Expert consensus on the prevention and treatment of enamel demineralization in orthodontic treatment
Expert consensus on the prevention and treatment of enamel demineralization in orthodontic treatment"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACTS Enamel demineralization, the formation of white spot lesions, is a common issue in clinical orthodontic treatment. The appearance of white spot lesions not only affects the texture
and health of dental hard tissues but also impacts the health and aesthetics of teeth after orthodontic treatment. The prevention, diagnosis, and treatment of white spot lesions that occur
throughout the orthodontic treatment process involve multiple dental specialties. This expert consensus will focus on providing guiding opinions on the management and prevention of white
spot lesions during orthodontic treatment, advocating for proactive prevention, early detection, timely treatment, scientific follow-up, and multidisciplinary management of white spot
lesions throughout the orthodontic process, thereby maintaining the dental health of patients during orthodontic treatment. SIMILAR CONTENT BEING VIEWED BY OTHERS DIAGNOSIS AND TREATMENT
OPTIONS FOR ANTERIOR WHITE SPOT LESIONS Article 25 September 2020 WHITE ENAMEL LESIONS IN CHILDREN: CONSIDERING CARIES, CHRONOLOGICAL AND CONGENITAL CAUSES AND THEIR CONSEQUENT CARE Article
23 April 2021 EXPERT CONSENSUS ON THE DIAGNOSIS AND THERAPY OF ENDO-PERIODONTAL LESIONS Article Open access 01 September 2024 INTRODUCTION The treatment course for correcting dental and
maxillofacial deformities usually lasts 2 to 3 years. If treatment is started after the deciduous dentition period, it may extend even longer, possibly up to 7 to 10 years.1,2 During this
period, poor maintenance of oral hygiene and a lack of health education and management can lead to a demineralization-remineralization imbalance of the hard dental tissues around orthodontic
appliances and gingival margins. Mineral loss beneath the relatively intact enamel surface causes an increase in surface porosity, resulting in decreased translucency and loss of gloss,
resulting in white spot lesions (WSL) on the enamel surface.3 WSL is softer in texture than adjacent healthy enamel, appearing chalky white when dry. Some patients may experience decreased
satisfaction due to the aesthetic effect of white spots on the enamel surface after orthodontic appliances removal. As WSL progresses, surface enamel collapses and caries form. In severe
cases, pulp tissue may invade, causing pulpitis, which requires root canal treatment or even extraction of the affected tooth.4,5,6,7 Therefore, the prevention, early diagnosis, and
treatment of WSL during orthodontic treatment are highly important for maintaining oral health and enhancing aesthetics and patient satisfaction after orthodontic treatment.8 The prevalence
of WSL ranges from 23.4% to 75.6%, depending on the detection methods and research purposes. Patients wearing clear aligners have a lower incidence of WSL than those receiving treatment with
fixed appliances.9,10 The severity of WSL in males was greater than that in females, although the incidence of WSL was not significantly different according to sex. In orthodontic cases,
WSL affects 23.4% of anterior teeth, with a greater incidence of maxillary anterior teeth than mandibular anterior teeth. Additionally, the WSL in patients wearing clear aligners appear
larger but shallower, while those in fixed appliance patients tend to be smaller but deeper.11 Risk factors for WSL include dental fluorosis, orthodontic treatment for more than 36 months,
poor oral hygiene before treatment, deterioration of oral hygiene during orthodontic treatment, and preexisting WSL. The most significant risk factor is the presence of preexisting WSL,
followed by deterioration of oral hygiene during treatment and poor oral hygiene before treatment.12,13,14 Studies have shown that fixed orthodontic appliances are difficult to clean in the
oral cavity, leading to increased plaque accumulation, which lowers the pH around them and increases the risk of caries.15,16 Studies also report that the composition of the dental plaque
biofilm microflora changes after wearing orthodontic appliances, with significantly elevated levels of acidogenic bacteria, including mutans streptococci. These bacteria, when provided with
sufficient carbohydrates, produce acidic byproducts, further lowering the plaque pH below the remineralization threshold and disrupting the mineralization-remineralization balance, leading
to demineralization of dental hard tissues and ultimately causing WSL over time.17,18 The main clinical treatment methods for WSL involve reducing enamel demineralization, promoting
remineralization, and aesthetically restoring demineralized enamel. Fluoride is a commonly used preventive agent for WSL. It forms fluoroapatite and fluorohydroxyapatite by binding with
calcium and phosphate in the enamel. As shown in Table 1, these substances have higher solubility products than hydroxyapatite, making them more resistant to acid dissolution, thus enhancing
the acid resistance of teeth to reduce enamel demineralization. However, fluoride application must be within the nationally regulated safe dosage limits, as excessive use can cause
fluorosis. Remineralizing agents such as casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) work by promoting the repair of microlesions on the enamel surface, allowing calcium and
phosphate ions to redeposit on the enamel, restoring its structure, and inhibiting WSL progression. However, their efficacy in severe cases is limited. Aesthetic restoration of teeth
affected by WSL, which involves removing a certain amount of superficial enamel, is considered the best approach for restoring dental configuration.19,20 Various limitations exist in the
treatment of severe WSL patients, emphasizing the importance of timely detection of WSL during orthodontic treatment and intervention with appropriate treatment methods. This article
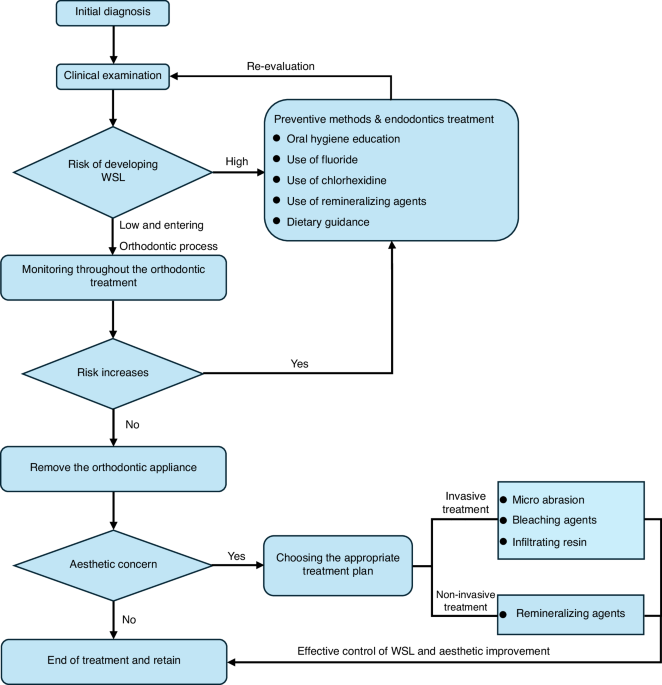
provides guidance on the management and treatment of WSL in orthodontic cases. The recommended clinical procedure is shown in Fig. 1. At the initial visit, the patient’s risk of dental
demineralization should be assessed through clinical examination and medical history inquiry. If evaluated as high risk, preventive methods should be implemented, and a referral to
endodontics is recommended. Orthodontic treatment should only commence if the patient is assessed as low-risk. During orthodontic treatment, the risk of dental demineralization should be
evaluated at each follow-up visit, with timely preventive methods and referrals to endodontics as needed until the risk is reduced. After the removal of orthodontic appliances, appropriate
invasive or non-invasive treatment measures should be selected for teeth with aesthetic concerns to achieve satisfactory outcomes for the patient. The following sections will detail the key
points of each stage. DIAGNOSIS OF ENAMEL DEMINERALIZATION Gorelick et al. proposed a scoring system based on the severity of WSL, and Fig. 2 shows the scoring criteria and the intraoral
photographs of the appearance of WSLs in the progress of orthodontic treatment.12 There are various kinds of clinical examination methods for WSL. The most used methods include visual
examination and digital photo evaluation. In recent years, technologies such as fluorescence, electrical resistance testing, light-conducting fiber transillumination, and near-infrared
transillumination have gradually been applied in the clinical diagnosis of WSL.21,22 ORAL EXAMINATION The most commonly used method for diagnosing WSL is visual examination.23 By combining
visual examination with probing, it can be determined whether the WSL is in a stable period. A rough and chalky enamel surface indicates active demineralization, while a smooth and glossy
enamel surface indicates a balance between demineralization and remineralization, with no further development.24 The refractive index of healthy enamel for light is 1.62, indicating
semitransparency. However, the refractive index of demineralized enamel increases due to increased porosity, resulting in a chalky appearance. When the surface of demineralized enamel is
moist, water fills the tiny gaps. As the refractive index of water is close to that of healthy enamel (1.33), the chalky appearance of demineralized enamel is difficult to observe. Dry
demineralized enamel, on the other hand, filled with air with a refractive index of 1.0 in its tiny gaps, exhibits a noticeable chalky appearance.25 Therefore, for accurate visual
examination, the tooth surface needs to be cleaned, dried for at least 5 seconds, and examined with the assistance of a mouth mirror and bright light. Visual examination has the advantages
of simplicity and cost-effectiveness, without the need for additional equipment. However, this method has disadvantages such as subjectivity in examination, low repeatability, and difficulty
in accurately diagnosing advanced lesions.26 DIGITAL PHOTO EVALUATION A simple visual examination cannot provide patient records. Oral photographs taken with a digital camera can store data
on dental lesions for consultation among orthodontists, prosthodontists, endodontists, and preventive dentistry departments, facilitating remote discussions on shared examination results.
Before taking photographs, it is necessary to carefully clean the tooth surface to remove plaque, dry the tooth surface and maintain an appropriate distance between the camera and the target
tooth. It is recommended to use horizontal dual flash or ring flash and a camera with interchangeable macro lenses. After obtaining high-definition images, the tooth WSL value was
calculated by defining regions of interest (ROIs) on the tooth surface and analyzing the grayscale values.27 Digital photos can store patient data for a long time with greater repeatability,
but they have drawbacks such as technical sensitivity and a high cost of equipment.28 FLUORESCENCE TECHNOLOGY When teeth are exposed to light of specific wavelengths, fluorescence is
produced. The fluorescence intensity varies among enamel, dentin, and cementum.29 Because dentin contains more organic material, its intrinsic fluorescence intensity is greater than that of
enamel. After demineralization, the intrinsic fluorescence of the enamel decreases, and these optical changes are directly related to the mineral content of the enamel. Therefore, utilizing
the spontaneous fluorescence characteristics of teeth for diagnosing demineralization has several applications. Quantitative light-induced fluorescence (QLF) is a technique that utilizes
this fluorescence principle. The tooth surface was irradiated with near-ultraviolet light, and the generated fluorescence image was analyzed using specific software to display the size and
density of demineralized enamel lesions.30 Some laser devices emit red light at wavelengths of 638-655 nm to diagnose demineralization of tooth tissue by inducing infrared fluorescence after
irradiation. The fluorescence intensity increases with the severity of demineralization, but its precision is insufficient to measure tiny variations in mineral content.31 To enhance
diagnostic sensitivity, a dye-enhanced laser fluorescence (DELF) technique has been developed. It involves staining demineralized tissues with a fluorescence dye that penetrates and enhances
the fluorescence generated by the laser by combining with a fluorescence dye spectrum close to the wavelength of the DIAGNOdent laser.32,33 However, fluorescence technology also has
significant drawbacks. Factors such as tooth staining, prosthesis, and other restorative materials can affect the fluorescence signal, leading to false-positive or false-negative results.34
Research has shown that the effectiveness of the fluorescence detection device DIAGNOdent Pen is comparable to that of conventional visual inspection. In recent years, various devices based
on fluorescence technology have been developed, such as DIAGNOdent (KaVo, Germany), MidWest (DENTSPLY, USA), VistaProof (Durr Dental, Germany) and others.35 Although various fluorescence
methods for caries detection devices are currently used in clinical practice as auxiliary diagnostic tools for caries detection, they cannot yet be considered the gold standard for detecting
dental caries.36 FIBER-OPTIC TRANSILLUMINATION—DIGITAL IMAGING FIBER-OPTIC TRANSILLUMINATION (FOTI-DIFOTI) The light transmission coefficient of demineralized dental tissue differs from
that of healthy dental tissue. Demineralization disrupts the dense hydroxyapatite in dental tissue, causing light to scatter as it passes through the highly porous demineralized tissue,
resulting in optical distortion. Since the light transmission coefficient of intact enamel is greater than that of carious lesions, shadows can be seen when examining demineralized dental
tissue with a fiber optic device.37 By evaluating the shadow intensity formed by the device’s light, demineralized dental tissue can be distinguished. Near-infrared light transillumination
(NILT) uses longer wavelengths of invisible near-infrared light to reduce light scattering within dental tissue, allowing better penetration of dental tissue.38,39 As a result, this method
can provide high contrast between healthy tissue and demineralized lesion tissue. A recent study showed that this diagnostic method can more accurately detect early demineralization of
dental enamel and dentin hidden in dental tissue than other methods.40 The principle of light transmission through optical fibers is the scattering and absorption of light on the surface of
enamel and dentin, stains, pigments, etc., on the surface of teeth, which may cause false positives. Fillings, prostheses, etc., can also cause the corresponding areas to be undetectable.41
In recent years, fiber optic transillumination technology has been widely used clinically to detect smooth surface caries, proximal caries, secondary caries, dental fluorosis, incomplete
fracture, etc.42 ELECTRICAL RESISTANCE MEASUREMENTS Electrical resistance measurement devices for dental hard tissues use fixed-frequency AC to measure their resistance.43 The magnitude of
the resistance depends on the porosity of the measured tooth area, the amount of liquid in the porous areas, the temperature, the flow of liquid, and the ion concentration in the porous
areas. It has been reported that the accuracy of resistance measurements in demineralized dental tissues on sound surfaces is greater than that on occlusal surfaces.44,45,46 In the early
stages of lesions, the sensitivity of electrical resistance measurement is superior to that of fiber optic transillumination, but its repeatability is poor, with some clinical limitations
and less clinical application. OPTICAL COHERENCE TOMOGRAPHY In addition to the methods mentioned above, in recent years, swept-source optical coherence tomography (SS-OCT) has been
increasingly utilized in dentistry. SS-OCT works by directing weak, coherent light onto the tooth surface. As demineralization of enamel occurs, organic components increase, leading to a
decrease in the light scattering coefficient compared to surrounding healthy tissue. This reduces light intensity, presenting as a high-gray image compared to the surrounding healthy area,
enabling the detection and analysis of early enamel caries.47 Studies have reported that SS-OCT can effectively assess the depth of WSL and has been applied in clinical practice.48
ARTIFICIAL INTELLIGENCE (AI) With the advancement of artificial intelligence technology, deep learning has made significant progress in dentistry. Convolutional neural networks (CNNs) based
on deep learning have been widely used in cervical vertebral maturation staging, automatic landmarking of lateral cephalograms, and caries diagnosis due to their advantages in processing
large images. Research has shown that using CNNs for segmenting digital dental surface photos and digital fiberoptic transillumination images can achieve an automatic caries detection
accuracy of up to 95%.49 AI models have shown excellent diagnostic performance in caries detection and may become an important auxiliary tool in clinical practice. Future research needs to
rely on comparable, large, and clinically significant datasets. OTHER METHODS In recent years, high-frequency ultrasound (HFUS) for measuring enamel demineralization and photothermal
radiometry (PTR) have also been explored for the clinical detection of enamel demineralization. However, further research is needed to develop these detection methods.50,51 The International
Caries Detection and Assessment System (ICDAS) 2004 consensus workshop concluded that visual examination and probing remain the standards for caries diagnosis.23 Currently, there are a
variety of methods used for demineralization detection, serving as auxiliary tools for clinical decision-making, enhancing diagnostic accuracy, and monitoring disease progression.52 CLINICAL
RECOMMENDATIONS FOR THE DIAGNOSIS OF ENAMEL DEMINERALIZATION * The preferred method for examining the demineralization of tooth surfaces is through a combination of visual and probing
examination, which can be supplemented by using a digital camera and a macro lens to record the demineralized tooth surfaces. It is important to ensure sufficient light but avoid
overexposure when taking photos with a digital camera to prevent false-negatives. * During the examination of tooth surfaces, it is important to thoroughly clean and dry the surfaces and
observe them under bright light to detect any changes in the appearance of white chalkiness. * A probe was used to examine the roughness of the tooth surfaces when conducting the examination
and to assess whether demineralization was in an active stage. * For quantitative analysis of white chalky changes on tooth surfaces, supplementary methods such as fluorescence technology,
fiber optic transillumination, and resistance testing should be used. The use of artificial intelligence for interpreting tooth demineralization has a promising application in assisting
chair-side examinations. RISK ASSESSMENT OF ENAMEL DEMINERALIZATION BEFORE ORTHODONTIC TREATMENT The orthodontic appliances used during treatment may increase the area of plaque attachment,
making it difficult to clean the appliance and the surrounding tooth surfaces. The irregular surfaces of brackets, archwires, and bands may limit the movement of oral muscles and the natural
self-cleaning action of salivary glands, which makes plaque formation easier.53 WSL are early signs of dental caries, with contributing factors including the host, bacteria, food, and time.
Reducing plaque formation and decreasing the consumption of cariogenic foods are primary strategies for minimizing WSL development. WSL is a significant factor that compromises oral health
and aesthetics throughout orthodontic treatment. Therefore, risk assessment and oral health education before orthodontic treatment play a vital role in reducing the occurrence of WSL.54,55
Risk assessment for WSL before orthodontic treatment includes the following aspects. Additionally, Fig. 3 briefly illustrates the primary risks associated with dental demineralization. ORAL
HYGIENE STATUS The use of fixed orthodontic appliances during orthodontic treatment increases irregularities on the tooth surface, providing conditions for plaque attachment and retention,
thus increasing the difficulty of oral cleaning. Poor oral hygiene habits and inadequate tooth brushing can lead to plaque accumulation on the tooth surface, potentially causing enamel
demineralization, resulting in WSL. DEMINERALIZATION STATUS To determine a patient’s level of demineralization risk, a comprehensive medical history should be taken, including a series of
questions related to known risk factors for increased caries susceptibility or protective factors. This involves assessing the patient’s medical history and relevant social history (e.g.,
place of birth and upbringing, current residence, educational level, and occupation). All this information is crucial for evaluating demineralization risk at an individual level.56 By
assessing the patient’s past caries experience, one can reflect their susceptibility to dental demineralization. EATING HABITS The dietary structure, especially the frequency and quantity of
fermentable carbohydrate intake, and the impact of diet on oral pH were evaluated. FLUORIDE USE The use of fluoride-containing toothpaste, mouthwash, gels, etc., and whether the patient
received professional fluoride varnish or other fluoride-releasing material treatments were also assessed. Fluoride is an effective anticaries agent that promotes the remineralization of
dental enamel, inhibits plaque metabolism, and increases enamel acid resistance. The regular use of fluoride-containing toothpaste, mouthwash, or gels or the use of professional fluoride
varnish or other fluoride-releasing materials during orthodontic treatment can reduce the occurrence of WSL. SYSTEMIC FACTORS The presence of systemic diseases, long-term medication use, or
other factors that affect saliva secretion and oral microbiota balance were assessed. Some systemic diseases, medications, or other factors may also affect the risk of WSL during orthodontic
treatment, such as decreased saliva secretion, weakened immunity, diabetes, and Sjogren’s syndrome. PREVENTIVE METHODS FOR ENAMEL DEMINERALIZATION IN ORTHODONTIC TREATMENT To reduce the
occurrence of WSL before orthodontic treatment, oral health education needs to be part of the treatment plan, including the following aspects: ORAL HYGIENE INSTRUCTION AND HEALTH EDUCATION
Regular professional endodontic examination helps to detect early white chalky spots or caries on the tooth surface and to see the specialist in time.57 Regular professional periodontal
therapy should be carried out to remove plaque and calculus, prevent decreased pH on the tooth surface, and prevent damage to the enamel. For orthodontic patients with periodontal disease,
regular periodontal examination and treatment should also be conducted to control periodontal inflammation and biofilm formation. ORAL HEALTH CARE The teeth were brushed promptly after each
meal, at least 3 times a day, with each tooth lasting no less than 3 min. Special orthodontic dental floss can be used to clean gaps through brackets and archwires. If it is necessary to
clean the interproximal gaps between teeth, it must be performed under the f the doctor’s teaching. The food residue on the tooth surface and around the orthodontic appliances was cleaned
with a gentle up-and-down brushing motion to reduce plaque accumulation. In addition, disclosing agents can be used after brushing to more clearly show areas that still need cleaning,
increasing the interest in brushing teeth of patients, especially children, and further improving the effect of brushing teeth. USE OF FLUORIDE Fluoride reduces demineralization of dental
tissues via three different mechanisms.58,59,60 The first mechanism is that the presence of fluoride increases the formation and accumulation of fluorapatite. Fluorapatite is formed by the
combination of calcium ions and phosphate ions in saliva and has lower solubility than hydroxyapatite, increasing the acid resistance of enamel.61,62 The second mechanism is promoting the
direct remineralization of fluorapatite crystals on the surface of dental tissues undergoing demineralization. The third mechanism relies on the antibacterial activity of fluoride ions, and
low concentrations of fluoride can inhibit the production of glucosyltransferases. The main role of glucosyltransferases is to increase bacterial adhesion and provide glucose for
extracellular polysaccharide formation. Local fluoride application at high concentrations (12000 ppm) has a direct toxic effect on oral microbiota, including _Streptococcus mutans_.63
Fluoride can be classified as systemic or topical. Systemic application is effective for individuals at high risk of caries or in low-fluoride areas. According to the World Health
Organization’s report, a daily intake of 1 mg of fluoride is beneficial to health. Systemic fluoride application methods include adding fluoride to drinking water, salt, and milk, as well as
adding fluoride-containing tablets or drops to the diet. Topical applications, such as fluoride varnish, can extend the contact time with teeth and slowly release fluoride to prevent the
rapid loss of fluoride after use64,65. The American Academy of Pediatric Dentistry recommends using fluoride varnish at least 5% (22,600 ppm) on primary teeth twice a year and 2-4 times a
year on permanent teeth.66,67 As shown in Fig. 4, the process of applying topical fluoride is relatively simple. Briefly, the tooth surface is first cleaned and dried. Then, an appropriate
amount of fluoride is applied to the tooth surface. It is important to note that no eating should occur within 2 to 4 h after the fluoride application, and brushing should be avoided that
evening to ensure the effectiveness of the application. DIETARY GUIDANCE Forms of good eating habits include avoiding or reducing the consumption of sticky, hard, acidic, and high-sugar
foods, such as candies and carbonated drinks, to prevent tooth erosion. If the individual has snacks between meals or drinks carbonated drinks or milk tea, it is advisable to brush their
teeth or rinse their mouths promptly. The oral cavity was cleaned thoroughly before sleeping at night, ensuring that no food or drink residue remained to prevent the formation of dental
plaque that can corrode teeth. Improving oral hygiene and reducing the intake of cariogenic foods are essential measures for patients to reduce biofilm attachment and decrease acid-producing
bacteria (such as _Streptococcus mutans_) metabolism, effectively preventing the formation of WSL.68 Educating patients on healthy lifestyles is the best way to prevent oral health
problems. USE OF CHLORHEXIDINE Chlorhexidine (CHX) can significantly inhibit the growth of _Streptococcus mutans_, accelerating its remineralization. CHX is available in varnishes, gels, and
aqueous solutions. Studies have shown that protective varnish Cervitec F containing CHX can achieve persistent inhibition of _Streptococcus mutans_ compared to gels and mouth rinses while
also reducing the incidence of WSL.69,70,71 Although the safety of CHX has been confirmed, it can lead to side effects such as taste disturbance, oral mucosal staining, and contact
dermatitis. For orthodontic treatments with longer durations, the localized application of CHX varnish on the tooth surface is safer.72,73 KEY POINTS FOR PREVENTING DEMINERALIZATION WITH
VARIOUS ORTHODONTIC APPLIANCES Orthodontic treatments typically involve fixed appliances such as brackets on the labial or lingual side or clear aligners. Due to differences in the structure
and placement of these appliances in the patient’s oral cavity, methods to prevent enamel demineralization vary. For fixed appliances bonded to the tooth surface, such as brackets, the
presence of brackets and archwires hinders self-cleaning of the oral cavity and daily hygiene, requiring brushing and cleaning of food debris around the brackets after every meal to reduce
plaque accumulation.74 Compared to fixed appliances, clear aligners are transparent, removable, thermoplastic orthodontic devices that cover a larger area of the tooth surface. Although
clear aligners can be easily removed for cleaning, they need to be worn for 20 to 22 h daily. Failing to maintain good oral hygiene during wear could lead to severe enamel demineralization,
presenting as large and shallow areas of demineralization on the teeth.75 Therefore, before wearing clear aligners, it is important to clean the tooth surface. After drinking sugary drinks
while wearing them, rinsing the mouth promptly is necessary to prevent acidification that could lead to demineralization of tooth tissues. CLINICAL RECOMMENDATIONS FOR PREVENTING ENAMEL
DEMINERALIZATION IN ORTHODONTIC TREATMENT * Maintaining good oral hygiene is the primary method for preventing enamel demineralization in orthodontic treatment. Oral hygiene instructions and
health education are crucial. * Emphasis should be placed on the correct and effective toothbrushing method, ensuring both the duration and frequency of brushing and reducing the intake of
cariogenic foods. * The use of fluoride toothpaste for daily dental care should be encouraged to enhance the acid resistance of enamel and reduce demineralization. * After wearing
orthodontic appliances, it is essential to clean the oral cavity and the area around the appliances for food residue after each meal to prevent the formation of an acidic environment leading
to enamel demineralization. MANAGEMENT OF ENAMEL DEMINERALIZATION DURING ORTHODONTIC TREATMENT WSL on the tooth surface is a common complication in orthodontic patients with poor oral
hygiene.76 Factors such as microleakage at the bracket-adhesive-bracket interface, prolonged acid etching during bonding, extended orthodontic treatment duration, and lack of oral health
awareness in patients can all contribute to plaque accumulation, acid production by bacteria, decreased enamel pH, and subsequent enamel demineralization. Early detection of white spot
lesions during orthodontic treatment and timely implementation of appropriate management strategies are crucial for safeguarding dental health. ASSESS DEMINERALIZATION RISK THROUGHOUT THE
PROCESS OF ORTHODONTIC TREATMENT During orthodontic treatment, it is crucial to assess whether the patient’s risk of demineralization has increased during follow-up visits. This assessment
includes evaluating oral hygiene status, such as plaque accumulation, calculus deposition, and food impaction. If the risk of demineralization is found to be elevated, preventive methods and
endodontic treatment should be promptly employed to prevent the occurrence of dental demineralization. This includes the use of fluoride toothpaste, fluoride varnish, and mouth rinses
containing fluoride around orthodontic appliances.77 REMINERALIZATION AND ANTIBIOFILM COMBINED THERAPY The remineralization agent casein phosphopeptide-amorphous calcium phosphate (CPP-ACP)
stabilizes ACP by incorporating phosphorylated serine from casein, thus maintaining a state of supersaturation with Ca2+ and PO42- on the tooth surface and promoting the remineralization of
hard dental tissues.78 CPP-ACP is a good choice for WSL remineralization, and when combined with fluoride, it enhances the remineralizing effects of WSL.79,80 Although the application of
fluoride, CPP-ACP, and others has a positive effect on preventing WSL progression, these methods still lack aesthetic improvement,81 and further clinical evidence is needed to prove the
effectiveness of CPP-ACP in promoting WSL remineralization.82 Therefore, materials capable of stabilizing and delivering ACP directly to the tooth surface, apart from fluoride, are indeed
among the best choices for remineralizing hard dental tissues. With the ongoing research and translation of new biomimetic remineralization materials, the use of remineralizing agents is
certainly a robust means for the prevention and treatment of WSL. Based on the concept and technology of interrupting dental caries (IDC), in recent years, biomaterials targeting biofilms
and remineralization have been continuously emerging. Poly(carboxylic acid) succinyl chitosan acrylamide (PCBAA)/ACP nanocomposite materials not only provide ions but also prevent rapid
aggregation and spontaneous transformation of ions on the lesion surface, allowing calcium and phosphate ions to penetrate the gaps more effectively, accelerating internal crystal growth,
and promoting the formation of dense remineralization layers.83 Phase transition bovine serum albumin-octopamine (PTB-OCT) is a universal anticaries coating that not only induces
mineralization on the surface of hard dental tissues and resins but also exhibits acid resistance and antimicrobial properties, reducing primary caries and postfill microleakage.84
L-cysteine/graphiticyne/silver composite nanozymes (GDY/L-cys/Ag, GLA) inhibit dental plaque by producing reactive oxygen species, and GLA serves as a nucleation point, cross-linking with
saliva rich in Ca2+, attracting PO43-, promoting the formation of hydroxyapatite on enamel, and facilitating rapid remineralization[83]. the polymeric nature of invisible aligner materials,
future basic research and clinical translation may involve developing polymeric materials with fluoride ion slow-release capabilities, antimicrobial properties, or surface modifications to
resist biofilm formation. LASER THERAPY Carbon dioxide lasers with wavelengths of 9.3, 9.9, 10.3, and 10.6 μm are considered the main types of lasers for inhibiting demineralization of
dental tissues, as the absorption bands of phosphates, carbonates, and hydroxyl groups in enamel and dentin structures fall within the range of 9–11 μm. Laser absorption by enamel leads to
physical and chemical changes, including organic matrix decomposition, reduced carbonate compounds, and fusion and recrystallization of hydroxyapatite crystals, resulting in increased acid
resistance.85,86,87 Furthermore, research shows that low-energy lasers can reduce enamel demineralization by 90%.88,89 An Er: YAG laser with a wavelength of 2.94 μm is absorbed by water,
hydroxyapatite, and collagen.90,91,92 The subablative energy of the Er: YAG laser induces chemical changes in dental tissues without causing morphological damage. Studies suggest that the
combined use of lasers and fluoride can synergistically enhance the anti-demineralization ability of dental tissues, but clinical evidence is still lacking, with research remaining in the
preclinical stages.93,94,95,96 OZONE USE Ozone is a potent oxidizing agent that is destructive to various pathogens, displaying germicidal, antiviral, and antifungal activities by enhancing
tissue metabolism through oxidation.97,98 Studies have shown that the use of ozone can reduce the counts of streptococci and candida in saliva.99 The safe concentration range for ozone is
0.05-5%, and ozone is generally applied in the form of gas, gels, or aqueous solutions in the oral cavity and has good biocompatibility. OzonyTron-OZ (Mymed, Germany) is an intraoral ozone
gas disinfection device that kills pathogens within demineralized teeth by adjusting the silicone tray to adhere to the tooth surface and ozone gas flow, preventing further demineralization
of the teeth.100 However, the clinical application of ozone for remineralization still requires more evidence and appropriate research.101,102 MICROABRASION OF DENTAL HARD TISSUES The main
indication for microabrasion of dental hard tissues is intrinsic discoloration or texture changes caused byamelogenesis imperfecta or dental fluorosis.103 This technique uses slow-speed
dental handpieces with gels containing acid and abrasives to remove discoloured enamel and stains the tooth surface.104,105 Microabrasion is a minimally invasive treatment that involves
removing a certain amount of dental tissue. When removing the WSL from dental tissue, attention should be given to the thickness of the enamel in the cervical area.106 Research has shown
that microabrasion improves the aesthetics of teeth with white spot lesions and demonstrates durability for at least 12 months. However, compared to microabrasion, resin infiltration has
better aesthetic improvement effects after 12 months.107,108 USE OF BLEACHING AGENTS In vitro studies have shown that bleaching can improve the aesthetics of teeth with WSL. However, the
bleaching process only enhances the appearance, disguising white spot lesions instead of treating them.109 Although bleaching WSL in vitro can reduce the differences in color between carious
and unaffected areas, there is still no clear evidence for its clinical application.110,111 RESIN INFILTRATION TREATMENT During WSL development, there is an increase in microporosity in the
enamel. Low-viscosity light-curing resin infiltrates the microporous enamel area of WSL through capillary action, sealing the micropores and increasing the strength of the enamel, providing
mechanical support to inhibit the progression of WSL.112,113,114,115,116 During WSL treatment, resin infiltration results in better aesthetic results than minor adjustments. The ability to
camouflage WSL is mainly due to the refractive index of the infiltrated resin being close to that of hydroxyapatite crystals.104,117,118 In conclusion, different treatment options can be
chosen based on the severity of the WSL that occurs during orthodontic treatment. For WSL with a Gorelick score of 3 or below, the localized use of fluoride combined with remineralizing
agents may promote enamel remineralization.WSL with a score of 3 or above would require minimally invasive treatment. CLINICAL MANAGEMENT AND TREATMENT OF POSTORTHODONTIC WSL After
orthodontic treatment is completed and the orthodontic appliance is removed, the health of the dental hard tissues and periodontal tissues needs to be reassessed. When necessary,
consultation and treatment from disciplines such as dental pulp therapy, prosthodontics, periodontics, and preventive dentistry may be needed. OTHER CONSIDERATIONS IN ORTHODONTICS:
MANAGEMENT OF ENAMEL DEMINERALIZATION IN EARLY ORTHODONTIC TREATMENT FOR CHILDREN AND ADOLESCENTS Due to the young age and long duration of orthodontic treatment in children and adolescents,
awareness of maintaining good oral hygiene is often lacking. Since enamel mineralization in children and adolescents is incomplete, the risk of developing WSL during orthodontic treatment
is greater. Uncontrolled progression of WSL can lead to dental caries and even pulp disease, affecting tooth development.119 Oral hygiene guidance for children and education for parents are
necessary prior to orthodontic treatment for children and adolescents. If needed, fluoridated toothpaste should be used for brushing, along with disclosing agents to maintain good oral
hygiene. Early pit and fissure sealants for molars should be applied. During each follow-up visit, monitoring of oral hygiene status, such as plaque, calculus, and gum health, should be
conducted to prevent the causative factors of WSL. If WSL has already developed during orthodontic treatment, localized fluoride application, the use of remineralizing agents, or resin
infiltration can be considered for treatment. Further oral hygiene education for children and parents is essential.120 If the WSL continues to progress, it may be necessary to replace the
orthodontic appliance with one that is easier to clean or to temporarily remove the appliance until effective control of the WSL is achieved before continuing orthodontic treatment.
RECOMMENDED CLINICAL PROCEDURES FOR THE PREVENTION AND TREATMENT OF WSL DURING THE WHOLE ORTHODONTIC TREATMENT PROCESS The management of WSL should start at the first visit before
orthodontic treatment and become part of the treatment plan. Health education throughout the orthodontic process should aim to improve patients’ lifestyle for better oral health, emphasizing
prevention over treatment. Treatment should initially involve conservative, noninvasive, and reversible methods. If these methods do not effectively resolve WSL, a more proactive approach
may be necessary (Fig. 1).121,122,123,124 * Before orthodontic treatment, it is necessary to fully evaluate the risk factors for dental caries. Only when the risk factors are under control,
the subsequent orthodontic treatment could proceed. * During orthodontic treatment, it is essential to monitor the occurrence of WSL at each follow-up visit and intervene promptly. The
primary focus should be on enhancing oral hygiene education, maintaining good oral health, and using fluoride and remineralizing agents locally to promote WSL remineralization. * If the
progression of WSL on the tooth surface during orthodontic treatment is uncontrollable, replace the orthodontic appliance with an easier-to-clean appliance or temporarily suspend orthodontic
treatment until the WSL is effectively controlled. * After orthodontic treatment, a multidisciplinary approach should be taken based on the severity of tooth demineralization after
appliance removal. * For orthodontic treatment in children and adolescents, oral hygiene education is necessary for guardians to ensure patient compliance with treatment and reduce the
occurrence of WSL. THE RESEARCH PROSPECTS OF WSL TREATMENT As the person in charge of orthodontic treatment, dentists providing orthodontic treatment have a responsibility to conduct
in-depth research on the mechanism of WSL so that the technological means in the clinic and basic research in the laboratory complement each other, using a combination of measures to
increase the prevention and treatment of WSL to new heights. In the field of basic research, it is possible to study biomimetic remineralization methods for rapid and efficient restoration
of natural/synthetic enamel hard tissues and combine them with antibiofilm technologies to block WSL in the early stages before it develops into severe caries. In the future, orthodontists
can closely collaborate and cooperate with oral prevention physicians, dental pulp physicians, and oral material researchers to develop a material that not only resists biofilms but also
rapidly and effectively repairs demineralized enamel in a form closest to natural occurrence to reduce the risk of WSL during orthodontic procedures, ultimately aiming to improve the
effectiveness of orthodontic treatment. WSL involves not only a continuous loss of minerals in teeth but also a dynamic process of demineralization and remineralization. It is an early
manifestation of caries. The progression of the disease depends on the balance between the pathological factors of demineralization (cariogenic bacteria, carbohydrates, and reduced saliva
secretion) and protective factors (antimicrobials, adequate saliva, and remineralizing ions).125 The management of WSL occurring during orthodontic treatment should focus on prevention,
reducing pathological factors of demineralization, increasing protective factors, and elevating patients’ awareness of maintaining dental hard tissues throughout the entire orthodontic
treatment process through oral health education to reduce the occurrence of WSL. For WSL that occurs before or during orthodontic treatment, treatment methods mainly include promoting the
remineralization of dental hard tissues, reducing demineralization of dental hard tissues, and restoring aesthetics after demineralization of tooth surfaces. WSL remineralization treatment
promotes the deposition of exogenous calcium and phosphate ions into demineralized crystal voids to increase the mineral content. According to the principle of biomimetic remineralization,
polymer membrane modifications are used to induce hydroxyapatite deposition directly on demineralized enamel or dentin surfaces or by utilizing polymer additives such as casein
phosphopeptide (CPP), carboxymethyl chitosan, amelogenin-like proteins, polyaspartic acid (PASP), and polyacrylic esters (PAA), simulating noncollagen proteins (NCPs) or nonenamel proteins
in the biological mineralization process by stabilizing precursor phases and promoting precursor ion infiltration, mediating the process of transforming amorphous calcium phosphate (ACP) to
the crystalline hydroxyapatite mineral phase.126,127 For WSL with a Gorelick score of 3 or higher, it is difficult for remineralization treatment to restore enamel defects on the tooth
surface. The current treatment options mainly involve selecting minimally invasive aesthetic restorations based on the size of the defect or veneer restorations to address aesthetic
concerns. Minimally invasive aesthetic restorations involve abrasing white chalky lesions on the tooth surface with microabrasive paste and restoring tooth morphology with infiltrating
resin. Veneers entail uniformly removing surface demineralized discoloured tooth tissue and covering the tooth surface with veneers made of ceramic materials similar in color to healthy
tooth tissue using bonding techniques to achieve restoration effects. Although aesthetic restorations can maximally restore tooth surface morphology, irreversible damage is also caused to
the tooth structure itself during the removal of diseased tissue. Modern caries management focuses on primary prevention, achieving and maintaining tooth health by optimizing clinical
decisions, stopping the progression of initial lesions, preserving tooth structure, and resorting to filling therapy only when necessary.128 The biomimetic remineralization method simulating
natural mineralization processes provides a promising strategy for the treatment of WSL. And Yuxing Bai et al. used nanostructured resin infiltrant containing calcium phosphate
nanoparticles to treat WSL of enamel and achieved satisfactory results.129 However, normal enamel and dentin structures are difficult to form, and the remineralized areas on the surfaces of
demineralized enamel and dentin, which are generally less than 10 µm thick, are too thin to resist occlusal forces and the mechanical friction of food mastication. Research on the treatment
of dental hypoplasia is still in its early stages. The occurrence and development of WSL have become oral health issues that cannot be ignored in orthodontic processes. The development of
restoration materials that promote the biomimetic remineralization of WSL and possess excellent mechanical properties holds broad application prospects for WSL treatment. With the
comprehensive arrival of the artificial intelligence era, orthodontics and the field of artificial intelligence are continuously emerging, driving the development and innovation of
orthodontics. In the future, it will be possible to utilize AI-based technological methods, in conjunction with existing examination methods for WSL, to personalize the monitoring of teeth
during orthodontic processes. This can predict the development and prognosis of WSL at an early stage, alert patients to the risk of WSL occurrence, and further reduce the impact of WSL on
orthodontic processes. At the same time, orthodontists need to realize that artificial intelligence only plays a supplementary role in orthodontic processes. Various emerging technologies
cannot fully replace the role of orthodontists in preventing and diagnosing WSL. Orthodontists still need to enhance their understanding of WSL, identify early signs of chalky lesions
promptly, and intervene when necessary. REFERENCES * Skidmore, K. J., Brook, K. J., Thomson, W. M. & Harding, W. J. Factors influencing treatment time in orthodontic patients. _Am. J.
Orthod. Dentofac._ 129, 230–238 (2006). Article Google Scholar * B, F., ZL, J., YX, B., L, W. & ZH, Z. Experts consensus on diagnostic and therapeutic strategies for malocclusions at
early developing stage. _Shanghai Kou Qiang Yi Xue_ 30, 449–455 (2021). Google Scholar * XJ, G. Dental and endodontic basic knowledges related in orthodontic treatment. _Chin. J. Orthod._
23, 167–170 (2016). Google Scholar * Selwitz, R. H., Ismail, A. I. & Pitts, N. B. Dental caries. _Lancet_ 369, 51–59 (2007). Article CAS PubMed Google Scholar * Marinelli, G. et al.
White spot lesions in orthodontics: prevention and treatment. A descriptive review. _J. Biol. Reg. Homeos Ag._ 35, 227–240 (2021). CAS Google Scholar * Maxfield, B. J. et al. Development
of white spot lesions during orthodontic treatment: Perceptions of patients, parents, orthodontists, and general dentists. _Am. J. Orthod. Dentofac._ 141, 337–344 (2012). Article Google
Scholar * Øgaard, B., Rølla, G. & Arends, J. Orthodontic appliances and enamel demineralization: Part 1. Lesion development. _Am. J. Orthod. Dentofac._ 94, 68–73 (1988). Article Google
Scholar * YX, B. Risk perception and management in orthodontic treatment. _Chinese J. Stomatology._ 12, 793–797 (2019). * Julien, K. C., Buschang, P. H. & Campbell, P. M. Prevalence of
white spot lesion formation during orthodontic treatment. _Angle Orthod._ 83, 641–647 (2013). Article PubMed PubMed Central Google Scholar * Buschang, P. H., Chastain, D., Keylor, C.
L., Crosby, D. & Julien, K. C. Incidence of white spot lesions among patients treated with clear aligners and traditional braces. _Angle Orthod._ 89, 359–364 (2019). Article PubMed
Google Scholar * Albhaisi, Z., Al-Khateeb, S. N. & Abu Alhaija, E. S. Enamel demineralization during clear aligner orthodontic treatment compared with fixed appliance therapy, evaluated
with quantitative light-induced fluorescence: A randomized clinical trial. _Am. J. Orthod. Dentofac. Orthop._ 157, 594–601 (2020). Article Google Scholar * Gorelick, L., Geiger, A. M.
& Gwinnett, A. J. Incidence of white spot formation after bonding and banding. _Am. J. Orthod._ 81, 93–98 (1982). Article CAS PubMed Google Scholar * Lucchese, A. & Gherlone, E.
Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. _Eur. J. Orthod._ 35, 664–668 (2013). Article PubMed Google Scholar * Heymann, G. C. &
Grauer, D. A contemporary review of white spot lesions in orthodontics. _J. Esthet. Restor. Dent._ 25, 85–95 (2013). Article PubMed Google Scholar * Chatterjee, R. & Kleinberg, I.
Effect of orthodontic band placement on the chemical composition of human incisor tooth plaque. _Arch. Oral. Biol._ 24, 97–100 (1979). Article CAS PubMed Google Scholar * Mattingly, J.,
Sauer, G., Yancey, J. & Arnold, R. Enhancement of Streptococcus mutans colonization by direct bonded orthodontic appliances. _J. Dent. Res._ 62, 1209–1211 (1983). Article CAS PubMed
Google Scholar * Rosenbloom, R. G. & Tinanoff, N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. _Am. J. Orthod. Dentofac._ 100, 35–37
(1991). Article CAS Google Scholar * Pitts, N. B. et al. Dental caries. _Nat. Rev. Dis. Prim._ 3, 1–16 (2017). Google Scholar * Lopes, P. C. et al. White spot lesions: diagnosis and
treatment–a systematic review. _BMC Oral. Health_ 24, 1–18 (2024). Article Google Scholar * Zou, J. et al. Expert consensus on early childhood caries management. _Int J. Oral. Sci._ 14, 35
(2022). Article PubMed PubMed Central Google Scholar * NouhzadehMalekshah, S., Fekrazad, R., Bargrizan, M. & Kalhori, K. A. Evaluation of laser fluorescence in combination with
photosensitizers for detection of demineralized lesions. _Photodiagn. Photodyn. Ther._ 26, 300–305 (2019). Article CAS Google Scholar * Foros, P., Oikonomou, E., Koletsi, D. &
Rahiotis, C. Detection methods for early caries diagnosis: A systematic review and meta-analysis. _Caries Res._ 55, 247–259 (2021). Article PubMed Google Scholar * Pitts, N. B. &
Stamm, J. W. International Consensus Workshop on Caries Clinical Trials (ICW-CCT)—Final Consensus Statements: Agreeing Where the Evidence Leads. _J. Dent. Res._ 83, 125–128 (2004). Article
Google Scholar * Zandoná, A. F. & Zero, D. T. Diagnostic tools for early caries detection. _J. Am. Dent. Assoc._ 137, 1675–1684 (2006). Article PubMed Google Scholar * Kidd, E. &
Fejerskov, O. What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. _J. Dent. Res._ 83, 35–38 (2004). Article Google
Scholar * Sadıkoğlu, İ. S. White spot lesions: recent detection and treatment methods. _Cyprus J. Med. Sci._ 5, 260–266 (2020). Article Google Scholar * Askar, H. et al. Detecting white
spot lesions on dental photography using deep learning: A pilot study. _J. Dent._ 107, 103615 (2021). Article CAS PubMed Google Scholar * Estai, M. et al. Comparison of a
smartphone-based photographic method with face-to-face caries assessment: a mobile teledentistry model. _Telemed. J. E-health_ 23, 435–440 (2017). Article PubMed Google Scholar * Lee,
H.-S., Lee, Y.-D., Kim, S.-K., Choi, J.-H. & Kim, B.-I. Assessment of tooth wear based on autofluorescence properties measured using the QLF technology in vitro. _Photodiagn. Photodyn._
25, 265–270 (2019). Article Google Scholar * Knaup, I. et al. Correlation of quantitative light-induced fluorescence and qualitative visual rating in infiltrated post-orthodontic white
spot lesions. _Eur. J. Orthod._ 45, 133–141 (2023). Article PubMed Google Scholar * Kim, H.-E. Red Fluorescence Intensity as a Criterion for Assessing Remineralization Efficacy in Early
Carious Lesions. _Photodiagn. Photodyn._ 103963 (2024). * Chandra, S. & Garg, N. _Textbook of operative dentistry_. (Jaypee Brothers Publishers, 2008). * Park, S.-W. et al. Lesion
activity assessment of early caries using dye-enhanced quantitative light-induced fluorescence. _Sci. Rep._ 12, 11848 (2022). Article CAS PubMed PubMed Central Google Scholar *
Warkhankar, A., Tanpure, V. R. & Wajekar, N. A. Using light fluorescence technique as an emerging approach in treating dental caries. _Int. J. Prevent. Clin. Dent. Res._ 10, 69–72
(2023). Article Google Scholar * Macey, R. et al. Fluorescence devices for the detection of dental caries. _Cochrane Db. Syst. Rev._ 12, CD013811 (2020). Google Scholar * Sürme, K., Kara,
N. B. & Yilmaz, Y. In Vitro Evaluation of Occlusal Caries Detection Methods in Primary and Permanent Teeth: A Comparison of CarieScan PRO, DIAGNOdent Pen, and DIAGNOcam Methods.
_Photobiomodul. Photomed. Laser Surg._ 38, 105–111 (2020). PubMed Google Scholar * Hogan, R., Pretty, I. A. & Ellwood, R. P. in _Detection and Assessment of Dental Caries: A Clinical
Guide_ (eds Andrea Ferreira Zandona & Christopher Longbottom) 139-150 (Springer International Publishing, 2019). * Schwendicke, F., Elhennawy, K., Paris, S., Friebertshäuser, P. &
Krois, J. Deep learning for caries lesion detection in near-infrared light transillumination images: A pilot study. _J. Dent._ 92, 103260 (2020). Article CAS PubMed Google Scholar *
Fried, D., Glena, R. E., Featherstone, J. D. & Seka, W. Nature of light scattering in dental enamel and dentin at visible and near-infrared wavelengths. _Appl. Opt._ 34, 1278–1285
(1995). Article CAS PubMed Google Scholar * Stratigaki, E. et al. Clinical validation of near-infrared light transillumination for early proximal caries detection using a composite
reference standard. _J. Dent._ 103, 100025 (2020). Article Google Scholar * Abogazalah, N. & Ando, M. Alternative methods to visual and radiographic examinations for approximal caries
detection. _J. Oral. Sci._ 59, 315–322 (2017). Article PubMed Google Scholar * Y, Y., JQ, X. & JJ, S. Application progress of fiber optic transillumination in caries diagnosis.
_Beijing J. Stomatology_ 28, 118–120 (2020). * Longbottom, C. & Huysmans, M.-C. Electrical measurements for use in caries clinical trials. _J. Dent. Res._ 83, 76–79 (2004). Article
Google Scholar * Wolinsky, L. E. et al. An in vitro assessment and a pilot clinical study of electrical resistance of demineralized enamel. _Int. J. Clin. Dent._ 10, 40–43 (1999). CAS
Google Scholar * Wang, J., Someya, Y., Inaba, D., Longbottom, C. & Miyazaki, H. Relationship between electrical resistance measurements and microradiographic variables during
remineralization of softened enamel lesions. _Caries Res._ 39, 60–64 (2005). Article PubMed Google Scholar * Sannino, I., Angelini, E., Parvis, M., Arpaia, P. & Grassini, S. in _2022_
_IEEE International Instrumentation and Measurement Technology Conference (I2MTC)_. 1–5 (IEEE). * Shimada, Y., Yoshiyama, M., Tagami, J. & Sumi, Y. Evaluation of dental caries, tooth
crack, and age-related changes in tooth structure using optical coherence tomography. _Jpn. Dent. Sci. Rev._ 56, 109–118 (2020). Article PubMed PubMed Central Google Scholar * Ibusuki,
T. et al. Observation of white spot lesions using swept source optical coherence tomography (SS-OCT): in vitro and in vivo study. _Dent. Mater. J._ 34, 545–552 (2015). Article CAS PubMed
Google Scholar * Kühnisch, J., Meyer, O., Hesenius, M., Hickel, R. & Gruhn, V. Caries detection on intraoral images using artificial intelligence. _J. Dent. Res._ 101, 158–165 (2022).
Article PubMed Google Scholar * Kim, J., Shin, T. J., Kong, H. J., Hwang, J. Y. & Hyun, H. K. High-Frequency Ultrasound Imaging for Examination of Early Dental Caries. _J. Dent. Res._
98, 363–367 (2019). Article CAS PubMed Google Scholar * Xing, H., Eckert, G. J. & Ando, M. Impact of angle on photothermal radiometry and modulated luminescence (PTR/LUM) value. _J.
Dent._ 132, 104500 (2023). Article CAS PubMed Google Scholar * Liang, J. P. Research and application of new techniques for early diagnosis of caries. _Chin. J. Stomatol._ 56, 33–38
(2021). CAS Google Scholar * Kwon, T. H., Salem, D. M. & Levin, L. in _Semin Orthod_. (Elsevier). * Bishara, S. E. & Ostby, A. W. White Spot Lesions: Formation, Prevention, and
Treatment. _SEMIN ORTHOD_ 14, 174–182 (2008). Article Google Scholar * Ogaard, B. Enamel effects during bonding-debonding and treatment with fixed appliances. _Risk Management in
Orthodontics: Experts’ Guide to Malpractice Ch.3_ (Quintessence Publishing Co., 2004). * Disney, J. A. et al. The University of North Carolina Caries Risk Assessment study: further
developments in caries risk prediction. _Community Dent. oral. Epidemiol._ 20, 64–75 (1992). Article CAS PubMed Google Scholar * S, L. & M, H. A Review of Enamel Demineralization in
Orthodontic Treatment with Fixed Appliances. _J. Oral. Sci. Res._ 37, 685–688 (2021). Google Scholar * Marinho, V. Cochrane reviews of randomized trials of fluoride therapies for preventing
dental caries. _Eur. J. Paediatr. Dent._ 10, 183–191 (2009). Article CAS Google Scholar * Weyland, M. I., Jost-Brinkmann, P.-G. & Bartzela, T. Management of white spot lesions
induced during orthodontic treatment with multibracket appliance: a national-based survey. _Clin. Oral. Invest_ 26, 4871–4883 (2022). Article Google Scholar * Sardana, D. et al.
Effectiveness of professional fluorides against enamel white spot lesions during fixed orthodontic treatment: a systematic review and meta-analysis. _J. Dent._ 82, 1–10 (2019). Article CAS
PubMed Google Scholar * Simmer, J. P., Hardy, N. C., Chinoy, A. F., Bartlett, J. D. & Hu, J. C. How fluoride protects dental enamel from demineralization. _J. Int Soc. Prev. Commun._
10, 134 (2020). Article Google Scholar * Song, H., Cai, M., Fu, Z. & Zou, Z. Mineralization Pathways of Amorphous Calcium Phosphate in the Presence of Fluoride. _Cryst. Growth Des._
23, 7150–7158 (2023). Article CAS Google Scholar * Zhang, Q. et al. Application of fluoride disturbs plaque microecology and promotes remineralization of enamel initial caries. _J. Oral.
Microbiol._ 14, 2105022 (2022). Article PubMed PubMed Central Google Scholar * Øgaard, B. in _Semin Orthod_. 183-193 (Elsevier). * Øgaard, B., Larsson, E., Henriksson, T., Birkhed, D.
& Bishara, S. E. Effects of combined application of antimicrobial and fluoride varnishes in orthodontic patients. _Am. J. Orthod. Dentofac._ 120, 28–35 (2001). Article Google Scholar *
American Academy of Pediatric Dentistry. Fluoride Therapy [J]. _Pediatr Dent_, 39, 242–245 (2017). * Alexander, S. A. & Ripa, L. W. Effects of self-applied topical fluoride preparations
in orthodontic patients. _Angle Orthod._ 70, 424–430 (2000). CAS PubMed Google Scholar * Hancock, S., Zinn, C. & Schofield, G. The consumption of processed sugar‐and
starch‐containing foods, and dental caries: a systematic review. _Eur. J. Oral. Sci._ 128, 467–475 (2020). Article CAS PubMed Google Scholar * Schaeken, M. J. & De Haan, P. Effects
of sustained-release chlorhexidine acetate on the human dental plaque flora. _J. Dent. Res._ 68, 119–123 (1989). Article CAS PubMed Google Scholar * Sajadi, F. S., Moradi, M., Pardakhty,
A., Yazdizadeh, R. & Madani, F. Effect of fluoride, chlorhexidine and fluoride-chlorhexidine mouthwashes on salivary Streptococcus mutans count and the prevalence of oral side effects.
_J. Dent. Res., Dent. Clin., Dent. prospects_ 9, 49 (2015). Article Google Scholar * Kamarudin, Y., Skeats, M. K., Ireland, A. J. & Barbour, M. E. Chlorhexidine hexametaphosphate as a
coating for elastomeric ligatures with sustained antimicrobial properties: A laboratory study. _Am. J. Orthod. Dentofac._ 158, e73–e82 (2020). Article Google Scholar * Jones, C. G.
Chlorhexidine: is it still the gold standard? _Periodontol 2000_ 15, 55–62 (1997). Article CAS PubMed Google Scholar * Fardai, O. & Turnbull, R. S. A review of the literature on use
of chlorhexidine in dentistry. _Assoc. J. Am. Dent. Assoc._ 112, 863–869 (1986). Article Google Scholar * Baumer, C. et al. Orthodontists’ instructions for oral hygiene in patients with
removable and fixed orthodontic appliances. _Int. J. Dent. Hyg._ (2023). * Raghavan, S., Abu Alhaija, E. S., Duggal, M. S., Narasimhan, S. & Al-Maweri, S. A. White spot lesions, plaque
accumulation and salivary caries-associated bacteria in clear aligners compared to fixed orthodontic treatment. A systematic review and meta-analysis. _BMC Oral. Health_ 23, 599 (2023). *
Sardana, D., Schwendicke, F., Kosan, E. & Tüfekçi, E. White spot lesions in orthodontics: consensus statements for prevention and management. _Angle Orthod._ 93, 621–628 (2023). Article
PubMed PubMed Central Google Scholar * Ten Cate, J., Buijs, M., Miller, C. C. & Exterkate, R. Elevated fluoride products enhance remineralization of advanced enamel lesions. _J.
Dent. Res._ 87, 943–947 (2008). Article PubMed Google Scholar * Reynolds, E. Casein phosphopeptide-amorphous calcium phosphate: the scientific evidence. _Adv. Dent. Res._ 21, 25–29
(2009). Article CAS PubMed Google Scholar * Karabekiroğlu, S. et al. Treatment of post-orthodontic white spot lesions with CPP-ACP paste: A three year follow up study. _Dent. Mater. J._
36, 791–797 (2017). Article PubMed Google Scholar * de Oliveira, P. R. A., Barreto, L. S. D. C. & Tostes, M. A. Effectiveness of CPP‐ACP and fluoride products in tooth
remineralization. _Int J. Dent. Hyg._ 20, 635–642 (2022). Article PubMed Google Scholar * Bourouni, S., Dritsas, K., Kloukos, D. & Wierichs, R. J. Efficacy of resin infiltration to
mask post-orthodontic or non-post-orthodontic white spot lesions or fluorosis—a systematic review and meta-analysis. _Clin. Oral. Invest_ 25, 4711–4719 (2021). Article CAS Google Scholar
* Xiaotong, W., Nanquan, R., Jing, X., Yuming, Z. & Lihong, G. Remineralization effect of casein phosphopeptide-amorphous calcium phosphate for enamel demineralization: a system review.
_Hua Xi Kou Qiang Yi Xue Za Zhi_ 35, 629–635 (2017). PubMed Google Scholar * He, J. et al. Polyzwitterion Manipulates Remineralization and Antibiofilm Functions against Dental
Demineralization. _ACS Nano_ 16, 3119–3134 (2022). Article CAS PubMed Google Scholar * Liao, J. et al. Stimuli-responsive graphdiyne-silver nanozymes for catalytic ion therapy of dental
caries through targeted biofilms removal and remineralization. _Nano Today_ 55, 102204 (2024). Article CAS Google Scholar * Tagomori, S. & Morioka, T. Combined effects of laser and
fluoride on acid resistance of human dental enamel. _Caries Res._ 23, 225–231 (1989). Article CAS PubMed Google Scholar * Kuroda, S. & Fowler, B. Compositional, structural, and phase
changes in in vitro laser-irradiated human tooth enamel. _Calcif. Tissue Int._ 36, 361–369 (1984). Article CAS PubMed Google Scholar * Rafiei, E., Fadaei Tehrani, P., Yassaei, S. &
Haerian, A. Effect of CO 2 laser (10.6 μm) and Remin Pro on microhardness of enamel white spot lesions. _Laser Med. Sci._ 35, 1193–1203 (2020). Article Google Scholar * Bevilácqua, F. M.,
Zezell, D. M., Magnani, R., da Ana, P. A. & Eduardo Cde, P. Fluoride uptake and acid resistance of enamel irradiated with Er:YAG laser. _Lasers Med. Sci._ 23, 141–147 (2008). Article
PubMed Google Scholar * Liu, Y., Hsu, C. Y., Teo, C. M. & Teoh, S. H. Potential mechanism for the laser-fluoride effect on enamel demineralization. _J. Dent. Res._ 92, 71–75 (2013).
Article CAS PubMed Google Scholar * Doneria, D. et al. Erbium lasers in paediatric dentistry. _Int J. Healthc. Sci._ 3, 604–610 (2015). Google Scholar * Delbem, A. C. B., Cury, J.,
Nakassima, C., Gouveia, V. & Theodoro, L. H. Effect of Er: YAG laser on CaF2 formation and its anti-cariogenic action on human enamel: an in vitro study. _J. clin. laser med. surg._ 21,
197–201 (2003). Article CAS PubMed Google Scholar * Morioka, T., Tagomori, S. & Oho, T. Acid resistance of lased human enamel with Erbium: YAG laser. _J. clin. laser med. surg._ 9,
215–217 (1991). Article Google Scholar * Mathew, A. et al. Acquired acid resistance of human enamel treated with laser (Er:YAG laser and Co2 laser) and acidulated phosphate fluoride
treatment: An in vitro atomic emission spectrometry analysis. _Contemp. Clin. Dent._ 4, 170–175 (2013). Article PubMed PubMed Central Google Scholar * Assarzadeh, H., Karrabi, M.,
Fekrazad, R. & Tabarraei, Y. Effect of Er: YAG laser irradiation and acidulated phosphate fluoride therapy on re-mineralization of white spot lesions. _J. Dent._ 22, 153 (2021). Google
Scholar * Ramezani, K. et al. Combined Effect of Fluoride Mouthwash and Sub-ablative Er: YAG Laser for Prevention of White Spot Lesions around Orthodontic Brackets. _Open Dent. J._ 16,
(2022). * Pinelli, C., Campos Serra, M. & de Castro Monteiro Loffredo, L. Validity and reproducibility of a laser fluorescence system for detecting the activity of white-spot lesions on
free smooth surfaces in vivo. _Caries Res._ 36, 19–24 (2002). * Grootveld, M., Silwood, C. J. & Lynch, E. High Resolution^ 1H NMR investigations of the oxidative consumption of salivary
biomolecules by ozone: Relevance to the therapeutic applications of this agent in clinical dentistry. _Biofactors_ 27, 5–18 (2006). Article CAS PubMed Google Scholar * Grocholewicz, K.,
Mikłasz, P., Zawiślak, A., Sobolewska, E. & Janiszewska-Olszowska, J. Fluoride varnish, ozone and octenidine reduce the incidence of white spot lesions and caries during orthodontic
treatment: randomized controlled trial. _Sci. Rep._ 12, 13985 (2022). Article CAS PubMed PubMed Central Google Scholar * Baysan, A., Whiley, R. & Lynch, E. Antimicrobial effect of a
novel ozone–generating device on micro–organisms associated with primary root carious lesions in vitro. _Caries Res._ 34, 498–501 (2000). Article CAS PubMed Google Scholar * Sen, S.
& Sen, S. Ozone therapy a new vista in dentistry: integrated review. _Med. gas. Res._ 10, 189 (2020). Article CAS PubMed PubMed Central Google Scholar * Liaqat, S. et al.
Therapeutic effects and uses of ozone in dentistry: A systematic review. _Ozone.: Sci. Eng._ 45, 387–397 (2023). Article CAS Google Scholar * Rickard, G. D., Richardson, R. J., Johnson,
T. M., McColl, D. C. & Hooper, L. Ozone therapy for the treatment of dental caries. _Cochrane Db. Syst. Rev._ (2004). * Sundfeld, R. H., Croll, T. P., Briso, A. & De Alexandre, R. S.
Considerations about enamel microabrasion after 18 years. _Am. J. Dent._ 20, 67–72 (2007). * Shan, D. et al. A comparison of resin infiltration and microabrasion for postorthodontic white
spot lesion. _Am. J. Orthod. Dentofac._ 160, 516–522 (2021). Article Google Scholar * Croll, T. P. Enamel microabrasion: the technique. _Quintessence Int._ 20, 359–400 (1989). Google
Scholar * Pini, N. I. et al. Enamel microabrasion: An overview of clinical and scientific considerations. _World J. Clin. Cases_ 3, 34–41 (2015). Article PubMed PubMed Central Google
Scholar * Gu, X. et al. Esthetic improvements of postorthodontic white-spot lesions treated with resin infiltration and microabrasion: A split-mouth, randomized clinical trial. _Angle
Orthod._ 89, 372–377 (2019). Article PubMed PubMed Central Google Scholar * Paris, S., Meyer-Lueckel, H., Cölfen, H. & Kielbassa, A. M. Penetration coefficients of commercially
available and experimental composites intended to infiltrate enamel carious lesions. _Dent. Mater._ 23, 742–748 (2007). Article CAS PubMed Google Scholar * Kim, Y., Son, H. H., Yi, K.,
Ahn, J. S. & Chang, J. Bleaching Effects on Color, Chemical, and Mechanical Properties of White Spot Lesions. _Oper. Dent._ 41, 318–326 (2016). Article CAS PubMed Google Scholar *
Gizani, S., Kloukos, D., Papadimitriou, A., Roumani, T. & Twetman, S. Is bleaching effective in managing post-orthodontic white-spot lesions? A systematic review. _Oral. Health Prev.
Dent._ 18, 1–10 (2020). Google Scholar * Sawaf, H., Kassem, H. E. & Enany, N. M. TOOTH COLOR UNIFORMITY FOLLOWING WHITE SPOT LESION TREATMENT WITH RESIN INFILTRATION OR BLEACHING IN
VITRO STUDY. _Egypt. Orthodontic J._ 56, 51–60 (2019). Article Google Scholar * Meyer-Lueckel, H. & Paris, S. Improved resin infiltration of natural caries lesions. _J. Dent. Res._ 87,
1112–1116 (2008). Article CAS PubMed Google Scholar * Chatzimarkou, S., Koletsi, D. & Kavvadia, K. The effect of resin infiltration on proximal caries lesions in primary and
permanent teeth. A systematic review and meta-analysis of clinical trials. _J. Dent._ 77, 8–17 (2018). Article CAS PubMed Google Scholar * Roberson, T., Heymann, H. & Swift, E.
(Elsevier, 2006). * Meyer-Lueckel, H., Chatzidakis, A., Naumann, M., Dörfer, C. E. & Paris, S. Influence of application time on penetration of an infiltrant into natural enamel caries.
_J. Dent._ 39, 465–469 (2011). Article CAS PubMed Google Scholar * Perdigão, J. Resin infiltration of enamel white spot lesions: An ultramorphological analysis. _J. Esthet. Restor.
Dent._ 32, 317–324 (2020). Article PubMed Google Scholar * Kim, S., Kim, E. Y., Jeong, T. S. & Kim, J. W. The evaluation of resin infiltration for masking labial enamel white spot
lesions. _Int J. Paediatr. Dent._ 21, 241–248 (2011). Article PubMed Google Scholar * Rocha Gomes Torres, C., Borges, A. B., Torres, L. M., Gomes, I. S. & de Oliveira, R. S. Effect of
caries infiltration technique and fluoride therapy on the colour masking of white spot lesions. _J. Dent._ 39, 202–207 (2011). Article PubMed Google Scholar * Zhou, C. et al. Expert
consensus on pediatric orthodontic therapies of malocclusions in children. _Int J. Oral. Sci._ 16, 32 (2024). Article PubMed PubMed Central Google Scholar * Ozgur, B., Unverdi, G. E.,
Ertan, A. & Cehreli, Z. Effectiveness and color stability of resin infiltration on demineralized and hypomineralized (MIH) enamel in children: six-month results of a prospective trial.
_Oper. Dent._ 48, 258–267 (2023). Article CAS PubMed Google Scholar * Abdullah, Z. & John, J. Minimally Invasive Treatment of White Spot Lesions-A Systematic Review. _Oral Health
Prev. Dent._ 14, (2016). * Paula, A. B. P. et al. Therapies for white spot lesions—A systematic review. _J. Evid.-Based Dent. Pr._ 17, 23–38 (2017). * Lopatiene, K., Borisovaite, M. &
Lapenaite, E. Prevention and treatment of white spot lesions during and after treatment with fixed orthodontic appliances: a systematic literature review. _Int. J. Oral Max. Surg._ 7,
(2016). * Akin, M. & Basciftci, F. A. Can white spot lesions be treated effectively? _Angle Orthod._ 82, 770–775 (2012). * Philip, N. State of the Art Enamel Remineralization Systems:
The Next Frontier in Caries Management. _Caries Res._ 53, 284–295 (2018). Article PubMed Google Scholar * Cochrane, N., Cai, F., Huq, N., Burrow, M. & Reynolds, E. New approaches to
enhanced remineralization of tooth enamel. _J. Dent. Res._ 89, 1187–1197 (2010). Article CAS PubMed Google Scholar * Fredrick, C., Krithikadatta, J., Abarajithan, M. & Kandaswamy, D.
Remineralisation of Occlusal White Spot Lesions with a Combination of 10% CPP-ACP and 0.2% Sodium Fluoride Evaluated Using Diagnodent: A Pilot Study. _Oral Hlth. Prev. Dent._ 11, (2013). *
Ismail, A. I. et al. Caries management pathways preserve dental tissues and promote oral health. _Community Dent. Oral._ 41, e12–e40 (2013). * Dai, Z. et al. Novel nanostructured resin
infiltrant containing calcium phosphate nanoparticles to prevent enamel white spot lesions. _J. Mech. Behav. Biomed. Mater._ 126, 104990 (2022). Article CAS PubMed Google Scholar
Download references ACKNOWLEDGEMENTS This work has been funded with National Key R&D Program of China (2022YFC2405904); National Natural Science Foundation of China (11932012, and
32171348). AUTHOR INFORMATION Author notes * These authors contributed equally: Lunguo Xia, Chenchen Zhou, Peng Mei. AUTHORS AND AFFILIATIONS * Department of Orthodontics, Shanghai Ninth
People’s Hospital, Shanghai Jiao Tong University School of Medicine, College of Stomatology, Shanghai Jiao Tong University, National Center for Stomatology, National Clinical Research Center
for Oral Diseases, Shanghai Key Laboratory of Stomatology, Shanghai Research Institute of Stomatology, Shanghai, China Lunguo Xia, Peng Mei & Bing Fang * State Key Laboratory of Oral
Diseases & National Clinical Research Center for Oral Diseases & Department of Pediatric Dentistry, West China Hospital of Stomatology, Sichuan University, Chengdu, China Chenchen
Zhou * State Key Laboratory of Military Stomatology, National Clinical Research Center for Oral Diseases, Shaanxi Clinical Research Center for Oral Diseases, Department of Orthodontics,
School of Stomatology, Air Force Medical University, Xi’an, China Zuolin Jin * Department of Orthodontics, Hubei-MOST KLOS and KLOBM, School & Hospital of Stomatology, Wuhan University,
Wuhan, China Hong He * Department of Orthodontics, Affiliated Stomatological Hospital of Nanjing Medical University, Jiangsu Province Key Laboratory of Oral Diseases, Nanjing, China Lin Wang
* Department of Orthodontics, Capital Medical University School of Stomatology, Beijing, China Yuxing Bai * Department of Stomatology, Union Hospital, Tongji Medical College, Huazhong
University of Science and Technology, School of Stomatology, Tongji Medical College, Huazhong University of Science and Technology, Hubei Province Key Laboratory of Oral and Maxillofacial
Development and Regeneration, Wuhan, China Lili Chen * Department of Orthodontics, Peking University School and Hospital of Stomatology, National Center of Stomatology, National Clinical
Research Center for Oral Diseases, National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing Key Laboratory of Digital Stomatology, Beijing, China Weiran
Li * State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases & Department of Orthodontics, West China Hospital of Stomatology, Sichuan
University, Chengdu, China Jun Wang * Department of Orthodontics, Hospital of Stomatology, Jilin University, Changchun, China Min Hu * Department of Orthodontics, Stomatological Hospital of
Chongqing Medical University, Chongqing Key Laboratory of Oral Diseases and Biomedical Sciences, Chongqing Municipal Key Laboratory of Oral Biomedical Engineering of Higher Education,
Chongqing, China Jinlin Song * Department of Orthodontics, Hospital of Stomatology, Guanghua School of Stomatology, Sun Yat-sen University, Guangdong Provincial Key Laboratory of
Stomatology, Guangzhou, China Yang Cao * Department of Orthodontics, Shanghai Stomatological Hospital, Shanghai Key Laboratory of Craniomaxillofacial Development and Diseases, Fudan
University, Shanghai, China Yuehua Liu * Center for Microscope Enhanced Dentistry, Capital Medical University School of Stomatology, Beijing, China Benxiang Hou * Department of Operative
Dentistry and Endodontics, Hospital of Stomatology, Guanghua School of Stomatology, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Stomatology, Guangzhou, China Xi Wei *
Department of Prosthodontics, School of Stomatology, Air Force Medical University, State Key Laboratory of Oral & Maxillofacial Reconstruction and Regeneration, National Clinical
Research Center for Oral Diseases, Shaanxi Key Laboratory of Stomatology, Xi’an, China Lina Niu * Department of Preventive Dentistry, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong
University School of Medicine, College of Stomatology, Shanghai Jiao Tong University, National Center of Stomatology, National Clinical Research Center for Oral Diseases, Shanghai Key
Laboratory of Stomatology, Shanghai Research Institute of Stomatology, Shanghai, China Haixia Lu * Tianjin Stomatological Hospital, School of Medicine, Nankai University, Tianjin Key
Laboratory of Oral and Maxillofacial Function Reconstruction, Tianjin, China Wensheng Ma * Department of Orthodontics, School of Stomatology, Harbin Medical University, the Second Affiliated
Hospital of Harbin Medical University, Harbin, China Peijun Wang * Department of Orthodontics, Shenyang Stomatological Hospital, Shenyang, China Guirong Zhang * Department of Orthodontics,
School and Hospital of Stomatology, Shandong University, Jinan, China Jie Guo * Department of Orthodontics, Affiliated Stomatological Hospital of Nanchang University, Jiangxi Provincial Key
Laboratory of Oral Biomedicine, Nanchang, China Zhihua Li * Department of Orthodontics, School and Hospital of Stomatology, Hebei Medical University, Hebei Provincial Key Laboratory of
Stomatology, Hebei Provincial Clinical Research Center for Oral Diseases, Shijiazhuang, China Haiyan Lu * School of Stomatology, Lanzhou University, Lanzhou, China Liling Ren * Department of
Orthodontics, Fujian Key Laboratory of Oral Diseases, Stomatological Key Lab of Fujian College and University, School and Hospital of Stomatology, Fujian Medical University, Fuzhou, China
Linyu Xu * Department of Orthodontics, School and Hospital of Stomatology, Shanxi Medical University, Shanxi Province Key Laboratory of Oral Diseases Prevention and New Materials, Taiyuan,
China Xiuping Wu * Department of Orthodontics, Xiangya Stomatology Hospital, Central South University, Changsha, China Yanqin Lu * Department of Orthodontics, Affiliated Stomatological
Hospital of Kunming Medical University, Kunming, China Jiangtian Hu * Department of Cariology and Endodontology, Peking University School and Hospital of Stomatology, National Center for
Stomatology, National Clinical Research Center for Oral Diseases, National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing Key Laboratory of Digital
Stomatology, Beijing, China Lin Yue * School and Hospital of Stomatology, Institute of Stomatology, Tianjin Medical University, Tianjin Key Laboratory of Oral Soft and Hard Tissues
Restoration and Regeneration, Tianjin, China Xu Zhang Authors * Lunguo Xia View author publications You can also search for this author inPubMed Google Scholar * Chenchen Zhou View author
publications You can also search for this author inPubMed Google Scholar * Peng Mei View author publications You can also search for this author inPubMed Google Scholar * Zuolin Jin View
author publications You can also search for this author inPubMed Google Scholar * Hong He View author publications You can also search for this author inPubMed Google Scholar * Lin Wang View
author publications You can also search for this author inPubMed Google Scholar * Yuxing Bai View author publications You can also search for this author inPubMed Google Scholar * Lili Chen
View author publications You can also search for this author inPubMed Google Scholar * Weiran Li View author publications You can also search for this author inPubMed Google Scholar * Jun
Wang View author publications You can also search for this author inPubMed Google Scholar * Min Hu View author publications You can also search for this author inPubMed Google Scholar *
Jinlin Song View author publications You can also search for this author inPubMed Google Scholar * Yang Cao View author publications You can also search for this author inPubMed Google
Scholar * Yuehua Liu View author publications You can also search for this author inPubMed Google Scholar * Benxiang Hou View author publications You can also search for this author inPubMed
Google Scholar * Xi Wei View author publications You can also search for this author inPubMed Google Scholar * Lina Niu View author publications You can also search for this author inPubMed
Google Scholar * Haixia Lu View author publications You can also search for this author inPubMed Google Scholar * Wensheng Ma View author publications You can also search for this author
inPubMed Google Scholar * Peijun Wang View author publications You can also search for this author inPubMed Google Scholar * Guirong Zhang View author publications You can also search for
this author inPubMed Google Scholar * Jie Guo View author publications You can also search for this author inPubMed Google Scholar * Zhihua Li View author publications You can also search
for this author inPubMed Google Scholar * Haiyan Lu View author publications You can also search for this author inPubMed Google Scholar * Liling Ren View author publications You can also
search for this author inPubMed Google Scholar * Linyu Xu View author publications You can also search for this author inPubMed Google Scholar * Xiuping Wu View author publications You can
also search for this author inPubMed Google Scholar * Yanqin Lu View author publications You can also search for this author inPubMed Google Scholar * Jiangtian Hu View author publications
You can also search for this author inPubMed Google Scholar * Lin Yue View author publications You can also search for this author inPubMed Google Scholar * Xu Zhang View author publications
You can also search for this author inPubMed Google Scholar * Bing Fang View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Conceptualization
and investigation: B.F., X.Z. and L.Y.; Supervision: B.F., X.Z. and L.Y.; Original draft: L.X., C.Z. and P.M.; Review and editing: Z.J., H.H., L.W., Y.B., L.C., W.L., J.W., M.H., J.S., Y.C.,
Y.L., B.H., X.W., L.N., H.L., W.M., P.W., G.Z., J.G., Z.L., H.L., L.R., L.X., X.W., Y.L. and J.H. CORRESPONDING AUTHORS Correspondence to Lin Yue, Xu Zhang or Bing Fang. ETHICS DECLARATIONS
COMPETING INTERESTS The authors declare no competing interests. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License,
which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link
to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or
exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints
and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Xia, L., Zhou, C., Mei, P. _et al._ Expert consensus on the prevention and treatment of enamel demineralization in orthodontic treatment.
_Int J Oral Sci_ 17, 13 (2025). https://doi.org/10.1038/s41368-024-00335-7 Download citation * Received: 19 June 2024 * Revised: 25 September 2024 * Accepted: 22 October 2024 * Published:
01 March 2025 * DOI: https://doi.org/10.1038/s41368-024-00335-7 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
Trending News
Real madrid will call tottenham boss mauricio pochettino - balagueZidane resigned as head coach of Real Madrid just days after leading the Spanish club to a third straight Champions Leag...
Were team gb’s skeleton suits responsible for fantastic three medal haul?Team GB skeleton rider Lizzie Yarnold won a stunning Winter Olympic gold on February 17, backed up by bronzes for Laura ...
Ski stations in pyrénées close early due to lack of snowMAJOR RESORT SHUT DOORS TWO WEEKS EARLY AS RAIN AND STORMS MADE IT TOO DANGEROUS TO SKI A ski station in the Pyrénées ha...
9/11 first responder pays it forward with relief missionsMemorial Day Sale! Join AARP for just $11 per year with a 5-year membership Join now and get a FREE gift. Expires 6/4 G...
Comment: weeds can make a garden cheaper and more manageable in franceCOLUMNIST SAMANTHA DAVID TELLS HOW EMBRACING NATURE HAS HIDDEN BENEFITS The day after I moved into my French farmhouse, ...
Latests News
Expert consensus on the prevention and treatment of enamel demineralization in orthodontic treatmentABSTRACTS Enamel demineralization, the formation of white spot lesions, is a common issue in clinical orthodontic treatm...
10 things you probably didn’t know about eddie jones - ruckIT’S TWO YEARS TO THE DAY SINCE EDDIE JONES WAS APPOINTED ENGLAND HEAD COACH, AND HE HAS SINCE WON BACK-TO-BACK SIX NATI...
Muller critical of bayern display despite cup progressionBayern Munich's progression to the DFB-Pokal final brought mixed emotions for match-winner Thomas Muller, who felt ...
Covid’s future: mini-waves rather than seasonal surges* NEWS * 01 May 2023 * Correction 04 May 2023 Three years after the start of the pandemic, SARS-CoV-2 shows no signs of ...
Australia’s consumer laws still don’t cover e-books and many other digital productsAustralia’s consumer laws aren’t adequately protecting Australians who buy digital products such as e-books and digital ...