A six-participant pilot single-subject study of an individualized pain management program for people with spinal cord injury
A six-participant pilot single-subject study of an individualized pain management program for people with spinal cord injury"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT STUDY DESIGN Single-subject repeated measures design. OBJECTIVES To explore the impacts of a novel individualized interdisciplinary pain self-management program for persons living
with spinal cord injury pain. SETTING A large rehabilitation institute for adults with physical disabilities in Quebec city (Quebec, Canada). METHODS Six persons having sustained a spinal
cord injury and experiencing chronic pain participated. Following a five-week pre-intervention phase (baseline repeated measures) and a clinical evaluation, individualized intervention
objectives were developed in collaboration with each participant. Then, participants completed a ten-week intensive intervention and a six-month consolidation phase. The program included
cognitive behavioral therapy, and physical and pharmacological interventions, which were group- and individual-based. Outcome measures were the Canadian Occupational Performance Measure
(COPM), the French-Canadian Chronic Pain Self-efficacy Scale (FC-CPSES), the Brief Pain Inventory (BPI), and the Hospital Anxiety and Depression Scale (HADS). RESULTS For five out of the six
participants, a majority of outcomes improved during either of the intervention phases or both. Improvements in occupational performance were clinically significant for three participants.
Pain interference and anxiety improved significantly in five participants, while pain self-efficacy and depressive symptoms improved in four participants. CONCLUSIONS The results suggest
that the pain self-management program was effective to reduce the impact of spinal cord injury pain. Further research is needed to replicate these results in a larger study and comprehend
the factors favoring or undermining improvements with such programs, as well as their persistence over time. You have full access to this article via your institution. Download PDF SIMILAR
CONTENT BEING VIEWED BY OTHERS PHYSICAL ACTIVITY INTERVENTIONS, CHRONIC PAIN, AND SUBJECTIVE WELL-BEING AMONG PERSONS WITH SPINAL CORD INJURY: A SYSTEMATIC SCOPING REVIEW Article 18
September 2020 TREATMENTS THAT ARE PERCEIVED TO BE HELPFUL FOR NON-NEUROPATHIC PAIN AFTER TRAUMATIC SPINAL CORD INJURY: A MULTICENTER CROSS-SECTIONAL SURVEY Article 19 March 2021 PRELIMINARY
EXAMINATION OF _COACHING IN CONTEXT_ WITH CLIENTS WITH SPINAL CORD INJURY Article 13 April 2021 INTRODUCTION Among the sequelae which can occur in people living with a SCI, pain is one of
the most common, with a prevalence around 60% [1]. Over half of persons having sustained SCI will develop chronic pain [2]. SCI pain is associated with negative psychosocial consequences,
notably on emotional functions (e.g., stress, depression, anxiety and diminished self-efficacy and wellbeing), as well as economic self-sufficiency [3]. Because SCI pain is often refractory
to curative treatment [2], a few programs targeting _pain management_ for persons living with a SCI have been developed [4,5,6,7,8,9,10,11]. Such pain management programs aim to improve
persons’ function and help them learn to live with pain [12]. Programs’ contents include interventions such as education about pain mechanisms, cognitive and behavioral therapy (CBT)
targeting self-management, exercise and relaxation. While their format varies, most programs offer multidisciplinary group interventions, based on cognitive-behavioral approaches, that
extend over several weeks. Studies have shown positive results for these programs on outcomes including pain intensity and interference with daily life, catastrophizing, self-efficacy,
anxiety, depression, function, social participation and life satisfaction [4, 6,7,8,9, 11]. Maintenance of improvements over time has however shown to be inconsistent across outcomes and
studies. Further focussing on relapse prevention and provision of booster sessions has been suggested for this purpose [4, 7, 8]. The core characteristics of these pain management programs
are in line with the needs expressed by persons living with SCI neuropathic pain in a qualitative study [13]. However, while persons living with SCI related pain need to meet with peers,
this study also revealed that it is important for them to be involved in the treatment plan and that the treatment also be individualized [13]. Thus, the main objective of this pilot study
was to assess the impact of a novel pain self-management program (PSMP) for persons living with chronic SCI pain, inspired by previously conducted programs, but with a specific focus on
individualization, and weaning intervention more gradually in order to help maintain gains over time. The PSMP was tailored to the needs of each participant by involving participants in the
determination of intervention objectives meaningful to them, providing individual sessions alternating with group sessions to work on their own objectives over an extended period of time,
and by using a client-centered primary outcome measure. METHODS STUDY DESIGN A single-subject (A – B) design [14] was used for this pilot study, comprising a five-week pre-intervention phase
(A) and a 36-week intervention phase (B). The intervention phase was further divided into a 10-week intensive phase (B1), followed by a 26-week consolidation phase (B2). Three baseline
measurement points took place during phase A, and seven measurement points during phase B. The detailed sequence of data collection points is presented in Table 1. STUDY SETTING AND
PARTICIPANTS The study took place at the _Institut de réadaptation en déficience physique de Québec_ (_IRDPQ_) of the _Centre intégré universitaire de santé et de services sociaux de la
Capitale-Nationale_, in Quebec, Canada. Participants recruited for the study were the first six patients to participate in this program, as part of its pilot implementation. The target
clientele for the PSMP consisted of 1) adults with traumatic or non-traumatic SCI; 2) living in the community in the territory of Eastern Quebec; and 3) presenting persistent or recurrent
pain having an important impact on the accomplishment of life habits or fulfillment of roles that had been refractory to other treatment approaches for more than six months. The study was
approved by the Research Ethics Committee of the _IRDPQ_ (IRB #2014–397). Each participant provided written informed consent. INTERVENTION The general aim of the PSMP was to make
accomplishment of life roles and habits possible in spite of pain. Program acceptability and feasibility were assessed prior to its implementation by conducting focus groups and interviews
with chronic pain experts and potential users [15]. The team providing the pilot program included a physiatrist, a physical therapist, a physical educator, an occupational therapist, a
psychologist and a clinical coordinator. Following phase A, the PSMP began with a three-week interdisciplinary clinical evaluation carried out for each participant as part of the program.
The results of all the measures and evaluations carried out were used by the clinicians to determine individualized intervention objectives in collaboration with each participant. Ten weeks
of intensive interventions (Phase B1) followed. Two four-hour group-based intervention sessions were provided during weeks 1, 4, 7, and 10. During weeks 2, 3, 5, 6, 8, and 9, interventions
were one-on-one and tailored to the specific needs of each participant. The consolidation phase (B2) consisted of follow-up group-based intervention sessions provided at weeks 16, 24, and
36. During the six-month duration of this phase, the participants could request an appointment with either of the health professionals of the team on a one-on-one basis. The interventions
included CBT, and physical and pharmacological interventions. The CBT sessions were made up of psychoeducation, self-management skills development and training, training for the management
of pain peaks and relapse prevention. Participants were allowed to choose topics beyond the pre-established content. Adapted exercise and relaxation sessions were provided. Participants also
met the physiatrist to adjust their medication. Every week, personal objectives were set by each of the participants along with the health professionals, and they were given homework linked
with their objectives. The detailed content and sequence of the interventions provided during phase B1 is presented in Table 2. DATA COLLECTION Participants’ demographics and clinical data
were drawn from clinical records. As the general aim of the PSMP was to improve the accomplishment of life roles and habits of persons living with SCI pain, the primary outcome in this study
was occupational performance, based on self-identification of functional goals. Pain self-efficacy, pain interference, pain intensity, as well as anxiety and depression symptoms were
secondary outcomes. All these outcomes fall within the most important measurement domains identified for the evaluation of chronic pain self-management programs by Taylor et al. [16].
Occupational performance was assessed through semi-structured interviews conducted by phone by the same evaluator on three occasions: at baseline and at the end of phases B1 and B2.
Secondary outcomes were measured with a single composite questionnaire self-administered online or in paper format, at each of the ten measurement points (see Table 1). STUDY INSTRUMENTS
CANADIAN OCCUPATIONAL PERFORMANCE MEASURE (COPM) Occupational performance was assessed using the French version of the COPM [17]. This outcome measure asks participants to identify five
problems important for them to address in regards to occupational performance, and rate their perceived performance level and satisfaction with performance in each of these problem areas, on
a scale from 1 (_poor_) to 10 (_very good_). The COPM demonstrated good concurrent criterion validity and sensitivity to change, as well as good acceptability for participants in another
study evaluating a chronic pain management program [18]. A 2-point difference in COPM scores is considered a clinically important change [17]. BRIEF PAIN INVENTORY (BPI) A French translation
of the pain interference subscale of the BPI adapted for persons with disabilities, the BPI-I10, was used to measure pain interference [19]. Participants rated the extent to which their
pain interfere with ten activities over the previous seven days on a scale ranging from 0 (_does not interfere_) to 10 (_interferes completely_). The English version of the BPI-I10 was
validated in the SCI population and demonstrated good reliability and convergent validity with other pain-related measures [19, 20]. Likewise, the French version of the original BPI
interference subscale (BPI-I7) showed good internal consistency as well as convergent validity in other populations [21, 22]. FRENCH-CANADIAN CHRONIC PAIN SELF-EFFICACY SCALE (FC-CPSES) Pain
self-efficacy was measured using the FC-CPSES, six-item version. This instrument is an adaptation of the Chronic Disease Self-Efficacy Scale, which measures perceived self-efficacy to
perform self-management behaviors, manage chronic disease in general and achieve outcomes [23]. Participants rated their level of confidence to perform six self-management activities for
pain and related symptoms on a scale from 1 (_not at all_) to 10 (_fully_). The six-item version of the FC-CPSES has been validated in chronic pain patients, demonstrating high internal
consistency, good convergent validity with measures of mental health-related quality of life and pain catastrophizing, as well as good sensitivity to change [23]. HOSPITAL ANXIETY AND
DEPRESSION SCALE (HADS) Anxiety and depression symptoms were measured using a French-Canadian version of the HADS [24]. Participants rated the frequency of anxiety-related symptoms (7
items), and depression-related symptoms (7 items), over the last week on a four-level Likert scale. The HADS has been validated in persons with SCI and both subscales demonstrate good
reliability, as well as good preliminary construct validity [25, 26]. NUMERICAL RATING SCALE TO MEASURE PAIN INTENSITY A French numerical rating scale, “_average pain experienced over the
last seven days_”, was used to measure pain intensity. Participants rated the intensity of their pain on a scale from 0 (_no pain_) to 10 (_worst possible pain_). Numerical rating scales for
measuring pain intensity demonstrate good validity and sensitivity to change among different populations and are recommended for use in studies of pain after SCI [19]. DATA ANALYSIS
Participants’ characteristics were synthesized using descriptive statistics. For all outcomes, data were analysed graphically for each participant at each measurement point. For all
secondary outcomes, means and standard deviations were computed for scores measured at baseline for each participant. Scores obtained during phases B1 and B2 were then compared visually to
the baseline mean. Two consecutive scores needed to be two standard deviations above or below the baseline mean for change to be considered significant [14]. In some cases, the standard
deviation for baseline scores was zero, because of missing data or because of consistency in scores between measurement points. In such cases, the zero standard deviation was replaced by
that of the other participant whose baseline mean for the same outcome was closest to the single measured value for that participant. RESULTS The six persons who took part in the pilot PSMP
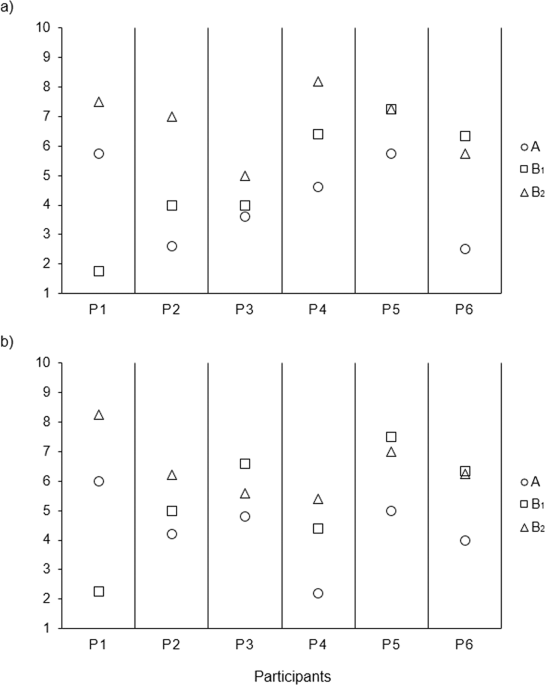
agreed to participate in the study. Characteristics of the participants are presented in Table 3. OCCUPATIONAL PERFORMANCE Occupational performance and satisfaction with performance scores
improved for five participants (P2, P3, P4, P5, and P6) at the end of phase B1 compared to baseline. These improvements were clinically significant in one participant for performance (P6),
and in three participants for satisfaction (P4, P5, and P6). At the end of phase B2, both occupational performance and satisfaction with performance were improved in all participants. These
improvements were clinically significant in three participants for performance (P2, P4, and P6), and in five participants for satisfaction (P1, P2, P4, P5, and P6). These results are
displayed in Fig. 1. PAIN INTERFERENCE There was a significant decrease in pain interference with intervention for five participants (P2, P3, P4, P5, and P6) (see Fig. 2). For three of them
(P3, P4, and P5), the decrease occurred during phase B1, and it was maintained over phase B2 for participant 4. For participants 2 and 6, the significant decrease occurred only during phase
B2. For participant 1, pain interference remained relatively stable over the three phases of the study. PAIN SELF-EFFICACY Significant improvements in pain self-efficacy occurred during
phase B1 in four participants (P1, P3, P5, and P6) (see Fig. 3). For two of them (P3 and P6), the improvement was maintained over phase B2. For the other two participants (P1 and P5), the
level of pain self-efficacy fluctuated over the two phases of the intervention. For participants 2 and 4, there was a trend towards an increase in pain self-efficacy, but the improvement was
not significant. ANXIETY AND DEPRESSION SYMPTOMS The results for anxiety and depression symptoms are displayed in Figs. 4, 5, respectively. Anxiety decreased significantly with intervention
in five participants (P1, P2, P4, P5, and P6). The decrease occurred during phase B1 in three of them (P4, P5, and P6) and was maintained over phase B2 in participant 6. Depressive symptoms
decreased significantly with intervention in four participants (P2, P3, P5, and P6). For participant 6, the decrease occurred during phase B1 and was maintained over phase B2. Depression
scores followed quite variable patterns over phases B1 and B2 in the other three participants (P2, P3, and P5). For participant 4, there was a trend towards a decrease in depression-related
symptoms with intervention, but the improvement was not significant. PAIN INTENSITY The results for pain intensity are displayed in Fig. 6. There was a significant decrease in pain intensity
with intervention in one participant (P4), which occurred during phase B2. For the other five participants, there was either no significant change in pain intensity with intervention (P1,
P2, and P6), or a significant increase (P3 and P5). DISCUSSION This pilot study used a single-subject design to assess the effects of an interdisciplinary PSMP for persons living with SCI
and chronic pain. The PSMP was innovative in that it was tailored to the needs of participants, with individualized objectives for each of them. Visual analysis of data revealed either
significant improvement or a tendency towards improvement with intervention in all of the outcomes measured for a majority of participants, except pain intensity. For occupational
performance, the scores improved during both intervention phases in a majority of participants. This may reflect the fact that the tool used to measure this outcome, the COPM, is tailored to
the personal goals of the participants [17]. Participants were perhaps especially motivated to improve their performance in the areas they chose themselves. For satisfaction with
occupational performance, pain interference, pain self-efficacy and anxiety and depression symptoms, scores did not follow such a clear trend over time across participants, but rather tended
to return to baseline levels during the consolidation phase in some of them. Visual analysis of each participant’s data individually also reveals that the improvement or trend towards
improvement across outcomes was more consistent in some participants. In some cases, for a given participant, scores fluctuated across outcomes during the course of the intervention, or even
markedly worsened at some point. These variations may perhaps be explained by events in the life of the participants related to their SCI condition. Indeed, events such as urinary tract
infections, pressure sores or upper limb joints overuse are secondary health conditions commonly reported in people living with SCI [27] that can impact on outcomes such as pain, distress or
functioning. To our knowledge, our study is the first to have assessed occupational performance, especially using a client-centered primary outcome measure. Previous studies found
improvements in related outcomes such as pain-related disability [6, 7, 9] and participation in activities [6]. We also found improvements in pain interference, which is in line with other
similar studies [4, 8]. Improvements were found as well in other studies on pain self-efficacy [8, 9], and anxiety [6, 8, 9, 11] and depressive symptoms [9, 11]. However, some studies found
no significant change with intervention for this latter outcome [6,7,8]. In the present study, depressive symptoms are the outcome for which there was the greatest variability in scores
across participants. Finally, for pain intensity, the absence of change we found was not surprising as pain reduction was not the primary objective of the PSMP. We nonetheless measured this
outcome because it is important for people living with SCI and some studies on pain management programs in this population showed reductions in pain intensity reaching or approaching
significance [6,7,8,9]. Long term effects of pain management programs are a crucial issue. In their study, Burns et al. [4] suggested to pursue interventions with a “periodic booster” after
the end of the intensive program to help maintain improvements, because their outcomes tended to return to baseline levels after the end of the program. For the same reason, Nicholson Perry
et al. [8] suggested to further insist on relapse prevention in such programs. Both booster interventions and relapse prevention were integrated within the PSMP. To our knowledge, our study
is the first to have included a consolidation phase comprising periodic booster interventions provided over an extended period of time. The only study we have found which offered some
intervention following its intensive phase provided a single comeback session three weeks after the end of a ten-week weekly intervention [5]. Our results indicate that the progressive
weaning of the intervention and the relapse prevention may have been effective, as outcomes continued to improve or at least were maintained during the consolidation phase in many cases.
This study had certain limitations. First, as we conducted a pilot study, our results are based on a small sample of individuals with SCI and pain who were their own controls. Although the
study design does not allow making generalizations, it permitted to detect variability in results within and between participants. Second, additional measurement points prior to the
beginning of the PSMP would have permitted to better characterize the baseline level and the normal degree of variability for each participant on each of the outcome measures. Moreover, some
data at baseline were missing. Results in those cases should be interpreted with caution. In conclusion, our results are in line with those of the few other existing studies that assessed
the effects of a multidisciplinary pain self-management program for persons living with SCI. Findings suggest that the pain self-management program could be effective in improving pain
interference in daily life, pain self-efficacy, as well as mood in people living with SCI and chronic pain. The fact that occupational performance, which was measured with a client-centered
instrument, was the sole outcome that further improved during the consolidation phase in a majority of participants, suggests that tailoring the program to the individual needs of each
participant is useful. Further research is needed to replicate these results in a larger study and comprehend the factors favoring or undermining improvements with such programs, as well as
their persistence over time. DATA AVAILABILITY The datasets generated and analyzed during the current study could be made available from the corresponding author on reasonable request.
REFERENCES * van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015;19:5–14. Article
Google Scholar * Mehta S, Teasell RW, Loh E, Short C, Wolfe DL, Benton B, et al. Pain following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et
al. (eds). Spinal Cord Injury Rehabilitation Evidence. Version 7.0. 2019. pp. 1–105. * Tran J, Dorstyn DS, Burke AL. Psychosocial aspects of spinal cord injury pain: a meta-analysis. Spinal
Cord. 2016;54:640–8. Article CAS Google Scholar * Burns AS, Delparte JJ, Ballantyne EC, Boschen KA. Evaluation of an interdisciplinary program for chronic pain after spinal cord injury.
PM R 2013;5:832–8. Article Google Scholar * Heutink M, Post MW, Luthart P, Pfennings LE, Dijkstra CA, Lindeman E. A multidisciplinary cognitive behavioural programme for coping with
chronic neuropathic pain following spinal cord injury: the protocol of the CONECSI trial. BMC Neurol [Internet]. 2010;10:96. * Heutink M, Post MW, Bongers-Janssen HM, Dijkstra CA, Snoek GJ,
Spijkerman DC, et al. The CONECSI trial: Results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal
cord injury. Pain 2012;153:120–8. Article Google Scholar * Heutink M, Post MW, Luthart P, Schuitemaker M, Slangen S, Sweers J, et al. Long-term outcomes of a multidisciplinary cognitive
behavioural programme for coping with chronic neuropathic spinal cord injury pain. J Rehabil Med. 2014;46:540–5. Article Google Scholar * Nicholson Perry K, Nicholas MK, Middleton JW.
Comparison of a pain management program with usual care in a pain management center for people with spinal cord injury-related chronic pain. Clin J Pain. 2010;26:206–16. Article Google
Scholar * Dear BF, Nicholson Perry K, Siddall P, Middleton JW, Johnson J, Katte L, et al. The Pain Course: Exploring the feasibility of an internet-delivered pain management programme for
adults with spinal cord injury. Spinal Cord. 2018;56:931–9. Article CAS Google Scholar * Dear BF, Titov N, Perry KN, Johnston L, Wootton BM, Terides MD, et al. The Pain Course: a
randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain 2013;154:942–50. Article
Google Scholar * Norrbrink Budh C, Kowalski J, Lundeberg T. A comprehensive pain management programme comprising educational, cognitive and behavioural interventions for neuropathic pain
following spinal cord injury. J Rehabil Med. 2006;38:172–80. Article Google Scholar * Flor H, Turk DC. Chronic pain: an integrated biobehavioral approach. IASP Press, Seattle; 2011. *
Norrbrink C, Lofgren M. Needs and requests - patients and physicians voices about improving the management of spinal cord injury neuropathic pain. Disabil Rehabil. 2016;38:151–8. Article
Google Scholar * Portney LG. Foundations of clinical research: applications to evidence-based practice. Fourth ed. F.A. Davis Company, Philadelphia; 2020. * Quirion R. Développement d’un
programme d’autogestion de la douleur chronique pour les personnes vivant avec une lésion médullaire [master’s essay]. Université de Sherbrooke, Sherbrooke; 2014. * Taylor SJC, Carnes D,
Homer K, Pincus T, Kahan BC, Hounsome N, et al. Improving the self-management of chronic pain: COping with persistent Pain, Effectiveness Research in Self-management (COPERS). NIHR Journals
Library, Southampton; 2016. * Law M, Baptiste S, Carswell A, McColl MA, Polatajko H, Pollock N. La mesure canadienne du rendement occupationnel. Fifth ed. CAOT Publications ACE, Ottawa;
2014. * Carpenter L, Baker GA, Tyldesley B. The use of the Canadian Occupational Performance Measure as an outcome of a pain management program. Can J Occup Ther. 2001;68:16–22. Article CAS
Google Scholar * Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB, et al. Pain after spinal cord injury: an evidence-based review for clinical practice and research.
Report of the National Institute on Disability and Rehabilitation Research Spinal Cord Injury Measures meeting. J Spinal Cord Med. 2007;30:421–40. Article Google Scholar * Raichle KA,
Osborne TL, Jensen MP, Cardenas D. The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain. 2006;7:179–86. Article Google Scholar * Serlin RC,
Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995;61:277–84. Article Google
Scholar * Poundja J, Fikretoglu D, Guay S, Brunet A. Validation of the French version of the Brief Pain Inventory in Canadian veterans suffering from traumatic stress. J Pain Symptom Manag.
2007;33:720–6. Article Google Scholar * Lacasse A, Bourgault P, Tousignant-Laflamme Y, Courtemanche-Harel R, Choiniere M. Development and validation of the French-Canadian Chronic Pain
Self-efficacy Scale. Pain Res Manag. 2015;20:75–83. Article Google Scholar * Savard J, Laberge B, Gauthier JG, Ivers H, Bergeron MG. Evaluating anxiety and depression in HIV-infected
patients. J Pers Assess. 1998;71:349–67. Article CAS Google Scholar * Woolrich RA, Kennedy P, Tasiemski T. A preliminary psychometric evaluation of the Hospital Anxiety and Depression
Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med. 2006;11:80–90. Article Google Scholar * Muller R, Cieza A, Geyh S. Rasch analysis of the Hospital Anxiety
and Depression Scale in spinal cord injury. Rehabil Psychol. 2012;57:214–23. * Noreau L, Proulx P, Gagnon L, Drolet M, Laramee MT. Secondary impairments after spinal cord injury: a
population-based study. Am J Phys Med Rehabil. 2000;79:526–35. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS The authors wish to thank all the stakeholders involved in
the pain self-management program studied (managers, professionals and users), as well as Chantal Dufour for her help with documentary research. FUNDING This work was supported by funds
granted to KPe by the _Fonds de recherche du Québec – Santé_, through her Junior 1 Research Scholar grant; and start-up funds from the _Centre interdisciplinaire de recherche en réadaptation
et intégration sociale_. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Centre interdisciplinaire de recherche en réadaptation et intégration sociale, Centre intégré universitaire de santé
et de services sociaux de la Capitale-Nationale, Quebec city, Quebec, Canada Ketsia Proulx, Marie-Eve Lamontagne, René Quirion, Catherine Mercier & Kadija Perreault * Département de
réadaptation, Faculté de médecine, Université Laval, Quebec city, Quebec, Canada Marie-Eve Lamontagne, René Quirion, Catherine Mercier & Kadija Perreault * Institut de réadaptation en
déficience physique de Québec, Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale, Quebec city, Quebec, Canada René Quirion & Isabelle Deaudelin
Authors * Ketsia Proulx View author publications You can also search for this author inPubMed Google Scholar * Marie-Eve Lamontagne View author publications You can also search for this
author inPubMed Google Scholar * René Quirion View author publications You can also search for this author inPubMed Google Scholar * Isabelle Deaudelin View author publications You can also
search for this author inPubMed Google Scholar * Catherine Mercier View author publications You can also search for this author inPubMed Google Scholar * Kadija Perreault View author
publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS MEL and RQ initiated and designed the study. The protocol was drafted by MEL, RQ, ID, KPe, and CM. Data
were collected by RQ, ID and KPe. KPr and KPe analysed and interpreted the data. The manuscript was drafted by KPr and KPe. All authors critically revised the manuscript and they have
accepted responsibility for its entire content and approved its submission. CORRESPONDING AUTHOR Correspondence to Kadija Perreault. ETHICS DECLARATIONS COMPETING INTERESTS The authors
declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other
rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Proulx, K., Lamontagne, ME., Quirion, R. _et al._ A six-participant pilot single-subject study of an individualized pain management program
for people with spinal cord injury. _Spinal Cord Ser Cases_ 9, 2 (2023). https://doi.org/10.1038/s41394-022-00557-z Download citation * Received: 21 March 2022 * Revised: 18 December 2022 *
Accepted: 29 December 2022 * Published: 16 January 2023 * DOI: https://doi.org/10.1038/s41394-022-00557-z SHARE THIS ARTICLE Anyone you share the following link with will be able to read
this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Javascript support required...
Paris olympics 2024: stylistic change behind india's hockey gloryThat has, inarguably contributed to consecutive bronze medals, a first for the side since 1972. Conceding 12 goals over ...
Submitting a form to different action methods in asp. Net mvcThere are different ways to indicate the action method, that we want to submit our form to. I am going to explain these ...
Jagan mohan reddy’s ysrcp sweeps andhra’s municipal body pollsThe YSR Congress Party (YSRCP) on Sunday, 14 March had a sweeping victory in urban body elections in Andhra Pradesh, win...
"Growing rich is hard, staying rich is harder," says Rahul Jain of Nuvama WealthWe preserve what we value. Life is a chief example of this. More so, we take extra care if what we value is earned by us...
Latests News
A six-participant pilot single-subject study of an individualized pain management program for people with spinal cord injuryABSTRACT STUDY DESIGN Single-subject repeated measures design. OBJECTIVES To explore the impacts of a novel individualiz...
Correction: corrigendum: production of ins(1,3,4,5)p4 mediated by the kinase itpkb inhibits store-operated calcium channels and regulates b cell selec_Nat. Immunol._ 8, 514–521 (2007); published online: 8 April 2007; corrected after print 24 May 2007 In the version of t...
Influence of antihypertensive therapy and blood pressure control on left ventricular geometry and function in subjects with type ii diabetes: the augsABSTRACT Cross-sectional data often fail to show beneficial effects of antihypertensive therapy in patients with hyperte...
Phase separation of eb1 guides microtubule plus-end dynamicsABSTRACT In eukaryotes, end-binding (EB) proteins serve as a hub for orchestrating microtubule dynamics and are essentia...
Applying genomic resources to accelerate wheat biofortificationABSTRACT Wheat has low levels of the micronutrients iron and zinc in the grain, which contributes to 2 billion people su...