Ca2+ signals are essential for t-cell proliferation, while zn2+ signals are necessary for t helper cell 1 differentiation
Ca2+ signals are essential for t-cell proliferation, while zn2+ signals are necessary for t helper cell 1 differentiation"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
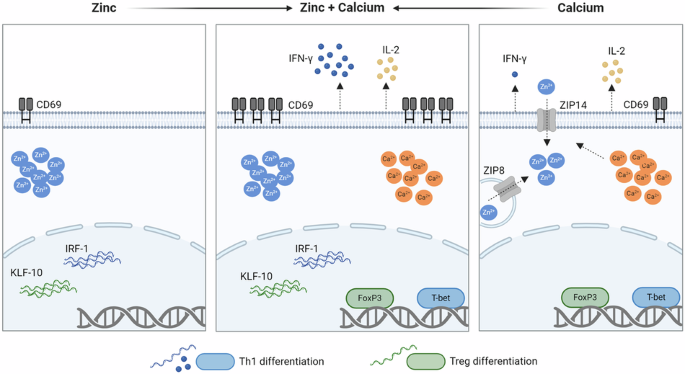
ABSTRACT The regulation of T-cell fate is crucial for the balance between infection control and tolerance. Calcium (Ca2+) and zinc (Zn2+) signals are both induced after T-cell stimulation,
but their specific roles in the fate of activation and differentiation remain to be elucidated. Are Zn2+- and Ca2+ signals responsible for different aspects in T-cell activation and
differentiation and do they act in concert or in opposition? It is crucial to understand the interplay of the intracellular signals to influence the fate of T cells in diseases with
undesirable T-cell activities or in Zn2+-deficient patients. Human peripheral blood mononuclear cells were stimulated with the Zn2+ ionophore pyrithione and thapsigargin, an inhibitor of the
sarcoplasmic/endoplasmic reticulum Ca2+ ATPase (SERCA). Intracellular Zn2+ and Ca2+ signals were monitored by flow cytometry and ELISA, quantitative PCR and western blot were used to
evaluate T-cell differentiation and the underlying molecular mechanism. We found that Zn2+ signals upregulated the early T-cell activation marker CD69, interferon regulatory factor 1
(IRF-1), and Krüppel-like factor 10 (KLF-10) expression, which are important for T helper cell (Th) 1 differentiation. Ca2+ signals, on the other hand, increased T-bet and Forkhead box P3
(FoxP3) expression and interleukin (IL)-2 release. Most interestingly, the combination of Zn2+ and Ca2+ signals was indispensable to induce interferon (IFN)-γ expression and increased the
surface expression of CD69 by several-fold. These results highlight the importance of the parallel occurrence of Ca2+ and Zn2+ signals. Both signals act in concert and are required for the
differentiation into Th1 cells, for the stabilization of regulatory T cells, and induces T-cell activation by several-fold. This provides further insight into the impaired immune functions
of patients with zinc deficiency. SIMILAR CONTENT BEING VIEWED BY OTHERS STIM1-MEDIATED NFAT SIGNALING SYNERGIZES WITH STAT1 TO CONTROL T-BET EXPRESSION AND TH1 DIFFERENTIATION Article 21
February 2025 THE TETRASPANIN CD151 MARKS A UNIQUE POPULATION OF ACTIVATED HUMAN T CELLS Article Open access 25 September 2020 THE CHAPERONIN CCT8 CONTROLS PROTEOSTASIS ESSENTIAL FOR T CELL
MATURATION, SELECTION, AND FUNCTION Article Open access 03 June 2021 INTRODUCTION The activation threshold of T lymphocytes and the regulation of T-cell fate are critical for the balance
between infection control and tolerance. Once activated, T cells proliferate and differentiate to mediate a highly specific immune response [1]. Stimulation of the T-cell receptor (TCR)
causes the distribution of calcium (Ca2+) signals throughout the cell, depending on the potency of the antigen [2]. An initial Ca2+ signal is induced by inositol-1,4,5-trisphosphate, causing
the release of Ca2+ from the endoplasmic reticulum (ER) into the cytosol. The depletion of Ca2+ from the ER stores is detected by sensors stromal interaction molecule 1 (STIM1) which
interacts with ORAI1 in the plasma membrane and thus activating calcium release-activated calcium (CRAC) channels. This induces a store-operated calcium entry (SOCE) from the synaptic cleft.
The potentiated Ca2+ signal then causes the translocation of the nuclear factor of activated T cells (NFAT) into the nucleus and thereby the expression of important genes for cell
proliferation, such as interleukin (IL) 2 [3,4,5]. In addition to Ca2+ signals, zinc (Zn2+) signals have also become a focus of interest. Zn2+ is an essential trace element which is present
in the serum with mean concentrations of 84.9 and 80.6 µg/dL in men and women, respectively [6]. Within cells, Zn2+ is mostly bound to proteins such as metallothionein [7], or to
Zn2+-binding S100 proteins such as calprotectin and calgranulin [8]. Additionally, Zn2+ is also present freely or loosely bound in the picomolar to nanomolar range. Intracellular Zn2+
signals can occur within seconds after stimulation influencing signaling cascades (zinc flux). Therefore, Zn2+ is also regarded as a second messenger [9, 10]. Slower Zn2+ signals have also
been described in mast cells, occurring a few minutes after receptor stimulation in a Ca2+-dependent manner and are referred to as “zinc wave” [11]. Stimulation of cells may additionally
cause changes in Zn2+ homeostasis after a few days, thereby affecting gene expression [10]. In T cells especially, it has been shown that after stimulation of the TCR via dendritic cells,
Zn2+ influx from the extracellular space occurs within 1 min, depending on the Zn2+ transporter Zip6. This signal occurred mostly in the subsynaptic region of the immunological synapse [9].
This is also seen in CRAC channel-mediated calcium influx where high concentrations of calcium are localized to the subsynaptic region [12, 13]. However, calcium signals were found to
rapidly diffuse throughout the cell [14]. When Zn2+ influx via Zip6 is inhibited, the activation markers CD25 and CD69 are less expressed, indicating that T-cell activation is impaired [15].
In addition, the Zn2+ transporter Zip8 is upregulated after T-cell activation, causing the release of Zn2+ from lysosomes into the cytoplasm. However, when Zip8 expression is inhibited, the
reduced cytoplasmic Zn2+ results in reduced interferon (IFN)-γ expression [16] and thus in T helper cell (Th) 1 differentiation. Many studies have highlighted the importance of Zn2+ in
maintaining the balance between Th1/Th2 [17, 18] in inducing regulatory T cells [19, 20]. The interplay between Zn2+ and Ca2+ signaling has also been partly investigated. Extracellular Zn2+
can sustain Ca2+ signaling after T-cell receptor stimulation [9], and in the human T-cell line Jurkat, it was seen that different stimulants used for T-cell activation induce either a Ca2+
or a Zn2+ signal [21]. However, the mechanism by which Zn2+ and Ca2+ act in parallel has yet to be examined. Therefore, we investigated whether Zn2+ and Ca2+ signals are responsible for
different aspects in T-cell activation and differentiation. We focused on the single and combined effects of Zn2+ and Ca2+ signals independent of other activating stimulants. RESULTS
INDUCTION OF ZN2+ AND CA2+ SIGNALS To investigate the individual and the combined effects of Zn2+ and Ca2+ signals, we separately induced intracellular Zn2+ signals using the Zn2+ ionophore
pyrithione (Fig. 1A) and Ca2+ signals using thapsigargin in peripheral blood mononuclear cells (PBMC) (Fig. 1B). Thapsigargin inhibits the sarcoplasmic/endoplasmic reticulum Ca2+ ATPase
(SERCA) and thereby reduces the transport of Ca2+ into the endoplasmic reticulum, which results in an accumulation of Ca2+ in the cytosol [22]. PBMC were stimulated with increasing
concentrations of pyrithione (0.25–2 µM) or thapsigargin (5–150 µM). First, the cell viability was investigated by propidium iodide staining and no significant increase in dead PI+
lymphocytes was observed (Fig. S1A, B). Even with the combined stimulation with pyrithione and thapsigargin, no significant increase in dead PI+ lymphocytes was found (Fig. S1C). Then, the
induction of intracellular Zn2+ and Ca2+ signals was measured by flow cytometry 10 min after stimulation. We confirmed that pyrithione and thapsigargin increased the intracellular Zn2+ and
Ca2+ concentrations, respectively, in a dose-dependent manner (Fig. 1A, B). 0.35 and 0.5 µM pyrithione increased the mean intracellular Zn2+ concentration from 0.048 to 0.171 and 0.248 nM,
respectively. For the following experiments, 0.35 and 0.5 µM pyrithione were used, since Zn2+ acts in the nanomolar concentration range [23]. For Ca2+ signals, 50 ng/ml thapsigargin was used
because it significantly increased mean intracellular Ca2+ levels from 18.4 to 164.5 nM. At 220 nM intracellular Ca2+ and above, maximal proliferation is induced in T cells [24]. However,
to be able to study the effect of Zn2+ in parallel, we decided to use a lower Ca2+ signal. Importantly, thapsigargin did not cause an increase in intracellular Zn2+ and pyrithione did not
induce a Ca2+ signal (Fig. 1A, B). In addition to pyrithione, which imports extracellular Zn2+ into the cell, the NO donor _S_-nitrosocysteine (SNOC) has been used to release Zn2+ from
intracellular sources as shown in some signaling pathways [25, 26]. SNOC releases Zn2+ bound to metallothionein by S-nitrosylation [27, 28]. In initial experiments, SNOC elicited only a very
small Zn2+ signal 10 min after stimulation, so we examined intracellular Zn2+ concentration in a 15-min interval. SNOC significantly increased the intracellular free Zn2+ concentration
after 30 min which is slower than pyrithione (Fig. 1C). Therefore, we decided to preincubate with SNOC for 30 min in the following experiments and then stimulate additionally with
thapsigargin. ZN2+ AND CA2+ SIGNALS ACTIVATE T CELLS IN A P38 MAPK-DEPENDENT MANNER First, we investigated the activation of T cells after stimulation with pyrithione, thapsigargin, and a
combination of both. Therefore, the surface expression of the early activation marker CD69 in CD3+ T cells was measured 48 h after stimulation with flow cytometry. We found that pyrithione
and thapsigargin individually upregulate CD69 expression in T cells in 12–20% of lymphocytes (Fig. 2A). However, when PBMC were stimulated simultaneously with different concentrations of
pyrithione and thapsigargin, 45.1 and 53.9% of lymphocytes were activated, respectively, and a distinct CD3+CD69+ population emerged (Fig. 2B). Therefore, Zn2+ and Ca2+ signals
synergistically induce CD69 expression, which is important for the retention of activated T cells in the lymph node [29]. In comparison, SNOC increased CD69 expression, and when combined
with thapsigargin, CD69 expression was also further increased (Fig. 2C). However, on average, SNOC + thapsigargin activated fewer T cells (28.3%) than pyrithione + thapsigargin (0.5 µM
pyrithione +thapsigargin: 53.9%). Therefore, in the following study, we focused on Zn2+ signals induced by pyrithione and not by SNOC. However, this experiment shows that also intracellular
Zn2+ release is able to synergize with Ca2+ signals. We next investigated proteins involved in the upregulation of CD69 by Ca2+ and Zn2+ signals. We focused on p38 mitogen-activated protein
kinase (p38 MAPK), which is activated upon T-cell receptor stimulation, by CD28 and IL-12/IL-18 receptor signaling. Further, p38 MAPK is important for CD69 expression in cytokine-stimulated
T cells [30], and is critical for differentiation into Th1 or Th2 cells [31] and has been shown to be activated by Zn2+ [32]. Therefore, we investigated whether T-cell activation by
pyrithione and thapsigargin is also mediated via p38 MAPK. First, we found that phosphorylation of p38 was increased in PBMC after thapsigargin stimulation and was further enhanced by
additional stimulation with pyrithione (Fig. 2D). Therefore, we preincubated PBMC for 30 min with the specific p38 MAPK inhibitor SB202190 and subsequently stimulated with pyrithione and
thapsigargin. It was found that the strong expression of CD69 induced by pyrithione and thapsigargin was significantly reduced when p38 MAPK was inhibited (Fig. 2E). ONLY ZN2+ PLUS CA2+
INDUCES DIFFERENTIATION INTO TH1 CELLS After T-cell activation, the release of growth factor interleukin (IL)-2 is important for T-cell proliferation and the development of regulatory T
cells (Treg) [33]. In Zn2+ deficiency, IL-2 expression is reduced [34, 35] whereas Zn2+ had no impact on IL-2 expression in mixed lymphocyte cultures [19]. Therefore, we were interested in
the individual functions of Zn2+ and Ca2+ signals in IL-2 regulation. IL-2 secretion by PBMC was measured 48 h after stimulation by ELISA. The results showed that stimulation with pyrithione
had no effect on IL-2 expression, whereas thapsigargin increased IL-2 secretion (Fig. 3A). Pyrithione did not enhance IL-2 production by thapsigargin. This was also not seen in experiments
with lower thapsigargin concentrations. 10 ng/ml thapsigargin did not significantly induce IL-2 production with or without pyrithione costimulation (Fig. S2). These results suggest that only
Ca2+, but not Zn2+ signaling is critical for IL-2 release. However, we found that the induction of IL-2 by thapsigargin depends on extracellular Zn2+, as the thapsigargin stimulation in
Zn2+-deficient (ZD) medium did not induce a significant release of IL-2 (Fig. 3B). Further, it has already been shown that Zn2+ affects the balance of Th1 and Th2 cells and induces Treg
cells [36, 37]. Therefore, we investigated how pyrithione and thapsigargin affect T-cell differentiation. To investigate the differentiation into Th1 cells, the characteristic cytokine IFN-γ
was determined. By qPCR and ELISA, IFN-γ was shown to be partially upregulated by pyrithione and thapsigargin, but the combined stimulation greatly increased its expression (Fig. 3C, D).
This was not only seen in PBMC but also in isolated naïve CD4+ T cells (Fig. S3). Therefore, we examined T-bet, which is critical for Th1 differentiation and a key transcription factor of
IFN-γ expression [38]. Interestingly, T-bet was regulated differently from IFN-γ. T-bet was induced by thapsigargin alone and was not further increased by pyrithione but rather decreased
with high pyrithione concentrations (Fig. 3E). Thus, T-bet cannot explain the increased expression of IFN-γ by thapsigargin and pyrithione. Therefore, we further examined the transcription
factor IRF-1 (interferon regulatory factor 1), which is also involved in Th1 differentiation. IRF-1 increases the responsiveness to IL-12, and Irf1−/− CD4+ T cells showed reduced IFN-γ
production [39, 40]. In our experiments, IRF-1 expression was examined at the mRNA level 3 h after stimulation and was significantly increased by 0.35 µM pyrithione and by the combination of
pyrithione and thapsigargin (Fig. 3F). In contrast, thapsigargin did not affect IRF-1 expression. The Ca2+ dependence of T-bet and the Zn2+ dependence of IRF-1 could jointly explain the
increase in IFN-y in the presence of simultaneous Zn2+ and Ca2+ signals. Moreover, the induction of T-bet and IRF-1 (Fig. 4A, B) and the release of IFN-γ (Fig. 4C) by thapsigargin and
pyrithione are dependent on p38 MAPK activity. Additionally, we investigated if Zn2+ induces T-cell activation and IFN-γ expression in dependence of the protein kinase C (PKC). Phorbol
12-myristate 13-acetate (PMA) and calcium ionophores are commonly used for T-cell activation [41] and PMA stimulation was already shown to increase intracellular Zn2+ levels in Jurkat T
cells [21]. Thus, the question arose if Zn2+ mimics the effect of PMA costimulation. Thus, experiments were performed in the presence of the PKC inhibitor bisindolylmaleimide (BIS) II (Fig.
S4) [42]. We found that thapsigargin and pyrithione still synergistically increased the CD69 expression (Fig. S4A) and that also the IFN-γ expression by thapsigargin and pyrithione was not
reduced in the presence of the PKC inhibitor (Fig. S4B). Thus, the effects of Zn2+ are not dependent on PKC and Zn2+ does not mimic the costimulatory effect of PMA. We next investigated how
thapsigargin causes a small IFN-γ release even in the absence of a Zn2+ signal via pyrithione. As shown above in Fig. 1A, thapsigargin does not induce a rapid Zn2+ flux. Therefore, we
examined the effect of thapsigargin on the intracellular Zn2+ homeostasis and found that intracellular Zn2+ was significantly increased 48 h after stimulation (Fig. 5A). This can be
explained by the altered Zn2+ transporter expression 3 h after stimulation with thapsigargin (Fig. 5B, C). The mRNA expression of the Zn2+ importer Zip8 and Zip14 were significantly
upregulated whereas Zip9 was downregulated by thapsigargin (Fig. 5B). The Zn2+ exporter ZnT1, ZnT4-7 and ZnT9 were not affected (Fig. 5C) whereas Zip2, Zip4, Zip5, Zip10-12, ZnT2, ZnT3, ZnT8
and ZnT10 were not detectable in PBMC. In comparison we found that the stimulation with pyrithione and thapsigargin also significantly increased Zip14 expression (Fig. S5A). Zip6 was
significantly upregulated which shows the same trend as with thapsigargin stimulation alone. In contrast, Zip8 was downregulated. Furthermore, the zinc exporter ZnT1 was upregulated and ZnT5
and ZnT6 were downregulated with combined thapsigargin and pyrithione stimulation (Fig. S5B). Given this impact of thapsigargin on Zn2+ homeostasis, we wondered whether thapsigargin still
induces the release of IFN-γ even in the absence of extracellular Zn2+. For this purpose, PBMC were stimulated with thapsigargin in normal cell culture medium or Chelex-treated
Zn2+-deficient (ZD) medium. Interestingly, without extracellular Zn2+, thapsigargin did not induce the release of IFN-γ (Fig. 5D). Since the Chelex® resin used to produce the ZD medium
removes divalent cations, we measured the depletion of Zn, Ca, Mg, Cu, Fe, and Mn (Table S1). Subsequently, the removed metal ions including Zn2+ were reconstituted accordingly (3.59 µM
ZnSO4/234.6 µg/L Zn) and the Zn2+-reconstituted (ZR) medium was measured again. A Zn2+-deficient (ZD) medium in these experiments was obtained by reconstituting all metal ions except Zn2+
(Table S1). We found that in ZR culture medium, thapsigargin-induced IFN-γ expression was significantly increased in comparison to the stimulation in ZD medium (Fig. S6). Therefore, these
results conclude that thapsigargin stimulation increases the IFN-γ expression in a Zn2+-depend way by altering the Zn2+ transporter expression and thus increasing intracellular Zn2+. TH2,
TH17 AND TREG DIFFERENTIATION AFTER ZN2+ AND CA2+ SIGNALS In addition to the markers for Th1 differentiation, we also examined characteristic cytokines and transcription factors of Th2, Th17
and Treg cells by ELISA and western blot. The cytokines IL-10 (Th2) and IL-17 (Th17) were not induced either by Zn2+ or Ca2+ signals (Fig. 6A, B). The concentrations were below the
detection limits of the respective ELISA. The transcription factors GATA-3 (Th2) and RORC2 (Th17) were also not altered by thapsigargin and pyrithione (Fig. 6C, D). Zn2+ and Ca2+ signals
alone accordingly did not induce differentiation into Th2 and Th17 cells. Forkhead box P3 (FoxP3) is a characteristic transcription factor of Treg cells [43]. FoxP3 was induced by
thapsigargin but was not affected by pyrithione (Fig. 7A). This result was unexpected, as Zn2+ supplementation has already been shown to stabilize FoxP3 expression and to induce Treg [19,
20]. Therefore, we additionally investigated whether thapsigargin can also induce FoxP3 in Zn2+ depletion. It was found that in Chelex-treated Zn2+-deficient medium thapsigargin can no
longer induce FoxP3 (Fig. 7B). Like pyrithione, ZnSO4 had no additional effect on FoxP3 expression. We further examined the transcription factor KLF-10 (Krüppel-like factor 10), which
suppresses differentiation into Th1 and instead promotes differentiation into Treg [44]. KLF-10 was significantly induced by pyrithione but was not affected by thapsigargin, nor further
induced by the combination with pyrithione and thapsigargin (Fig. 7C). The induction of KLF-10 by pyrithione was also dependent on p38 MAPK (Fig. 7D). DISCUSSION In this study we focused on
the mechanism of how Zn2+ and Ca2+ signals act in parallel in the induction of T-cell activation and differentiation. We found that Zn2+ and Ca2+ regulate different aspects but that the
presence of both signals is critical for T-cell activation, Th1 differentiation and Treg function. As a marker of early T-cell activation, we investigated CD69 expression, which is important
for the retention of activated T cells in lymph nodes but is also involved in T-cell differentiation [29, 45]. We have shown that Ca2+ and Zn2+ signals individually cause a low level of
T-cell activation (CD69), but that both signals in combination amplify the CD69 expression several-fold. Zn2+ and Ca2+ signals upregulate the CD69 expression in CD3+ T cells in a p38
MAPK-dependent manner. However, when p38 MAPK was inhibited, the CD69 expression was not fully reduced to the control level, suggesting that on the one hand p38 MAPK, but also other
signaling molecules are important for the effects of Zn2+ and Ca2+ on CD69 expression. Furthermore, we have investigated if the Zn2+ signal mimics the costimulatory effect seen by PMA [41]
since it was shown that PMA stimulation increases intracellular Zn2+ levels [21]. Thus, we have examined the role of PKC by using the inhibitor BIS II. Our results demonstrate that the
synergistic effects of thapsigargin and pyrithione do not depend on the PKC. Further, the release of IL-2, which is important for cell proliferation, was only induced by Ca2+ signals. Ca2+
activates calcineurin, which in turn dephosphorylates NFAT to induce IL-2 transcription [5]. Zn2+ signals had no effect on the IL-2 expression. However, in alternative T-cell stimulation
models, the importance of Zn2+ in regulating IL-2 has been previously demonstrated. After stimulation with concanavalin A or PMA and ionomycin high extracellular Zn2+ has been shown to
inhibit calcineurin and IL-2 expression [46]. Conversely, in Zn2+ deficiency, IL-2 expression has been shown to be downregulated in a CREMα-dependent manner [34, 35]. This is consistent with
our results showing that thapsigargin-induced IL-2 release is not induced in Zn2+-deficient medium. Additionally, Zn2+ did not affect the release of IL-2 in mixed lymphocyte cultures [19].
Moreover, we focused on the role of Zn2+ and Ca2+ in the differentiation into Th1 cells. The individual signals barely triggered the release of IFN-γ, but in combination the IFN-γ expression
was highly increased. Unexpectedly, the major transcription factor T-bet was differentially regulated than IFN-γ and was only induced by Ca2+ but not Zn2+. Thus, Zn2+ seems to induce IFN-γ
independently from T-bet expression, so accordingly we investigated IRF-1 regulation. IRF-1 is an important regulator of Th1 differentiation which enhances IL-12 signaling and thus increased
IFN-γ expression. In previous studies Irf1−/− CD4+ T cells showed reduced IFN-γ production [39, 40] and IRF-1 is also upregulated by Zn2+ in unstimulated PBMC [47]. In our experiments we
show that Zn2+ but not Ca2+ upregulated IRF-1. Thus, only when Zn2+ and Ca2+ signals were combined, resulting in IRF-1 and T-bet upregulation respectively, the IFN-γ release increased
several-fold. This agrees well with the observation that people in Zn2+ deficiency have an impaired IFN-γ release [48]. However, Zn2+ might affect IFN-γ release by other factors as well and
future studies are necessary to clarify the role of IRF-1. For example, it was previously published that Zn2+ deficiency affects IFN-γ on the post-transcriptional level [49]. Additionally,
experiments were performed in PBMC which have mixed populations of T cells, B cells, natural killer (NK) cells, monocytes and dendritic cells. Thus, the regulation of IFN-γ by T-bet and
IRF-1 might not only be specific for T cells and other cell types, particularly NK cells [50], could be masking the T-cell response. Nevertheless, we confirmed the synergistic effect of
thapsigargin and pyrithione in IFN-γ production in isolated CD4+ T cells. Further, we focused on the low IFN-γ release by single Ca2+ signals. We found that Ca2+ upregulates specific Zn2+
transporters, leading to an increase in intracellular Zn2+ and thus upregulating IFN-γ to a small extent. The Zn2+ transporter Zip4 and Zip14 are located in the plasma membrane [51] and
their upregulation results in increased import of Zn2+ from the extracellular space into the cell. Zip8 is located in the lysosomal membrane [51] and its upregulation results in increased
transport of Zn2+ from the lysosomes into the cytoplasm. Zip8 is already known to be strongly upregulated after T-cell activation [16]. Aydemir et al. have shown that Zip8 is important for
IFN-γ expression because the released Zn2+ via Zip8 inhibits calcineurin and thus sustains CREB phosphorylation which results in increased IFN-γ [16]. The importance of Zip8 and Zn2+ in
IFN-γ expression was further highlighted in studies with proton-pump inhibitors [52] and is currently further investigated in our group in the elderly population. Complementary to Aydemir et
al. [16] our results suggest that the upregulation of Zip8 is induced by the Ca2+ signal which occurs after T-cell receptor stimulation. However, the stimulation with pyrithione and
thapsigargin downregulated Zip8 in our experiments, demonstrating a different zinc transporter pattern 3 h after stimulation than in T-cell stimulation via the TCR 48 h after stimulation
[16]. Zip14 is evolutionary closely related to Zip8 [51] and its upregulation was shown before by phytohaemagglutinin and T-cell receptor stimulation in PBMC, respectively. In addition,
Zip14 was also upregulated by the combined stimulation with pyrithione and thapsigargin. Zip14 is located in the plasma membrane and emphasizes the importance of extracellular Zn2+ [51].
However, the function of Zip14 in lymphocytes remains to be elucidated [16, 53]. The mRNA of the transporter Zip9-11 was downregulated, but as the overall Zn2+ increased, this seemed not to
have a great impact. As a result of the altered Zn2+ transporter expression we measured an increase in intracellular Zn2+. Zn2+ was essential for the Ca2+-induced IFN-γ release, since under
extracellular Zn2+ deficiency thapsigargin did not induce IFN-γ release. This is comparable to the described “homeostatic Zn2+ signal”, because the Zn2+ concentration was increased 48 h
after stimulation due to altered transporter expression [23]. In addition to Th1 differentiation, we showed the importance of Zn2+ and Ca2+ in Treg differentiation. Ca2+ signals induced the
expression of FoxP3, but Zn2+ had no effect on FoxP3. This result was unexpected, as Zn2+ supplementation has already been shown to be important for FoxP3 expression and to induce Treg in
other T-cell activation models [19, 20]. Therefore, we examined the expression of FoxP3 after stimulation with thapsigargin under extracellular Zn2+ deficiency and found that FoxP3 was no
longer upregulated. This confirms previous observations that Zn2+ is necessary for the stabilization of FoxP3 [19]. In contrast, KLF-10 was only upregulated by Zn2+ but not by Ca2+
signaling. KLF-10 suppresses differentiation into Th1 and instead promotes differentiation into Treg [44]. While Th1 and Treg cell differentiation was induced with pyrithione and
thapsigargin stimulation, a differentiation into Th2 and Th17 cells was not observed, as no IL-10 and IL-17 was produced. However, the importance of Ca2+ signals for Th2 and Th17
differentiation, respectively, was described before. In murine T cells, the calcium ionophore ionomycin alone was shown to induce IL-4 production in a p38 and NFAT-dependent manner [54].
Therefore, the characteristic Th2 cytokines IL-4, IL-5 and IL-13 [55] could also be induced by thapsigargin and could be investigated in future studies. Our experiments have shown that p38
phosphorylation is enhanced by the combined stimulation of thapsigargin and pyrithione, suggesting that p38-dependent IL-4 expression [54] might also be synergistically affected by Zn2+
signaling. In the differentiation of Th17 cells, the store-operated calcium entry increased the development of a pathogenic Th17 phenotype [56]. Blocking the pore subunit of CRAC channels
Orai1 impaired Th17 differentiation more than Th1 and Th2 cell differentiation [57]. However, further studies demonstrated an increased Th17 differentiation with low strength T-cell
stimulation and a reduction of Th17 when a Ca2+ ionophore was added [58]. Thus, Ca2+ signaling regulates the differentiation into T17 cells, however in our experiments the induction of Th17
cells was not observed. This might be due the missing stimulation via the TCR or a low threshold Ca2+ signal via thapsigargin. Additionally, Zn2+ supplementation was shown to decrease the
amount of Th17 cells, so no enhancing effect of Zn2+ and Ca2+ signals was expected [59, 60]. The results of this study reinforce the relevance of Zn2+ signaling in addition to the well-known
Ca2+ signals and differentiate the effects in activation and differentiation of T cells. This is of great importance for understanding the basic mechanisms of T-cell fate. In summary, we
have demonstrated different levels of Zn2+ and Ca2+ action. Zn2+ signals are essential for complementing Ca2+ signals in the activation of T cells and, in particular, Th1 differentiation,
which is important for defense against intracellular pathogens. MATERIALS AND METHODS ISOLATION OF PERIPHERAL BLOOD MONONUCLEAR CELLS (PBMC) After obtaining informed consent and explaining
the nature and potential consequences of the studies, human venous blood was drawn from healthy volunteer donors, anticoagulated with sodium heparin (B. Braun, Melsungen, Germany) and
diluted 1:2 in PBS (Sigma-Aldrich, Steinheim, Germany). PBMC were isolated from whole blood using Lymphocytes Separation Media, 1.077 g/ml (Capricorn Scientific, Ebsdorfergrund, Germany).
Isolated PBMC were washed in PBS and adjusted to a final concentration of 1 × 106 cells/mL in culture medium with or without Zn2+. The zinc-adequate (ZA) culture medium consisted of
RPMI-1640 (Sigma-Aldrich) supplemented with 10% heat-inactivated fetal calf serum (FCS) “Low Endotoxin” (Bio&Sell, Feucht, Germany) 2 mM l-glutamine, 100 U/mL potassium penicillin and
100 U/mL streptomycin sulfate (all from Sigma-Aldrich). To incubate cells in medium without Zn2+, the described medium was treated for 1 h with Chelex® 100 sodium form (Sigma-Aldrich) to
chelate all divalent cations. Afterwards, 500 µM CaCl2 and 400 µM MgCl2 (both from Merck, Darmstadt, Germany) were reconstituted and the pH was adjusted back to the level of the culture
medium (pH 7.4). Finally, the Zn2+-deficient (ZD) medium was sterile filtered. The Zn2+ depletion was always confirmed by atomic absorption spectrometry using an AAnalyst 800 (Perkin-Elmer,
Waltham, USA). For experiments with Zn2+-reconstituted medium (ZR), the Chelex®-treated medium was measured by inductively coupled plasma mass spectrometry (ICP-MSMS) (Agilent 8900 ICP-MSMS,
Agilent Technologies, Waldbronn, Germany). The concentration of the metal ions Zn, Ca, Mg, Cu, Fe and Mn were measured in samples that were diluted with nitrogenic acid, using rhodium as an
internal standard (Table S1). To obtain a ZR-medium all removed metal ions were reconstituted accordingly and the ZR-medium was measured again by ICP-MS. T-CELL ISOLATION Naïve CD4+ T cells
were isolated using the MojoSort™ Human CD4 Naïve T Cell Isolation Kit (BioLegend, San Diego, CA, USA) according to the manufacturer’s protocol. For isolation, PBS with 0.5% bovine serum
albumin (AppliChem, Darmstadt, Germany), and 2 mM EDTA (Sigma-Aldrich) were used. PBMC STIMULATION PBMC were adjusted to 1 × 106 cells/mL in normal (ZA) or Chelex-treated Zn2+-deficient (ZD)
medium. Cells were stimulated with the indicated concentration of sodium pyrithione and thapsigargin and incubated at 37 °C (both from Sigma-Aldrich). SNOC (generated as described before
[61]) was preincubated for 30 min at 37 °C and then additionally stimulated with thapsigargin. The time of incubation after stimulation is indicated in each figure legend. In general, RNA
was analyzed 3 h and protein expression 48 h after stimulation. When p38 was examined, cells were preincubated at 37 °C for 30 min with 10 µM of the p38 MAPK inhibitor SB202190
(Sigma-Aldrich) or left untreated and subsequently stimulated with pyrithione and thapsigargin and incubated for additional 48 h at 37 °C. LABILE ZN2+ AND CA2+ MEASUREMENTS To measure Zn2+
and Ca2+ signals, respectively, 1–30 min after stimulation 2 × 106 PBMC/mL were first stained with 1 µM FluoZin-3 AM or Fluo-4 for 30 min (both from Invitrogen by Thermo Fisher Scientific,
Eugene, OR, USA). After the staining 1 × 106 cells in 1 mL culture medium were stimulated with the indicated concentrations of pyrithione, thapsigargin (both from Sigma-Aldrich) or SNOC
(generated as described before [61]) and incubated for 10 min or for the indicated time intervals at 37 °C. For Zn2+ measurements, the washed cells were then incubated with 100 µM ZnSO4 and
5 µM sodium pyrithione to induce a maximal fluorescence (_F_max), with 50 µM of the Zn2+ chelator _N_,_N_,_N_,_N_-tetrakis(2-pyridylmethyl)-ethylenediamine (TPEN) to induce a minimal
fluorescence (_F_min) (all from Sigma-Aldrich) or were left untreated (_F_) and incubated for 10 min in a 37 °C water bath. Instead, for Ca2+ measurements cells were incubated with 2 µM
A23187 (Tocris, bio-techne, Wiesbaden-Nordenstadt, Germany) to induce _F_max and with 20 mM EDTA (Sigma-Aldrich) to induce _F_min or were left untreated (_F_). The fluorescent intensity was
measured using the FACSCalibur™ Flow Cytometer (BD Biosciences, San Jose, CA, USA) and analyzed with FlowJo™ Software version 10.8.1 (BD Biosciences). Lymphocytes were gated according to
their size. Labile Zn2+ and Ca2+ were calculated using the equation \(\left[{\rm{Zn}}^{2+}\right]{\rm{or}}[{\rm{Ca}}^{2+}]={K}_{\rm{D}}\times \frac{({F-F}_{\min })}{({F}_{\max }-F)}\) with a
dissociation constant (_K_D) for FluoZin-3 AM (Zn2+) of 8.9 nM and for Fluo-4 (Ca2+) of 335 nM. For measurements of intracellular Zn2+ 48 h after stimulation, 1 × 106 PBMC/mL were first
stimulated as described before and incubated for 48 h at 37 °C. Afterwards, the collected cells were stained with 1 µM FluoZin-3 AM for 30 min, and subsequently _F_min, _F_max and _F_ were
induced in each sample and measured and analyzed by flow cytometry as described above. FLOW CYTOMETRY 1 × 106 cells in PBS + 1% FCS were incubated with the antibodies CD3-FITC (Cat. 345763)
and CD69-APC (Cat. 555533) or the respective isotype controls IgG1, κ-FITC (Cat. 555748) and IgG1, κ-APC (Cat. 555751) (antibodies from BD Biosciences) for 20 min at room temperature in the
dark. Afterwards, cells were washed and measured by flow cytometry using FACSCalibur™ Flow Cytometer (BD Biosciences) and analyzed with FlowJo™ Software version 10.8.1 (BD Biosciences).
Lymphocytes were gated according to their size. ELISA For the quantification of IL-2, IFN-γ, IL-10 and IL-17 the supernatants were collected after 48 h of incubation and stored at −20 °C.
Samples were diluted and IL-2, IFN-γ, IL-10 (all from BD Biosciences) or IL-17 ELISA (R&D Systems, Minneapolis, MN, USA) were performed according to the manufacturer’s protocol. The
detection limits were as follows: 7.8 pg/mL (IL-2); 4.7 pg/mL (IFN-γ); 7.8 pg/mL (IL-10) and 15.6 pg/mL (IL-17). Values below the detection limit were substituted a value just below the
detection limit. Samples were determined in duplicates and absorption was detected using the Spark plate reader (Tecan, Männedorf, Switzerland). QUANTITATIVE REAL-TIME POLYMERASE CHAIN
REACTION (QPCR) 2 × 106 PBMC were lysed in 1 mL TRIzol® Reagent (Ambion/Life Technologies, Darmstadt, Germany) and stored at −80 °C. mRNA was extracted according to the manufacturer’s
protocol and the mRNA concentration was determined by Nanodrop 2000 (Thermo Fisher Scientific, Waltham, MA, USA). cDNA synthesis was performed using the qScriptTM cDNA Synthese Kit
(Quantabio, Beverly, MA, USA) and was diluted 1:2.5 in UV-irradiated H2O. qPCR was performed with PowerSYBR® Green PCR Master Mix (Applied Biosystems by Thermo Fisher Scientific, Woolston,
UK) and 100 nM of the respective forward and reverse primer. The following primer were used: IFN-γ [49], PBGD [49], IRF-1 [47], KLF-10 [47], Zip1-2 [34], Zip3 [62]; Zip4-12 [63], Zip13 [63],
Zip14 [64], ZnT1-9 [65], ZnT10 [34]. The following amplification cycles were used: 1 × 10 min at 95 °C, 40 × 15 s at 95 °C and 60 s at 60 °C, 62 °C (Zip13) or 65 °C (ZnT10). Afterwards, a
melting curve was performed. Data were analyzed by \({2}^{-\Delta \Delta {C}_{T}}\) method [66] and if the mean CT of the PCR product was >35, the corresponding mRNA expression was
excluded as not detectable (n.d.). WESTERN BLOT 2 × 106 cells/sample were resuspended in 100 µL sampling buffer (65 mM Tris-HCl [pH 6.8], 2% SDS, 1 mM Na3VO4, 26% glycerol, 1%
β-mercaptoethanol and 0.01% bromphenol blue), lysed by sonification using Vibra Cell sonicator (Sonics & Materials, Newtown, CT, USA) and heated for 5 min at 95 °C. The sample volume
used was defined by the protein concentration, which was determined by Bio-Rad Protein Assay Dye Reagent Concentrate (Bio-Rad Laboratories, Inc., Hercules, CA, USA). A color prestained
protein standard (New England BioLabs, Frankfurt a.M., Germany) and the samples were run on a 10% polyacrylamide gel at 170 V and blotted onto nitrocellulose membranes at 100 V. Loading of
the gel and protein transfer was confirmed by Ponceau S staining (AppliChem). Membranes were blocked for 1 h in TBS-T (20 mM Tris [pH 7.6],137 mM NaCl and 0.1% Tween-20), containing 5%
fat-free dry milk. Subsequently, membranes were incubated overnight at 4 °C in primary antibodies which were diluted 1:1000 in TBS-T and 5% bovine serum albumin (p38 MAPK (Cat. 9212 S),
phospho-p38 MAPK (Thr180/Tyr182) (Cat. 9215 S), T-bet (Cat. 13232), GATA-3 (Cat. 5852), FoxP3 (Cat. 12632), β-actin (Cat. 4967 S) (all from Cell Signaling Technology, Danvers, MA, USA),
ROR_γ_(t) (Cat. PA5-86733, Invitrogen by Thermo Fisher Scientific)). The secondary antibody HRP-linked anti-rabbit IgG (Cat. 7074, Cell Signaling Technology) was diluted 1:2000 in TBS-T and
5% fat-free dry milk and membranes were incubated at room temperature for 3 h. Band density was determined using Westar Antares (Cyanagen, Bologna, Italy) and LAS-3000 (Fujifilm) and was
analyzed by ImageJ (National Institutes of Health, Bethesda, MD, USA). Original western blots are available as supplementary information. STATISTICAL ANALYSIS Data were statistically
analyzed using GraphPad Prism (version 8.0.1). All data were tested for outliers by the ROUT method, which were removed accordingly, and tested for normality with the Shapiro–Wilk test (_n_
< 8) or with the Anderson–Darling test (_n_ > 8). Accordingly, parametric or non-parametric two-sided tests were used. Sphericity was not assumed and the Geisser–Greenhouse correction
was used. The corresponding tests and the number of sample units are indicated in the figure legends. Different N are PBMC from individual donors whereas experiments were performed with up
to three individual donors on 1 day. Experiments were performed with at least three individual donors. If experiments were significant or clearly not significant, experiments were stopped.
In the case of statistical trends, a simple power analysis was performed and the number of experiments was increased. Data are presented as mean + SEM. When the mean of each column was
compared with the mean of every other column, letters were used to clearly show significant differences. Significantly different results (_p_ < 0.05) have no common identification letter.
For all other tests, significances are indicated as *_p_ < 0.05; **_p_ < 0.01; ***_p_ < 0.001. DATA AVAILABILITY All data generated or analyzed during this study are included in
this published article and detailed data are available from the corresponding author on reasonable request. Original western blots were uploaded as Supplementary Material. REFERENCES *
Smith-Garvin JE, Koretzky GA, Jordan MS. T cell activation. Annu Rev Immunol. 2009;27:591–619. Article CAS PubMed PubMed Central Google Scholar * Skokos D, Shakhar G, Varma R, Waite JC,
Cameron TO, Lindquist RL, et al. Peptide-MHC potency governs dynamic interactions between T cells and dendritic cells in lymph nodes. Nat Immunol. 2007;8:835–44. Article CAS PubMed
Google Scholar * Lewis RS. Calcium signaling mechanisms in T lymphocytes. Annu Rev Immunol. 2001;19:497–521. Article CAS PubMed Google Scholar * Zweifach A, Lewis RS. Mitogen-regulated
Ca2+ current of T lymphocytes is activated by depletion of intracellular Ca2+ stores. Proc Natl Acad Sci USA. 1993;90:6295–9. Article CAS PubMed PubMed Central Google Scholar * Trebak
M, Kinet J-P. Calcium signalling in T cells. Nat Rev Immunol. 2019;19:154–69. Article CAS PubMed PubMed Central Google Scholar * Hennigar SR, Lieberman HR, Fulgoni VL, McClung JP. Serum
zinc concentrations in the US population are related to sex, age, and time of blood draw but not dietary or supplemental zinc. J Nutr. 2018;148:1341–51. Article PubMed Google Scholar *
Colvin RA, Holmes WR, Fontaine CP, Maret W. Cytosolic zinc buffering and muffling: their role in intracellular zinc homeostasis. Metallomics. 2010;2:306–17. Article CAS PubMed Google
Scholar * Singh P, Ali SA. Multifunctional role of S100 protein family in the immune system: an update. Cells. 2022;11:2274. Article CAS PubMed PubMed Central Google Scholar * Yu M,
Lee W-W, Tomar D, Pryshchep S, Czesnikiewicz-Guzik M, Lamar DL, et al. Regulation of T cell receptor signaling by activation-induced zinc influx. J Exp Med. 2011;208:775–85. Article CAS
PubMed PubMed Central Google Scholar * Wessels I, Fischer HJ, Rink L. Dietary and physiological effects of zinc on the immune system. Annu Rev Nutr. 2021;41:133–75. Article CAS PubMed
Google Scholar * Yamasaki S, Sakata-Sogawa K, Hasegawa A, Suzuki T, Kabu K, Sato E, et al. Zinc is a novel intracellular second messenger. J Cell Biol. 2007;177:637–45. Article CAS PubMed
PubMed Central Google Scholar * Lioudyno MI, Kozak JA, Penna A, Safrina O, Zhang SL, Sen D, et al. Orai1 and STIM1 move to the immunological synapse and are up-regulated during T cell
activation. Proc Natl Acad Sci USA. 2008;105:2011–6. Article CAS PubMed PubMed Central Google Scholar * Cahalan MD, Chandy KG. The functional network of ion channels in T lymphocytes.
Immunol Rev. 2009;231:59–87. Article CAS PubMed PubMed Central Google Scholar * Negulescu PA, Krasieva TB, Khan A, Kerschbaum HH, Cahalan MD. Polarity of T cell shape, motility, and
sensitivity to antigen. Immunity. 1996;4:421–30. Article CAS PubMed Google Scholar * Colomar-Carando N, Meseguer A, Company-Garrido I, Jutz S, Herrera-Fernández V, Olvera A, et al. Zip6
transporter is an essential component of the lymphocyte activation machinery. J Immunol. 2019;202:441–50. Article CAS PubMed Google Scholar * Aydemir TB, Liuzzi JP, McClellan S, Cousins
RJ. Zinc transporter ZIP8 (SLC39A8) and zinc influence IFN-gamma expression in activated human T cells. J Leukoc Biol. 2009;86:337–48. Article CAS PubMed PubMed Central Google Scholar *
Uciechowski P, Kahmann L, Plümäkers B, Malavolta M, Mocchegiani E, Dedoussis G, et al. TH1 and TH2 cell polarization increases with aging and is modulated by zinc supplementation. Exp
Gerontol. 2008;43:493–8. Article CAS PubMed Google Scholar * Kahmann L, Uciechowski P, Warmuth S, Malavolta M, Mocchegiani E, Rink L. Effect of improved zinc status on T helper cell
activation and TH1/TH2 ratio in healthy elderly individuals. Biogerontology. 2006;7:429–35. Article CAS PubMed Google Scholar * Rosenkranz E, Metz CHD, Maywald M, Hilgers R-D, Weßels I,
Senff T, et al. Zinc supplementation induces regulatory T cells by inhibition of Sirt-1 deacetylase in mixed lymphocyte cultures. Mol Nutr Food Res. 2016;60:661–71. Article CAS PubMed
Google Scholar * Maywald M, Meurer SK, Weiskirchen R, Rink L. Zinc supplementation augments TGF-β1-dependent regulatory T cell induction. Mol Nutr Food Res. 2017;61:1600493. Article Google
Scholar * Haase H, Ober-Blobaum JL, Engelhardt G, Hebel S, Heit A, Heine H, et al. Zinc signals are essential for lipopolysaccharide-induced signal transduction in monocytes. J Immunol.
2008;181:6491–502. Article CAS PubMed Google Scholar * Treiman M, Caspersen C, Christensen SB. A tool coming of age: thapsigargin as an inhibitor of sarco-endoplasmic reticulum
Ca2+-ATPases. Trends Pharmacol Sci. 1998;19:131–5. Article CAS PubMed Google Scholar * Maywald M, Wessels I, Rink L. Zinc signals and immunity. Int J Mol Sci. 2017;18:1–34. Article
Google Scholar * Schwarz EC, Kummerow C, Wenning AS, Wagner K, Sappok A, Waggershauser K, et al. Calcium dependence of T cell proliferation following focal stimulation. Eur J Immunol.
2007;37:2723–33. Article CAS PubMed Google Scholar * Kaltenberg J, Plum LM, Ober-Blöbaum JL, Hönscheid A, Rink L, Haase H. Zinc signals promote IL-2-dependent proliferation of T cells.
Eur J Immunol. 2010;40:1496–503. Article CAS PubMed Google Scholar * Taylor KM, Hiscox S, Nicholson RI, Hogstrand C, Kille P. Protein kinase CK2 triggers cytosolic zinc signaling
pathways by phosphorylation of zinc channel ZIP7. Sci Signal. 2012;5:ra11. Article PubMed PubMed Central Google Scholar * Berendji D, Kolb-Bachofen V, Meyer KL, Grapenthin O, Weber H,
Wahn V, et al. Nitric oxide mediates intracytoplasmic and intranuclear zinc release. FEBS Lett. 1997;405:37–41. Article CAS PubMed Google Scholar * Kröncke KD, Fehsel K, Schmidt T, Zenke
FT, Dasting I, Wesener JR, et al. Nitric oxide destroys zinc-sulfur clusters inducing zinc release from metallothionein and inhibition of the zinc finger-type yeast transcription activator
LAC9. Biochem Biophys Res Commun. 1994;200:1105–10. Article PubMed Google Scholar * Cibrián D, Sánchez-Madrid F. CD69: from activation marker to metabolic gatekeeper. Eur J Immunol.
2017;47:946–53. Article PubMed PubMed Central Google Scholar * Li C, Beavis P, Palfreeman AC, Amjadi P, Kennedy A, Brennan FM. Activation of p38 mitogen-activated protein kinase is
critical step for acquisition of effector function in cytokine-activated T cells, but acts as a negative regulator in T cells activated through the T-cell receptor. Immunology.
2011;132:104–10. Article CAS PubMed PubMed Central Google Scholar * Dodeller F, Schulze-Koops H. The p38 mitogen-activated protein kinase signaling cascade in CD4 T cells. Arthritis Res
Ther. 2006;8:205. Article PubMed PubMed Central Google Scholar * Hönscheid A, Dubben S, Rink L, Haase H. Zinc differentially regulates mitogen-activated protein kinases in human T
cells. J Nutr Biochem. 2012;23:18–26. Article PubMed Google Scholar * Abbas AK, Trotta E, Simeonov DR, Marson A, Bluestone JA. Revisiting IL-2: biology and therapeutic prospects. Sci
Immunol. 2018;3:eaat1482. Article PubMed Google Scholar * Kloubert V, Wessels I, Wolf J, Blaabjerg K, Janssens V, Hapala J, et al. Zinc deficiency leads to reduced interleukin-2
production by active gene silencing due to enhanced CREMα expression in T cells. Clin Nutr. 2021;40:3263–78. Article CAS PubMed Google Scholar * Baarz BR, Laurentius T, Wolf J, Wessels
I, Bollheimer LC, Rink L. Short-term zinc supplementation of zinc-deficient seniors counteracts CREMα-mediated IL-2 suppression. Immun Ageing. 2022;19:40. Article CAS PubMed PubMed
Central Google Scholar * Prasad AS. Effects of zinc deficiency on Th1 and Th2 cytokine shifts. J Infect Dis. 2000;182:S62–8. Article CAS PubMed Google Scholar * Rosenkranz E, Hilgers
R-D, Uciechowski P, Petersen A, Plümäkers B, Rink L. Zinc enhances the number of regulatory T cells in allergen-stimulated cells from atopic subjects. Eur J Nutr. 2017;56:557–67. Article
CAS PubMed Google Scholar * Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH. A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell. 2000;100:655–69.
Article CAS PubMed Google Scholar * Kano S, Sato K, Morishita Y, Vollstedt S, Kim S, Bishop K, et al. The contribution of transcription factor IRF1 to the interferon-gamma-interleukin 12
signaling axis and TH1 versus TH-17 differentiation of CD4+ T cells. Nat Immunol. 2008;9:34–41. Article CAS PubMed Google Scholar * Unutmaz D, Vilcek J. IRF1: a deus ex machina in TH1
differentiation. Nat Immunol. 2008;9:9–10. Article CAS PubMed Google Scholar * Chatila T, Silverman L, Miller R, Geha R. Mechanisms of T cell activation by the calcium ionophore
ionomycin. J Immunol. 1989;143:1283–9. Article CAS PubMed Google Scholar * Sosa-Peinado A, Fructuoso-García K, Vásquez-Bochm LX, González-Andrade M. Bisindolylmaleimides new ligands of
CaM protein. Molecules. 2022;27:7161. Article CAS PubMed PubMed Central Google Scholar * Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+
regulatory T cells. Nat Immunol. 2003;4:330–6. Article CAS PubMed Google Scholar * Cao Z, Wara AK, Icli B, Sun X, Packard RRS, Esen F, et al. Kruppel-like factor KLF10 targets
transforming growth factor-β1 to regulate CD4+CD25− T cells and T regulatory cells. J Biol Chem. 2009;284:24914–24. Article CAS PubMed PubMed Central Google Scholar * Shiow LR, Rosen
DB, Brdicková N, Xu Y, An J, Lanier LL, et al. CD69 acts downstream of interferon-alpha/beta to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature. 2006;440:540–4. Article CAS
PubMed Google Scholar * Tanaka S, Akaishi E, Hosaka K, Okamura S, Kubohara Y. Zinc ions suppress mitogen-activated interleukin-2 production in Jurkat cells. Biochem Biophys Res Commun.
2005;335:162–7. Article CAS PubMed Google Scholar * Maywald M, Rink L. Zinc supplementation induces CD4+CD25+Foxp3+ antigen-specific regulatory T cells and suppresses IFN-γ production by
upregulation of Foxp3 and KLF-10 and downregulation of IRF-1. Eur J Nutr. 2017;56:1859–69. Article CAS PubMed Google Scholar * Beck FW, Prasad AS, Kaplan J, Fitzgerald JT, Brewer GJ.
Changes in cytokine production and T cell subpopulations in experimentally induced zinc-deficient humans. Am J Physiol. 1997;272:E1002–7. CAS PubMed Google Scholar * Rodenkirchen V,
Schettgen T, Rink L. Zinc deficiency impairs interferon-γ production on post-transcriptional level. J Trace Elem Med Biol. 2020;62:126598. Article CAS PubMed Google Scholar * Huang C, Bi
J. Expression regulation and function of T-Bet in NK cells. Front Immunol. 2021;12:761920. Article CAS PubMed PubMed Central Google Scholar * Jeong J, Eide DJ. The SLC39 family of zinc
transporters. Mol Aspects Med. 2013;34:612–9. Article CAS PubMed PubMed Central Google Scholar * Liu W, Jakobs J, Rink L. Proton-pump inhibitors suppress T cell response by shifting
intracellular zinc distribution. Int J Mol Sci. 2023;24:1191. Article CAS PubMed PubMed Central Google Scholar * Wex T, Grungreiff K, Schutte K, Stengritt M, Reinhold D. Expression
analysis of zinc transporters in resting and stimulated human peripheral blood mononuclear cells. Biomed Rep. 2014;2:217–22. Article CAS PubMed PubMed Central Google Scholar * Guo L,
Urban JF, Zhu J, Paul WE. Elevating calcium in Th2 cells activates multiple pathways to induce IL-4 transcription and mRNA stabilization. J Immunol. 2008;181:3984–93. Article CAS PubMed
Google Scholar * Dong C. Cytokine regulation and function in T cells. Annu Rev Immunol. 2021;39:51–76. Article CAS PubMed Google Scholar * Kaufmann U, Kahlfuss S, Yang J, Ivanova E,
Koralov SB, Feske S. Calcium signaling controls pathogenic Th17 cell-mediated inflammation by regulating mitochondrial function. Cell Metab. 2019;29:1104–1118.e6. Article CAS PubMed
PubMed Central Google Scholar * Kim K-D, Srikanth S, Tan Y-V, Yee M-K, Jew M, Damoiseaux R, et al. Calcium signaling via Orai1 is essential for induction of the nuclear orphan receptor
pathway to drive Th17 differentiation. J Immunol. 2014;192:110–22. Article CAS PubMed Google Scholar * Purvis HA, Stoop JN, Mann J, Woods S, Kozijn AE, Hambleton S, et al. Low-strength
T-cell activation promotes Th17 responses. Blood. 2010;116:4829–37. Article CAS PubMed PubMed Central Google Scholar * Kitabayashi C, Fukada T, Kanamoto M, Ohashi W, Hojyo S, Atsumi T,
et al. Zinc suppresses Th17 development via inhibition of STAT3 activation. Int Immunol. 2010;22:375–86. Article CAS PubMed Google Scholar * George MM, Subramanian Vignesh K, Landero
Figueroa JA, Caruso JA, Deepe GS. Zinc induces dendritic cell tolerogenic phenotype and skews regulatory T cell-Th17 balance. J Immunol. 2016;197:1864–76. Article CAS PubMed Google
Scholar * Barth L-M, Rink L, Wessels I. Increase of the intracellular zinc concentration leads to an activation and internalisation of the epidermal growth factor receptor in A549 cells.
Int J Mol Sci. 2020;22:326. Article PubMed PubMed Central Google Scholar * Dubben S, Hönscheid A, Winkler K, Rink L, Haase H. Cellular zinc homeostasis is a regulator in monocyte
differentiation of HL-60 cells by 1 alpha,25-dihydroxyvitamin D3. J Leukoc Biol. 2010;87:833–44. Article CAS PubMed Google Scholar * Leung KW, Liu M, Xu X, Seiler MJ, Barnstable CJ,
Tombran-Tink J. Expression of ZnT and ZIP zinc transporters in the human RPE and their regulation by neurotrophic factors. Investig Ophthalmol Vis Sci. 2008;49:1221–31. Article Google
Scholar * Ishida T, Takechi S. Nrf2-ARE-dependent alterations in zinc transporter mRNA expression in HepG2 cells. PLoS ONE. 2016;11:e0166100. Article PubMed PubMed Central Google Scholar
* Overbeck S, Uciechowski P, Ackland ML, Ford D, Rink L. Intracellular zinc homeostasis in leukocyte subsets is regulated by different expression of zinc exporters ZnT-1 to ZnT-9. J Leukoc
Biol. 2008;83:368–80. Article CAS PubMed Google Scholar * Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method.
Methods. 2001;25:402–8. Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS We thank Gabriela Engelhardt, Silke Hebel and Laura Dahlmanns for their great experimental
support in final experiments. The graphical abstract was created with BioRender.com. FUNDING Open Access funding enabled and organized by Projekt DEAL. AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * Institute of Immunology, Faculty of Medicine, RWTH Aachen University Hospital, Aachen, Germany Jana Jakobs & Lothar Rink * Institute for Occupational, Social and
Environmental Medicine, Faculty of Medicine, RWTH Aachen University, Aachen, Germany Jens Bertram Authors * Jana Jakobs View author publications You can also search for this author inPubMed
Google Scholar * Jens Bertram View author publications You can also search for this author inPubMed Google Scholar * Lothar Rink View author publications You can also search for this author
inPubMed Google Scholar CONTRIBUTIONS JJ performed the experiments, analyzed and interpreted the data and wrote the manuscript. JB performed the ICP-MS measurements and LR conceived and
supervised the study, and revised the manuscript. All authors have read and approved the final paper. CORRESPONDING AUTHOR Correspondence to Lothar Rink. ETHICS DECLARATIONS COMPETING
INTERESTS The authors declare no competing interests. ETHICS APPROVAL This study was conducted at RWTH Aachen Medical Faculty. The research was performed in accordance with the Declaration
of Helsinki. The protocol and informed consent were reviewed and approved by the RWTH Aachen Medical Faculty Institutional Ethics Committee (EK23-234). INFORMED CONSENT Informed consent was
obtained from all human participants. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional
affiliations. SUPPLEMENTARY INFORMATION COMPLETE SUPPLEMENTARY MATERIAL ORIGINAL DATA RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0
International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the
source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative
Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by
statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Jakobs, J., Bertram, J. & Rink, L. Ca2+ signals are essential for T-cell
proliferation, while Zn2+ signals are necessary for T helper cell 1 differentiation. _Cell Death Discov._ 10, 336 (2024). https://doi.org/10.1038/s41420-024-02104-1 Download citation *
Received: 22 January 2024 * Revised: 11 July 2024 * Accepted: 16 July 2024 * Published: 24 July 2024 * DOI: https://doi.org/10.1038/s41420-024-02104-1 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative
Trending News
Defusing the russia-ukraine crisisCarolyn Kissane, academic director and clinical professor at the Center for Global Affairs at New York University, leads...
Clinical and radiographic evaluation of indirect pulp treatment of young permanent molars using photo-activated oral disinfection versus calcium hydroABSTRACT BACKGROUND Calcium hydroxide is the most commonly used material in indirect pulp treatment (IPT). However, its ...
Affordable and powerful windows 10 laptops – coming soon to indiaCan you get an affordable laptop in the country right now that is worth the price? Most of what we have seen are cheap k...
Prince charles high-fives the kids at caithness schoolCrossroads Primary head teacher Jaccqui Budge said: “The pupils were delighted to meet the Prince and the high-fives wer...
Ladera Ranch News: The Orange County RegisterReal estate news: Warehouse construction begins in AnaheimThe 139,535-square-foot industrial complex is due to wrap up b...
Latests News
Ca2+ signals are essential for t-cell proliferation, while zn2+ signals are necessary for t helper cell 1 differentiationABSTRACT The regulation of T-cell fate is crucial for the balance between infection control and tolerance. Calcium (Ca2+...
Α-synuclein-specific t cell reactivity is associated with preclinical and early parkinson’s diseaseABSTRACT A diagnosis of motor Parkinson’s disease (PD) is preceded by a prolonged premotor phase with accumulating neuro...
Explorations by collette: benefits for aarp membersMemorial Day Sale! Join AARP for just $11 per year with a 5-year membership Join now and get a FREE gift. Expires 6/4 G...
Stricter language rules for french residency cards planned from julyORIGINAL TIMETABLE FOR TIGHTER ‘INTEGRATION’ REQUIREMENTS HAD THEM SET TO BE IMPLEMENTED BY JANUARY 2026 Stricter langua...
Holy cross to award three honorary degrees at commencementHoly Cross will award three honorary degrees to David Wantz, John Nally and Barbara O’Connor at its 55th Commencement on...