Optica_ 3, 918–924,
https://doi.org/10.1364/OPTICA.3.000918 (2016). Article Google Scholar * Glasser, A. & Campbell, M. C. Presbyopia and the optical changes in the human crystalline lens with age.
_Vision Res_ 38, 209–229 (1998). Article CAS Google Scholar * Charman, W. N. Developments in the correction of presbyopia II: surgical approaches. _Ophthalmic Physiol Opt_ 34, 397–426,
https://doi.org/10.1111/opo.12129 (2014). Article PubMed Google Scholar * Schwarz, C. _et al_. Binocular visual acuity for the correction of spherical aberration in polychromatic and
monochromatic light. _J Vis_ 14, https://doi.org/10.1167/14.2.8 (2014). * Manzanera, S. & Artal, P. Minimum change in spherical aberration that can be perceived. _Biomed Opt Express_ 7,
3471–3477, https://doi.org/10.1364/BOE.7.003471 (2016). Article PubMed PubMed Central Google Scholar * de Gracia, P. _et al_. Combining coma with astigmatism can improve retinal image
over astigmatism alone. _Vision Res_ 50, 2008–2014, https://doi.org/10.1016/j.visres.2010.07.014 (2010). Article PubMed Google Scholar * Dou, R. & Giles, M. K. Closed-loop
adaptive-optics system with a liquid-crystal television as a phase retarder. _Opt Lett_ 20, 1583–1585 (1995). Article ADS CAS Google Scholar * Love, G. D. Wave-front correction and
production of Zernike modes with a liquid-crystal spatial light modulator. _Appl Opt_ 36, 1517–1520 (1997). Article ADS CAS Google Scholar * Schwarz, C., Prieto, P. M., Fernandez, E. J.
& Artal, P. Binocular adaptive optics vision analyzer with full control over the complex pupil functions. _Opt Lett_ 36, 4779–4781, https://doi.org/10.1364/OL.36.004779 (2011). Article
ADS PubMed Google Scholar * Martinez-Cuenca, R. _et al_. Closed-loop adaptive optics with a single element for wavefront sensing and correction. _Opt Lett_ 36, 3702–3704,
https://doi.org/10.1364/OL.36.003702 (2011). Article ADS PubMed Google Scholar * Zhang, Z., You, Z. & Chu, Z. Fundamentals of phase-only liquid crystal on silicon (LCOS) devices.
_Light: Science & Applications_, https://doi.org/10.1038/lsa.2014.94 (2014). * Manzanera, S., Prieto, P. M., Ayala, D. B., Lindacher, J. M. & Artal, P. Liquid crystal Adaptive Optics
Visual Simulator: Application to testing and design of ophthalmic optical elements. _Opt Express_ 15, 16177–16188, 146452 (2007). * Tabernero, J., Schwarz, C., Fernandez, E. J. & Artal,
P. Binocular visual simulation of a corneal inlay to increase depth of focus. _Invest Ophthalmol Vis Sci_ 52, 5273–5277, https://doi.org/10.1167/iovs.10-6436 (2011). Article PubMed Google
Scholar * Zhao, L. _et al_. Efficient implementation of a spatial light modulator as a diffractive optical microlens array in a digital Shack-Hartmann wavefront sensor. _Appl Opt_ 45,
90–94 (2006). Article ADS Google Scholar * Lombardo, M., Serrao, S., Devaney, N., Parravano, M. & Lombardo, G. Adaptive optics technology for high-resolution retinal imaging.
_Sensors_ (Basel) 13, 334–366, https://doi.org/10.3390/s130100334 (2012) * Hervella, L., Villegas, E. A., Prieto, P. M. & Artal, P. Assessment of subjective refraction with a clinical
adaptive optics visual simulator. _J Cataract Refract Surg_ 45, 87–93, https://doi.org/10.1016/j.jcrs.2018.08.022 (2019). * Stefano, B. _et al_. Multi-actuator adaptive lens for wavefront
correction in optical coherence tomography and twophoton excitation fluorescence microscopy (Conference Presentation). SPIE BiOS.2016. * Akondi, V., Dorronsoro, C., Gambra, E. & Marcos,
S. Temporal multiplexing to simulate multifocal intraocular lenses: theoretical considerations. _Biomed Opt Express_ 8, 3410–3425, https://doi.org/10.1364/BOE.8.003410 (2017). Article
PubMed PubMed Central Google Scholar * Marsack, J. D., Thibos, L. N. & Applegate, R. A. Metrics of optical quality derived from wave aberrations predict visual performance. _J Vi_s 4,
322–328, https://doi.org/ 10:1167/4.4.8/4/4/8/ (2004). * Akondi, V. _et al_. Evaluation of the True Wavefront Aberrations in Eyes Implanted With a Rotationally Asymmetric Multifocal
Intraocular Lens. _J Refract Surg_ 33, 257–265, https://doi.org/10.3928/1081597X-20161206-03 (2017). Article PubMed Google Scholar * Bouchal, Z., Chlup, V., Celechovsky, R., Bouchal, P.
& Nistor, I. C. Achromatic correction of diffractive dispersion in white light SLM imaging. _Opt Express_ 22, 12046–12059, https://doi.org/10.1364/OE.22.012046 (2014). Article ADS
PubMed Google Scholar * Vinas, M. _et al_. _In Vivo_ Measurement of Longitudinal Chromatic Aberration in Patients Implanted With Trifocal Diffractive Intraocular Lenses. _J Refract Surg_
33, 736–742, https://doi.org/10.3928/1081597X-20170814-01 (2017). Article PubMed Google Scholar * Delori, F. C., Webb, R. H. & Sliney, D. H. Maximum permissible exposures for ocular
safety (ANSI 2000), with emphasis on ophthalmic devices. _J Opt Soc Am A Opt Image Sci Vis_ 24, 1250–1265, 132117 (2007). * Artal, P., Marcos, S., Navarro, R. & Williams, D. R. Odd
aberrations and double-pass measurements of retinal image quality. _J Opt Soc Am A Opt Image Sci Vis_ 12, 195–201 (1995). Article ADS CAS Google Scholar * Gatinel, D., Pagnoulle, C.,
Houbrechts, Y. & Gobin, L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. _J Cataract Refract Surg_ 37, 2060–2067,
https://doi.org/10.1016/j.jcrs.2011.05.047 (2011). Article PubMed Google Scholar * Gatinel, D. & Houbrechts, Y. Comparison of bifocal and trifocal diffractive and refractive
intraocular lenses using an optical bench. _J Cataract Refract Surg_ 39, 1093–1099, https://doi.org/10.1016/j.jcrs.2013.01.048 (2013). Article PubMed Google Scholar * Ehrenstein, W. H.
& Ehrenstein, A. In _Modern techniques in neuroscience research_ (eds Windhorst, U. & Johansson, H.) Ch. 43, 1211–1240 (Springer, 1999). * Brainard, D. H. The Psychophysics Toolbox.
_Spat Vis_ 10, 433–436 (1997). Article CAS Google Scholar * Holladay, J. T. Proper method for calculating average visual acuity. _J Refract Surg_ 13, 388–391 (1997). CAS PubMed Google
Scholar * Marcos, S., Moreno, E. & Navarro, R. The depth-of-field of the human eye from objective and subjective measurements. _Vision Res_ 39, 2039–2049 (1999). Article CAS Google
Scholar Download references ACKNOWLEDGEMENTS This research has received funding from the European Research Council under the European Union’s Seventh Framework Program (FP/2007–2013)/ERC
Grant Agreement. [ERC-2011-AdC 294099]; the H2020 COFUND Marie Curie 291820 program; ERCPoC SimVis project. This study was also supported by Spanish Government grant FIS2014-56643-R to S.M.,
FIS2017-84753-R to S.M. and C.D., and DTS16-00127 to C.D., and Spanish Government FPU Predoctoral Fellowship (FPU16/01944) to S.A. Authors thank Laura Barrios from the Scientific Calculus
Center of the Spanish National Research Council (CSIC) for help with the statistical analysis. AUTHOR INFORMATION Author notes * Vyas Akondi Present address: Department of Ophthalmology,
Stanford University, Palo Alto, California, USA AUTHORS AND AFFILIATIONS * Institute of Optics, Spanish National Research Council, IO-CSIC, Serrano, 121, Madrid, 28006, Spain Maria Vinas,
Clara Benedi-Garcia, Sara Aissati, Daniel Pascual, Vyas Akondi, Carlos Dorronsoro & Susana Marcos Authors * Maria Vinas View author publications You can also search for this author
inPubMed Google Scholar * Clara Benedi-Garcia View author publications You can also search for this author inPubMed Google Scholar * Sara Aissati View author publications You can also search
for this author inPubMed Google Scholar * Daniel Pascual View author publications You can also search for this author inPubMed Google Scholar * Vyas Akondi View author publications You can
also search for this author inPubMed Google Scholar * Carlos Dorronsoro View author publications You can also search for this author inPubMed Google Scholar * Susana Marcos View author
publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS M.V., C.D. and S.M. conceived the experiment(s); M.V., C.B. and S.A. conducted the experiment(s); M.V.
and D.P. developed specific experimental routines; V.A. provided the SLM phase maps and SimVis technology input signal; M.V. performed the statistical analysis; M.V. and S.M. analyzed the
results and wrote the manuscript. All authors reviewed the manuscript. CORRESPONDING AUTHOR Correspondence to Maria Vinas. ETHICS DECLARATIONS COMPETING INTERESTS M.V., D.P., V.A., C.D.,
S.M. Personal Financial Interest (2EyesVision); C.D. and S.M. patents (PCT/ES2010/070218; PCT/ES2014/070725; PCT/ES2016/070673). ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature
remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the
article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use
is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Vinas, M., Benedi-Garcia, C., Aissati, S. _et al._ Visual simulators replicate
vision with multifocal lenses. _Sci Rep_ 9, 1539 (2019). https://doi.org/10.1038/s41598-019-38673-w Download citation * Received: 15 June 2018 * Accepted: 04 January 2019 * Published: 07
February 2019 * DOI: https://doi.org/10.1038/s41598-019-38673-w SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Climate change can drive social tipping points – for better or for worseIt’s impossible to turn on the TV, listen to the radio or scroll social media without hearing about real-world climate i...
Strain sensor on a chip for quantifying the magnitudes of tensile stress on cellsABSTRACT During cardiac development, mechanotransduction from the in vivo microenvironment modulates cardiomyocyte growt...
rinkya | TechCrunchSAVE $200+ ON YOUR TECHCRUNCH ALL STAGE PASS BUILD SMARTER. SCALE FASTER. CONNECT DEEPER. JOIN VISIONARIES FROM PRECURSO...
Form a64a: application to receive information from court records about a parental orderForm FORM A64A: APPLICATION TO RECEIVE INFORMATION FROM COURT RECORDS ABOUT A PARENTAL ORDER Form A64A: Application to r...
Clean up or we’ll close down bangalore: congressThe Congress has warned the state government that it will call for Bangalore bandh if the garbage problem is not solved ...
Latests News
Visual simulators replicate vision with multifocal lensesABSTRACT Adaptive optics (AO) visual simulators based on deformable mirrors, spatial light modulators or optotunable len...
Hyme energy signs global deal with arla to scale thermal storage tech | techcrunchFor many industries, lithium batteries just don’t cut it — they’re getting increasingly expensive, require too much spac...
Find all the latest news about malta | euronewsWater Matters Europe's water is under increasing pressure. Pollution, droughts, floods are taking their toll on our...
Neuroscience Center | NatureAccess through your institution Buy or subscribe This is a preview of subscription content, access via your institution ...
Brexit news: eight 'hardball' cards may can use to get the best dealBrexit news: Economist suggests eight ways Theresa May can pressure deal from EU counterparts (Image: GETTY) The Prime M...