The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritis
The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritis"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Knee osteoarthritis (OA) is an established risk factor for falls and balance impairment. This study investigated the incidence of falls, balance-related outcomes and risk factors
for falls before and after primary total knee arthroplasty (TKA). Three hundred seventy-six OA patients scheduled to undergo TKA were included. Falls data within the preoperative, first
postoperative and second postoperative years were collected, balance-related functions were assessed using the Assessment of Quality of Life (AQoL), WOMAC, Falls Efficacy Scale International
(FES-I), Activities-specific Balance Confidence (ABC), knee extension strength, Berg Balance Scale (BBS) and Timed Up and Go (TUG) before surgery and 1 and 2 years after surgery. Compared
with preoperative values, the incidence of falls significantly decreased (14.89%, 6.23% and 3.14% within the preoperative, first postoperative and second postoperative years, respectively)
and the AQoL, WOMAC, FES-I, ABC, knee extension strength, BBS and TUG significantly improved after TKA. Logistic regression analysis revealed that Kellgren-Lawrence grade ≥ 3 of the
contralateral knee was an independent risk factor for falls before and after TKA. Conclusively, primary TKA is associated with a reduced incidence of falls and improved balance-related
functions, and the contralateral knee should be considered in the design of fall-prevention strategies in patients with OA. SIMILAR CONTENT BEING VIEWED BY OTHERS FALL CLASSIFICATION,
INCIDENCE AND CIRCUMSTANCES IN PATIENTS UNDERGOING TOTAL KNEE REPLACEMENT Article Open access 18 November 2022 MEDIAL OPEN-WEDGE HIGH TIBIAL OSTEOTOMY FOR THE TREATMENT OF DEGENERATIVE VARUS
KNEE OSTEOARTHRITIS IN GERIATRIC PATIENTS: A RETROSPECTIVE STUDY Article Open access 06 October 2023 HIP ABDUCTION ANGLE AFTER OPEN-WEDGE HIGH TIBIAL OSTEOTOMY IS ASSOCIATED WITH THE TIMED
UP & GO TEST AND RECURRENCE OF VARUS ALIGNMENT Article Open access 29 April 2023 INTRODUCTION Falls are among the most common causes of injury and hospitalization in the elderly, and an
estimated 1/3 of people over the age of 65 fall each year1. The reported annual incidence of falls among older Chinese community-dwelling people ranges from 11% to 34%, and the annual
incidence of more than one fall is 4% to 5%2. Balance is a complex function that requires the integration of sensory information of the position of the body and the ability to make proper
motor responses to body movement3. Balance is essential for maintaining postural stability while performing daily activities4, and loss of balance is a common cause of falls in older
people5,6. Osteoarthritis (OA) is a widely prevalent and age-associated joint disorder, and it is an important risk factor for falls. More than 50% of all OA patients and 64% of female OA
patients report falling within one year5,7,8,9. Approximately 60% to 80% of patients with knee OA report joint instability10,11. No effective treatments are currently available to prevent or
reverse OA progression12, but total knee arthroplasty (TKA) is a common surgical intervention for treating end-stage knee OA. TKA aims to relieve pain, restore loco-motor functions, correct
deformities and improve quality of life13. Patients with knee OA undergoing TKA often present with residual functional deficits, and one important area of concern is balance impairments,
which increase the risk of falls in these patients14,15,16,17. The incidence of falls is as high as 7% to 40% after TKA18,19,20. An understanding of the issues associated with the recovery
of balance-related functions following TKA may ultimately enhance the design of fall-prevention programmes supported by scientific evidence3. Previous studies assessed balance-related
functions in OA patients only during early stages after TKA at 1 year or less in small samples, and the results were inconsistent and controversial3,5,21. OA often involves bilateral
knees22, and previous studies demonstrated that the pain and knee extension strength of the contralateral knee were associated with knee functions after TKA22,23. However, few studies
investigated the impact of the OA status of the contralateral knee on the incidence of falls after primary TKA. We hypothesize that the annual incidence of falls and balance-related
functions will improve after primary TKA, and the OA status of the contralateral knee, age and sex are risk factors for falls before and after TKA in OA patients. This study investigated the
following specific issues: (1) the annual incidence of falls before and after primary TKA; (2) the effect of primary TKA on balance-related outcomes, such as fear of falling, balance
confidence and physical functions; and (3) the possible risk factors for falls before and after primary TKA in patients with knee OA. METHODS PATIENTS Consecutive patients who were scheduled
for primary unilateral TKA at the Department of Orthopaedics, West China Hospital, Sichuan University were assessed from August 2013 to December 2014 and invited to participate if they met
the following eligibility criteria: (1) diagnosis of end-stage primary knee OA with no previous surgery on either knee; (2) absence of uncontrolled systemic diseases, neurological, cardiac,
psychiatric disorders, or other medical conditions that would significantly compromise physical functions (e.g., stroke); and (3) sufficient language skills to communicate, the ability to
follow verbal instructions, and no memory problems. Patients were excluded for any of the following reasons: (1) if they did not understand the nature of the study; (2) if they underwent TKA
due to non-OA diseases, such as rheumatoid arthritis (RA) and traumatic injury; or (3) if they underwent reoperation of the replaced knee or received contralateral knee arthroplasty during
the follow-up period. Ethics approval was obtained from the Ethics Committee of West China Hospital, Sichuan University, and all procedures were performed according to the Declaration of
Helsinki. All participants were informed of the nature of the study and signed a written informed consent before participation. TOTAL KNEE ARTHROPLASTY The same surgical team performed all
surgeries using a standard medial parapatellar approach in the same laminar air flow operating room, and a posterior stabilized knee prosthesis system (DePuy, New Jersey, USA) with a mobile
or fixed bearing was used in all patients. A pneumatic tourniquet was used in all patients, which was inflated before skin incision and released after prosthesis placement, and a suction
drainage was indwelled before suturing and removed the first morning after surgery. All patients received similar perioperative physiotherapy, such as enhanced perioperative education,
muscle strengthening and gait re-education before surgery, flexion-extension of the ankle joints and straight leg raising immediately after anaesthesia awakening, and flexion-extension of
the operated knee, muscle strengthening and gait re-education beginning on the first postoperative day (POD). Fall-prevention strategies, including an enhanced explanation of the hazards and
risk factors of falls to enhance patient consciousness of fall-prevention, correcting high-risk activities, introducing methods to avoid falling during daily activities, and guided
preoperative and postoperative functional exercises were performed during hospitalization (face to face) and after discharge (quarterly by telephone and at each follow-up visit). The
surgical characteristics, including incision length, operative time (from the skin incision to the end of skin suture) and prosthesis type (mobile or fixed) were recorded. SELF-REPORTED
MEASURES After being recruited to the study, participants completed a series of self-reported questionnaires and physical performance tests for falls, quality of life, fear of falling,
balance confidence and physical functions one day before surgery (T0), and 1 year (T1) and 2 years (T2) after surgery. A fall was defined as unintentionally coming to rest on the ground or
at some other lower level, not as a result of a major intrinsic event, such as faint or stroke3. Preoperative fall data within the previous 1 year were collected at T0, and postoperative
fall data were collected quarterly by telephone and confirmed at the yearly follow-up visit. Quality of life was measured using the self-reported Assessment of Quality of Life (AQoL), which
is composed of five domains, including illness, independent living, social relationships, physical senses and psychological well-being, with three items per domain24. The utility scores for
each dimension and an overall utility score from 0 to 1 (0 representing the worst health and 1 representing perfect health) were collected. The Short Falls Efficacy Scale International
(FES-I) questionnaire was used to evaluate the fear of falling25. The FES-I consists of seven items (score 1–4 for each) that evaluate the participant’s level of concern of the possibility
of falling when performing certain daily activities, and the total score ranges from 7 (not concerned) to 28 (severely concerned). The self-reported Activities-specific Balance Confidence
(ABC) Scale was used to quantify how confident a person feels that he or she will not lose balance while performing 16 certain daily activities on a scale from 0% (absolutely not confident)
to 100% (completely confident)18. The total score was averaged across the 16 items, and higher scores indicate greater balance confidence. Pain, stiffness and physical functions of the knee
were also assessed using the Western Ontario and McMaster University Osteoarthritis Index (WOMAC)26, which assesses over three domains, including the severity of knee pain during 5 daily
activities (range 0–500), stiffness (range 0–200), and physical functions of the lower extremities during 17 daily activities (range 0–1,700). The items were scored using a 100-mm visual
analogue scale, where 0 represents no pain, stiffness or difficulty with physical functions, and higher scores represent worse functional health. All three subscales are summed to provide a
total WOMAC score (range 0–2,400). PHYSICAL PERFORMANCE TESTS The knee extension strength, Berg Balance Scale (BBS), and Timed Up and Go (TUG) were used to further assess balance-related
functions. The knee extension strength was measured via isometric pulling at 90° against padded straps attached to an electronic dynamometer (HANDPITM, Zhejiang, China). The highest value
(kg) of the three trials was recorded and normalized to the patient’s body height and body mass using the following formula5: normalized knee extension strength = measured strength
(kg)/[body height (m) × body mass (kg)] × 100. The BBS is a physical assessment of balance comprising a set of 14 balance tasks27. Each subset was scored on a 5-level ordinal scale from 0 to
4, yielding a maximum total score of 56. Higher scores indicate better balance, and scores below 45 indicate an increased risk of falls. A change of 4–7 points in the elderly is the
estimated minimal detectable change at a 95% confidence level (MDC95) that may be objectively determined for a patient28. TUG is a test of functional mobility in older people29. The patient
is observed and timed while getting up from an armchair, walking 3 metres, and returning to their original seated position. Older adults who take longer than 14 sec to complete the TUG have
a high fall risk30, and the minimal level of detectable change at the 90% confidence level (MDC90) is 2.49 sec.31. Researchers with rich clinical experience in assessing elderly performed
the physical assessments, and the researchers were blinded to the preoperative results upon performing the postoperative assessments. STATISTICAL ANALYSIS All statistical analyses were
performed using SPSS software (version 22.0, IBM, USA). All continuous variables were assessed for normality of distribution using the Kolmogorov-Smirnov and Shapiro-Wilk tests prior to data
analysis. Comparisons of continuous variables between two groups were made using the _t_-test for normally distributed data or the Wilcoxon signed rank sum test for non-normally distributed
data. Comparisons of continuous variables between three or more groups were performed using one-way analysis of variance (ANOVA) with Student-Newman-Keuls (SNK) _post hoc_ analysis for
normally distributed data or the Kruskal-Wallis _H_ and Mann-Whitney _U_ tests for non-normally distributed data. Comparisons of dichotomous variables were performed using the _Cochran Q_
test for repeated measures or the _Chi-square_ (_χ_ 2) test for non-repeated measures. Binary logistic regression was performed to identify independent risk factors for falls, and the
general and surgical factors, including age, sex, body mass index, KL grade of the contralateral knee, incision length, operative time and prosthesis type, were included in the model. A _P_
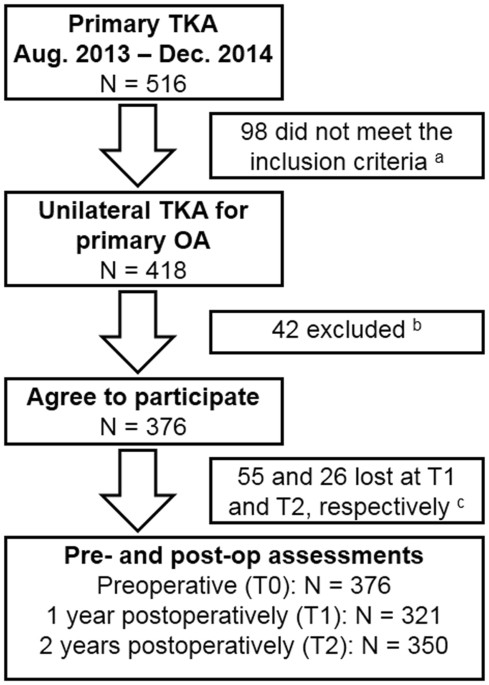
value less than 0.05 was considered statistically significant. RESULTS SUBJECTS Figure 1 provides the full details of the study flow. A total of 376 OA patients (117 males) undergoing
primary and unilateral TKA were included preoperatively, with a mean age of 68.88 (47–89) years. A total of 321 (85.37%) and 350 (93.09%) patients were followed-up at T1 and T2,
respectively. There were no significant differences in the general and surgical characteristics, including age, gender, body mass index (BMI), KL grade of the contralateral knee, incision
length, operative time and prosthesis type, between patients at T0 to T2 (all _Ps_ < 0.05). FALLERS AND FALLS BEFORE AND AFTER PRIMARY TKA Table 1 shows the details of the pre- and
postoperative fallers and falls. A total of 14.89% (56/376) of patients fell, encompassing a total of 101 falls in the last preoperative year. A total of 6.23% (20/321) of patients had a
total of 27 falls in the first postoperative year, and 3.14% (11/350) of patients had a total of 14 falls in the second postoperative year. A total of 58.93% (33/56) of the fallers
experienced more than one fall in the last preoperative year compared to 25.00% (5/20) and 18.18% (2/11) in the first and second postoperative years, respectively. There were significant
reductions in the postoperative number of total fallers (the incidence of falls) and fallers with more than one fall compared to the preoperative values (_Q_ = 50.98, _P_ < 0.01; _Q_ =
46.69, _P_ < 0.01, respectively). A total of 76.00% (38/50, n = 321) and 90.57% (48/53, n = 350) of preoperative fallers did not fall again in the first and second postoperative years,
respectively, and 2.95% (8/271, n = 321) and 2.02% (6/297, n = 350) of preoperative non-fallers fell in the first and second postoperative years, respectively. A significant shift in favour
of preoperative fallers becoming postoperative non-fallers was observed (_Q_ = 78.18, _P_ < 0.01). A total of 13.03% (49/376) of patients required an aid to walk independently outside at
T0, and this percentage was significantly reduced to 6.85% (22/321) and 3.71% (13/350) at T1 and T2, respectively (_Q_ = 58.50, _P_ < 0.01). BALANCE-RELATED OUTCOMES BEFORE AND AFTER
PRIMARY TKA Table 2 shows the serial changes in balance-related outcomes. The AQoL, WOMAC (total and subscales), FES-I, ABC, knee extension strength, BBS and TUG improved significantly after
primary TKA compared with preoperative values (all _Ps_ < 0.01). The AQoL was significantly higher at T2 than at T0 and T1, but no significant difference was found between the scores at
T0 and T1. The WOMAC (total and subscales) and FES-I were significantly lower at T1 and T2 than at T0, and the scores were also significantly lower at T2 than at T1. The ABC was
significantly higher at T1 and T2 than at T0, and the ABC was also significantly higher at T2 than at T1. Physical performance tests revealed that the knee extension strength and BBS were
significantly higher at T1 and T2 than at T0, and the knee extension strength was also significantly higher at T2 than at T1. No significant difference was observed between the BBS at T1 and
T2. A total of 61.68% (198/321) and 57.71% (202/350) of patients exhibited increased BBS scores at T1 and T2, respectively, and 45.48% (146/321) and 43.71% (153/350) exceeded the MDC95 (4
points) at T1 and T2, respectively. In contrast, the TUG was significantly lower at T1 and T2 than at T0, and the TUG was also significantly lower at T2 than at T1. A total of 68.85%
(221/321) and 70.86% (248/350) of these patients exhibited a decrease in TUG at T1 and T2, respectively, and 59.81% (192/321) and 62.00% (217/350) demonstrated an improvement greater than
the MDC90 (2.49 sec) at T1 and T2, respectively. COMPARISONS BETWEEN FALLERS AND NON-FALLERS BEFORE AND AFTER PRIMARY TKA Table 3 shows that the mean age and percentage of female patients
were significantly higher in fallers than in non-fallers at T0 and T1, and the KL grade of the contralateral knee was significantly higher in fallers than in non-fallers at T0 to T2 (all
_Ps_ < 0.05). There were no significant differences in BMI, incision length, operative time or prosthesis type between fallers and non-fallers (all _Ps_ > 0.05). Figure 2 shows
balance-related outcomes between fallers and non-fallers. The AQoL and the ABC at T0 to T2 and the BBS at T0 and T2 were significantly lower in fallers than in non-fallers (all _Ps_ <
0.05). In contrast, the FES-I and the TUG were significantly higher in fallers than in non-fallers at T0 and T2 (all _Ps_ < 0.05). There were no significant differences in WOMAC (total
and subscales) or knee extension strength between fallers and non-fallers (all _Ps_ > 0.05). RISK FACTORS FOR FALLS BEFORE AND AFTER PRIMARY TKA We performed binary logistic regression
analysis of all factors, as shown in Table 3, to investigate the possible risk factors for falls before and after primary TKA. Table 4 shows that age (≥70 years), sex (female) and KL grade
of the contralateral knee (≥3) were significant independent risk factors for a history of falling in the last preoperative year and the first postoperative year, and the latter was also a
significant independent risk factor in the second postoperative year. DISCUSSION Knee OA is an established risk factor for falls, and TKA is the most frequently performed surgery to treat
end-stage knee OA32. Therefore, the impact of TKA on the incidence of falls and balance-related outcomes in OA patients and the possible risk factors for falls before and after TKA are of
considerable interest. This study found that the annual incidence of falls, AQoL, WOMAC (total and subscales), FES-I, ABC, knee extension strength, BBS and TUG improved significantly after
primary TKA compared to preoperative values. Age (≥70 years), sex (female) and KL grade of the contralateral knee (≥3) were identified as significant independent risk factors for falls in
the last preoperative year and the first postoperative year, and the latter was also an independent risk factor for falls in the second postoperative year after primary TKA. The reported
annual incidence of falls ranges from 11–34% in older Chinese community-dwelling people2, and the incidence is greater than 50% in people with knee OA and ranges from 7–40% in patients after
TKA5,7,8,18,19. We reported a relatively lower incidence before (14.89%) and after primary TKA (6.23% and 3.14% in the first and second postoperative year, respectively) compared to the
previous studies, which may be related to multiple factors, including fall-prevention strategies, data collection, and patient sources. Campbell _et al_. reported that single interventions
were as effective in reducing falls as interventions with multiple components33, but Gillespie _et al_. reported that interventions aimed to improve knowledge on fall-prevention alone did
not significantly reduce the risk of falls in older community-dwelling adults7. However, few studies compared the effects of interventions to improve fall-related knowledge on the incidence
of falls between community-dwelling people and post-TKA patients. The fall-prevention strategies performed in this study included interventions to improve fall-related knowledge and
functions. It is difficult to investigate whether increased fall-prevention knowledge alone affected the risk of falls after TKA. Fall-prevention strategies generally commence during the
preoperative period and appear to be most effective when they target high-risk populations or individuals33. However, the optimal timing and interventions to prevent falls before and after
TKA are rarely reported, and therefore, these factors are important areas for further study. Previous studies have also reported that fall recollection is commonly characterised by poor
sensitivity compared to prospective fall tracking34,35, and the active tracking of falls after surgery may lead to reduced falls simply from participant awareness that their falls were being
recorded (Hawthorne effect)36. A small number of patients in this study could not accurately recollect the details of the falls, especially before surgery, although most patients were very
sure of the number and details of their falls (Table 2). It also possible that some patients were unable to recollect their falls despite not presenting any obvious memory dysfunction, and
thus, the results may have underestimated the incidence of falls. The source of patients—approximately 70% of patients were from cities—may also have contributed to the low incidence of
falls in the study; however, the effect of living environment on the incidence of falls must be further investigated. Falls are the most frequent type of accident and the major cause of
injury-related hospitalization in the elderly. Falls may cause older people to become fearful of falling even when falls do not result in physical injury, which reduces quality of life,
restricts daily activities and results in the onset of functional decline37. Fear of falling is a common problem in people with lower limb arthritis and has serious consequences in relation
to reduced activity and loss of confidence and independence25. Significant reduction in fear of falling and an increase in balance confidence were found after TKA compared to before TKA in
this study, and this finding may be due, at least in part, to the considerable improvements in knee pain, stiffness and physical functions (WOMAC), which were consistent with previous
studies3,5,38. Levinger _et al_. found that the AQoL was significantly reduced 4 months postoperatively compared to preoperative scores, which may be primarily associated with impairments in
independent living and social relationships5. We found that the AQoL was slightly increased 1 year after surgery and remarkably improved 2 years after surgery, which indicates that the
quality of life improved at least 1 year after primary TKA. However, self-reported measures alone may fail to capture actual changes in physical ability following TKA and overestimate
performance changes39,40,41. Physical performance tests are necessary to further evaluate balance-related functions. Deficits in muscular function are consistently reported in patients with
knee OA and in patients who undergo knee arthroplasty6,42,43,44,45. Knee pain and quadriceps weakness affect the sensory and mechanical functions of the joint, and these factors are
associated with increased postural sway44,45,46,47, which results in balance difficulties and increased risk of falls48,49. Several methods for assessing knee extension strength have been
reported, such as direct measurement (Newton, pound and kilogram) and normalization to body mass and/or body height5,50,51. However, previous findings of altered knee extension strength
following TKA are inconsistent and controversial, and there is no consensus on which method performs best5,21,46,52,53. In this study, the knee extension strength was normalized to the
patient’s body height and body mass according to a previous study5 and was notably improved following primary TKA. There were no significant differences in normalized knee extension strength
between fallers and non-fallers, but the fallers exhibited relatively weaker strength than non-fallers. BBS and TUG are commonly used physical performance tests for lower limb
functions29,54, and these measurements are related to the risk of accidental falling in community dwelling adults55,56. Swinkels _et al_. reported increased BBS and reduced TUG (both
improvements) 6 months after TKA compared to preoperative values, and the differences between pre- and postoperative TUG reached statistical significance54. We performed this study using a
longer follow-up and found that BBS and TUG improved significantly 1 and 2 years after surgery compared to preoperative scores, which suggests that TKA improved the risk of accidental
falling in patients with knee OA. Various questionnaires and physical tests have been developed to assess balance-related functions3,18. However, these tests are not without limitations, and
there is no consensus on which tool performs best. Therefore, a combination of different tools has been suggested3,18. Swinkels _et al_. reported that BBS was significantly negatively
correlated with TUG and positively correlated with ABC, stiffness and physical functions of WOMAC before and after surgery. TUG was also significantly negatively correlated with ABC54. In
contrast, Minzner _et al_. reported poor concurrent validity between patient-reported and performance-based measures of physical functions in patients who undergo unilateral TKA57. The
present study also found that AQoL was positively correlated with BBS before surgery (_r_ = 0.15, _P_ < 0.01) and negatively correlated with TUG 1 year and 2 years after surgery (_r_ =
−0.13, _P_ = 0.02; _r_ = −0.13, _P_ = 0.01, respectively) and that ABC was negatively correlated with TUG 1 year after surgery (_r_ = −0.14, _P_ = 0.01). Differences in the time assessments
and the methods used may have affected these results, and further studies are needed to investigate the correlations between self-reported and physical performance outcomes for the risk for
falls and balance-related functions. Age and gender are important risk factors for falls, and older patients and women exhibit a higher likelihood of falling37,58. Our study found that age
(≥70 years) and gender (female) were significant independent risk factors for falls in patients with end-stage OA and during the first postoperative year following primary TKA. A large
proportion of patients who undergo TKA for the treatment of end-stage OA have concurrent OA in the contralateral knee22. Many studies demonstrated that pre- and postoperative factors in the
contralateral knee, such as pain and knee extension strength22,23, were associated with knee functions after TKA, but few studies investigated the impact of contralateral knee OA status on
falling. We found that the OA severity of the contralateral knee was an independent risk factor for falls before and after TKA, and KL grade ≥3 of the contralateral knee was associated with
an increased likelihood of falling. Therefore, surgeons and physiotherapists should pay more attention to contralateral knee status, in addition to age and gender, in patients with knee OA
before and after primary TKA when designing fall-prevention strategies. Several limitations must be considered when interpreting the findings of this study. First, the participants in this
study had primary and unilateral TKA due to OA. These results may only be generalized to individuals with similar characteristics, and further studies are warranted to expand the present
results and the generalizability to patients with bilateral or unicompartmental knee arthroplasty or other conditions (such as RA). Second, fall data were collected using interviews or
telephone calls, which primarily rely on the retrospective recall of falls by patients and may result in an underestimation of fall prevalence. Third, no non-surgical group with similar
severity of knee OA was recruited as control, and all patients in this study received a similar postoperative rehabilitation programme. Thus, this study was unable to establish the natural
course of falls and whether the postoperative rehabilitation accounted for the reduced incidence of falls. Fourth, although the strength testing data was normalized to body height and body
mass, the lever arm at the point of force application was not taken into account, and therefore, the data were not fully normalized to subject anthropometrics. Finally, other factors, such
as psychophysiological status, comorbidities and lifestyles were not documented and may have affected the results. However, to our knowledge, our findings reported the serial changes in the
incidence of falls and balance-related outcomes and identified possible risk factors for falls before and after primary TKA in the largest population and for the longest period of follow-up
of any existing study. In conclusion, the data of this study suggest that primary TKA is associated with a reduced incidence of falls and improved balance-related functions in patients with
OA. OA severity of the contralateral knee is a significant independent risk factor for falls, and surgeons and physiotherapists should pay more attention to the contralateral knee when
designing fall-prevention strategies before and after primary TKA in patients with OA. REFERENCES * Close, J. _et al_. Prevention of falls in the elderly trial (PROFET): a randomised
controlled trial. _Lancet_ 353(9147), 93–97 (1999). Article CAS PubMed Google Scholar * Kwan, M. M., Close, J. C., Wong, A. K. & Lord, S. R. Falls incidence, risk factors, and
consequences in Chinese older people: a systematic review. _J Am Geriatr Soc_ 59(3), 536–643 (2011). Article PubMed Google Scholar * Moutzouri M. _et al_. The effect of total knee
arthroplasty on patients’ balance and incidence of falls: a systematic review. _Knee Surg Sports Traumatol Arthrosc_ (2016). * Sibley, K. M., Beauchamp, M. K., Van Ooteghem, K., Straus, S.
E. & Jaglal, S. B. Using the systems framework for postural control to analyze the components of balance evaluated in standardized balance measures: a scoping review. _Arch Phys Med
Rehabil_ 96(1), 122–132.e129 (2015). Article PubMed Google Scholar * Levinger, P. _et al_. Physiological risk factors for falls in people with knee osteoarthritis before and early after
knee replacement surgery. _Knee Surg Sports Traumatol Arthrosc_ 19(7), 1082–1089 (2011). Article PubMed Google Scholar * Wang, X. _et al_. Mobility and muscle strength together are more
strongly correlated with falls in suburb-dwelling older chinese. _Sci Rep_ 6, 25420 (2016). Article ADS CAS PubMed PubMed Central Google Scholar * Gillespie, L. D. _et al_.
Interventions for preventing falls in older people living in the community. _Cochrane Database Syst Rev_ 9, Cd007146 (2012). * Williams, S. B., Brand, C. A., Hill, K. D., Hunt, S. B. &
Moran, H. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study.
_Arch Phys Med Rehabil_ 91(1), 106–114 (2010). Article PubMed Google Scholar * Xing, D. _et al_. Osteoarthritis and all-cause mortality in worldwide populations: grading the evidence from
a meta-analysis. _Sci Rep_ 6, 24393 (2016). Article ADS CAS PubMed PubMed Central Google Scholar * Fitzgerald, G. K., Piva, S. R. & Irrgang, J. J. Reports of joint instability in
knee osteoarthritis: its prevalence and relationship to physical function. _Arthritis Rheum_ 51(6), 941–946 (2004). Article PubMed Google Scholar * Schmitt, L. C., Fitzgerald, G. K.,
Reisman, A. S. & Rudolph, K. S. Instability, laxity, and physical function in patients with medial knee osteoarthritis. _Phys Ther_ 88(12), 1506–1516 (2008). Article PubMed PubMed
Central Google Scholar * Glyn-Jones, S. _et al_. Osteoarthritis. _Lancet_ 386(9991), 376–387 (2015). Article CAS PubMed Google Scholar * Vielgut, I. _et al_. Sports activity after
low-contact-stress total knee arthroplasty - a long term follow-up study. _Sci Rep_ 6, 24630 (2016). Article ADS CAS PubMed PubMed Central Google Scholar * Nguyen, U. S. _et al_. The
impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. _Osteoarthritis Cartilage_ 22(4),
527–534 (2014). Article PubMed PubMed Central Google Scholar * Sorensen, R. R., Jorgensen, M. G., Rasmussen, S. & Skou, S. T. Impaired postural balance in the morning in patients
with knee osteoarthritis. _Gait Posture_ 39(4), 1040–1044 (2014). Article PubMed Google Scholar * Duffell, L. D., Southgate, D. F., Gulati, V. & McGregor, A. H. Balance and gait
adaptations in patients with early knee osteoarthritis. _Gait Posture_ 39(4), 1057–1061 (2014). Article PubMed PubMed Central Google Scholar * Khalaj, N., Abu Osman, N. A., Mokhtar, A.
H., Mehdikhani, M. & Wan Abas, W. A. Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. _PLoS One_ 9(3), e92270 (2014). Article ADS PubMed
PubMed Central Google Scholar * Chan, A. C. & Pang, M. Y. Assessing Balance Function in Patients With Total Knee Arthroplasty. _Phys Ther_ 95(10), 1397–1407 (2015). Article PubMed
Google Scholar * Swinkels, A., Newman, J. H. & Allain, T. J. A prospective observational study of falling before and after knee replacement surgery. _Age Ageing_ 38(2), 175–181 (2009).
Article PubMed Google Scholar * D, L. R. & G, J. G. A longitudinal comparative study of falls in persons with knee arthroplasty and persons with or at high risk for knee
osteoarthritis. _Age Ageing_ 45(6), 794–800 (2016). Article Google Scholar * Petterson, S. C. _et al_. Improved function from progressive strengthening interventions after total knee
arthroplasty: a randomized clinical trial with an imbedded prospective cohort. _Arthritis Rheum_ 61(2), 174–183 (2009). Article PubMed Google Scholar * Maxwell, J. _et al_. The influence
of the contralateral knee prior to knee arthroplasty on post-arthroplasty function: the multicenter osteoarthritis study. _J Bone Joint Surg Am_ 95(11), 989–993 (2013). Article PubMed
PubMed Central Google Scholar * Zeni, J. A. Jr. & Snyder-Mackler, L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of
contralateral limb strength. _Phys Ther_ 90(1), 43–54 (2010). Article PubMed PubMed Central Google Scholar * Tilbury, C. _et al_. Outcome of total hip arthroplasty, but not of total
knee arthroplasty, is related to the preoperative radiographic severity of osteoarthritis. A prospective cohort study of 573 patients. _Acta Orthop_ 87(1), 67–71 (2016). Article PubMed
Google Scholar * Kempen, G. I. _et al_. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. _Age Ageing_ 37(1), 45–50 (2008). Article
PubMed Google Scholar * Faschingbauer M. _et al_. Predictive values of WOMAC, KOOS, and SF-12 score for knee arthroplasty: data from the OAI. _Knee Surg Sports Traumatol Arthrosc_ (2016).
* Berg, K. O., Maki, B. E., Williams, J. I., Holliday, P. J. & Wood-Dauphinee, S. L. Clinical and laboratory measures of postural balance in an elderly population. _Arch Phys Med
Rehabil_ 73(11), 1073–1080 (1992). CAS PubMed Google Scholar * Donoghue, D. & Stokes, E. K. How much change is true change? The minimum detectable change of the Berg Balance Scale in
elderly people. _J Rehabil Med_ 41(5), 343–346 (2009). Article PubMed Google Scholar * Podsiadlo, D. & Richardson, S. The timed “Up & Go”: a test of basic functional mobility for
frail elderly persons. _J Am Geriatr Soc_ 39(2), 142–148 (1991). Article CAS PubMed Google Scholar * Shumway-Cook, A., Brauer, S. & Woollacott, M. Predicting the probability for
falls in community-dwelling older adults using the Timed Up & Go Test. _Phys Ther_ 80(9), 896–903 (2000). CAS PubMed Google Scholar * Kennedy, D. M., Stratford, P. W., Wessel, J.,
Gollish, J. D. & Penney, D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. _BMC
Musculoskelet Disord_ 6, 3 (2005). Article PubMed PubMed Central Google Scholar * Arden, N. K. _et al_. Knee pain, knee osteoarthritis, and the risk of fracture. _Arthritis Rheum_ 55(4),
610–615 (2006). Article PubMed Google Scholar * Campbell, A. J. & Robertson, M. C. Rethinking individual and community fall prevention strategies: a meta-regression comparing single
and multifactorial interventions. _Age Ageing_ 36(6), 656–662 (2007). Article PubMed Google Scholar * Mackenzie, L., Byles, J. & D’Este, C. Validation of self-reported fall events in
intervention studies. _Clin Rehabil_ 20(4), 331–339 (2006). Article PubMed Google Scholar * Ganz, D. A., Higashi, T. & Rubenstein, L. Z. Monitoring falls in cohort studies of
community-dwelling older people: effect of the recall interval. _J Am Geriatr Soc_ 53(12), 2190–2194 (2005). Article PubMed Google Scholar * Sedgwick, P. & Greenwood, N. Understanding
the Hawthorne effect. _Bmj_ 351, h4672 (2015). Article PubMed Google Scholar * Gale, C. R., Cooper, C. & Aihie Sayer, A. Prevalence and risk factors for falls in older men and women:
the English longitudinal study of ageing. _Age Ageing_ 45(6), 789–794 (2016). Article PubMed PubMed Central Google Scholar * Swanik, C. B., Lephart, S. M. & Rubash, H. E.
Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. _J Bone Joint Surg Am_ 86-A(2), 328–334 (2004). Article
PubMed Google Scholar * Stratford, P. W., Kennedy, D. M., Maly, M. R. & Macintyre, N. J. Quantifying self-report measures’ overestimation of mobility scores postarthroplasty. _Phys
Ther_ 90(9), 1288–1296 (2010). Article PubMed Google Scholar * Stratford, P. W. & Kennedy, D. M. Performance measures were necessary to obtain a complete picture of osteoarthritic
patients. _J Clin Epidemiol_ 59(2), 160–167 (2006). Article PubMed Google Scholar * Stratford, P. W., Kennedy, D. M. & Woodhouse, L. J. Performance measures provide assessments of
pain and function in people with advanced osteoarthritis of the hip or knee. _Phys Ther_ 86(11), 1489–1496 (2006). Article PubMed Google Scholar * Shakoor, N. _et al_. Asymmetries and
relationships between dynamic loading, muscle strength, and proprioceptive acuity at the knees in symptomatic unilateral hip osteoarthritis. _Arthritis Res Ther_ 16(6), 455 (2014). Article
PubMed PubMed Central Google Scholar * Levinger, P. _et al_. Lower limb proprioception deficits persist following knee replacement surgery despite improvements in knee extension strength.
_Knee Surg Sports Traumatol Arthrosc_ 20(6), 1097–1103 (2012). Article PubMed Google Scholar * Cammarata, M. L., Schnitzer, T. J. & Dhaher, Y. Y. Does knee osteoarthritis
differentially modulate proprioceptive acuity in the frontal and sagittal planes of the knee? _Arthritis Rheum_ 63(9), 2681–2689 (2011). Article PubMed PubMed Central Google Scholar *
Hassan, B. S., Doherty, S. A., Mockett, S. & Doherty, M. Effect of pain reduction on postural sway, proprioception, and quadriceps strength in subjects with knee osteoarthritis. _Ann
Rheum Dis_ 61(5), 422–428 (2002). Article CAS PubMed PubMed Central Google Scholar * Valtonen, A., Poyhonen, T., Heinonen, A. & Sipila, S. Muscle deficits persist after unilateral
knee replacement and have implications for rehabilitation. _Phys Ther_ 89(10), 1072–1079 (2009). Article PubMed Google Scholar * Gauchard, G. C., Vancon, G., Meyer, P., Mainard, D. &
Perrin, P. P. On the role of knee joint in balance control and postural strategies: effects of total knee replacement in elderly subjects with knee osteoarthritis. _Gait Posture_ 32(2),
155–160 (2010). Article PubMed Google Scholar * Hunt, M. A. _et al_. Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee
osteoarthritis. _Osteoarthritis Cartilage_ 16(5), 591–599 (2008). Article CAS PubMed Google Scholar * Grabiner, M. D. _et al_. Trunk kinematics and fall risk of older adults: translating
biomechanical results to the clinic. _J Electromyogr Kinesiol_ 18(2), 197–204 (2008). Article PubMed Google Scholar * Huang, H., Guo, J., Yang, J., Jiang, Y., Yu, Y. Isokinetic
angle-specific moments and ratios characterizing hamstring and quadriceps strength in anterior cruciate ligament deficient knees. 7(1), 7269 (2017). * de Zwart, A. H. _et al_. Falls
Associated with Muscle Strength in Patients with Knee Osteoarthritis and Self-reported Knee Instability. _J Rheumatol_ 42(7), 1218–1223 (2015). Article PubMed Google Scholar * Fuchs, S.,
Thorwesten, L. & Niewerth, S. Proprioceptive function in knees with and without total knee arthroplasty. _Am J Phys Med Rehabil_ 78(1), 39–45 (1999). Article CAS PubMed Google Scholar
* Gage, W. H., Frank, J. S., Prentice, S. D. & Stevenson, P. Postural responses following a rotational support surface perturbation, following knee joint replacement: frontal plane
rotations. _Gait Posture_ 27(2), 286–293 (2008). Article PubMed Google Scholar * Swinkels, A. & Allain, T. J. Physical performance tests, self-reported outcomes, and accidental falls
before and after total knee arthroplasty: an exploratory study. _Physiother Theory Pract_ 29(6), 432–442 (2013). Article PubMed Google Scholar * Viccaro, L. J., Perera, S. &
Studenski, S. A. Is timed up and go better than gait speed in predicting health, function, and falls in older adults? _J Am Geriatr Soc_ 59(5), 887–892 (2011). Article PubMed PubMed
Central Google Scholar * Muir, S. W., Berg, K., Chesworth, B. & Speechley, M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a
prospective study. _Phys Ther_ 88(4), 449–459 (2008). Article PubMed Google Scholar * Mizner, R. L. _et al_. Measuring functional improvement after total knee arthroplasty requires both
performance-based and patient-report assessments: a longitudinal analysis of outcomes. _J Arthroplasty_ 26(5), 728–737 (2011). Article PubMed Google Scholar * Wei, F. & Hester, A. L.
Gender difference in falls among adults treated in emergency departments and outpatient clinics. _J Gerontol Geriatr Res_ 3, 152 (2014). PubMed PubMed Central Google Scholar Download
references ACKNOWLEDGEMENTS The authors would like to thank all of the patients who participated in this study, and the support of the China Postdoctoral Science Foundation (No.
2017M610604), the Postdoctoral Research and Development Project of Sichuan University (No. 2017SCU12041) and the Sichuan Provincial Health and Family Planning Commission Research Program
(No. 17PJ124). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Orthopaedics, West China Hospital, Sichuan University, Chengdu, 610041, China Hai-bo Si, Yi Zeng, Jian Zhong,
Zong-ke Zhou, Ning Ning & Bin Shen * Key Laboratory of Transplant Engineering and Immunology, West China Hospital, Sichuan University, Chengdu, 610041, China Hai-bo Si, Yan-rong Lu &
Jing-qiu Cheng Authors * Hai-bo Si View author publications You can also search for this author inPubMed Google Scholar * Yi Zeng View author publications You can also search for this
author inPubMed Google Scholar * Jian Zhong View author publications You can also search for this author inPubMed Google Scholar * Zong-ke Zhou View author publications You can also search
for this author inPubMed Google Scholar * Yan-rong Lu View author publications You can also search for this author inPubMed Google Scholar * Jing-qiu Cheng View author publications You can
also search for this author inPubMed Google Scholar * Ning Ning View author publications You can also search for this author inPubMed Google Scholar * Bin Shen View author publications You
can also search for this author inPubMed Google Scholar CONTRIBUTIONS Si H.b. and Ning N. conceived and designed this study. Si H.b., Ning N. and Shen B. recruited and monitored patients. Si
H.b., Zeng Y., Zhong J. and Zhou Z.k. gathered the data. Si H.b., Lu Y.r., Cheng J.q., Ning N. and Shen B. analysed and interpreted the data. Si H.b. and Ning N. drafted the manuscript. All
authors approved the manuscript. CORRESPONDING AUTHORS Correspondence to Ning Ning or Bin Shen. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare that they have no competing
interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND
PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any
medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The
images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not
included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly
from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Si, Hb., Zeng, Y.,
Zhong, J. _et al._ The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritis. _Sci Rep_ 7, 16583 (2017).
https://doi.org/10.1038/s41598-017-16867-4 Download citation * Received: 08 June 2017 * Accepted: 18 November 2017 * Published: 29 November 2017 * DOI:
https://doi.org/10.1038/s41598-017-16867-4 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Video Author Angeline Boulley talks about her new book, 'Firekeeper’s Daughter' - ABC NewsABC NewsVideoLiveShowsShopStream onTrump at West Point LatestLatestNew Orleans jailbreak Memorial Day weekend Boeing dea...
Real estate news headlines - 9NewsBuyer coughs up $3.6 million for six car spots in Sydney CBDOne lucky buyer has just spent a jaw-dropping amount of mone...
Life quickly finds a way: the surprisingly swift end to evolution’s big bangThe Cambrian explosion more than 500 million years ago is often considered biology’s “big bang”. Virtually all the major...
Doubled shapiro steps in a dynamic axion insulator josephson junctionABSTRACT Dynamic axion insulators feature a time-dependent axion field that can be induced by antiferromagnetic resonanc...
Prince harry was phone-hacking victim, london court rulesBritain's Prince Harry, Duke of Sussex, leaves the High Court in London, Britain March 27, 2023. Henry Nicholls | R...
Latests News
The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritisABSTRACT Knee osteoarthritis (OA) is an established risk factor for falls and balance impairment. This study investigate...
The rip3-rip1-nf-κb signaling axis is dispensable for necroptotic cells to elicit cross-priming of cd8+ t cellsAccess through your institution Buy or subscribe Apoptosis and necroptosis are two types of programmed cell death with d...
Many small communes in france yet to finalise address changesTHE NEW LAW MEANS THAT EVERYONE WILL HAVE AN OFFICIAL ADDRESS DO YOU RECEIVE THE CONNEXION'S FREE WEEKDAY NEWSLETTE...
The "labour together" report is a portrait of a party in crisis | thearticleThe response to the “Labour Together” report has shown it to be something of a Rorschach test. Most people can see somet...
3 Supreme Court Cases That Could Affect Older WorkersBy: Kenneth Terrell Published October 01, 2018 The U.S. Supreme Court started its 2018 term this week. The eight justi...