Renal cancer and pneumothorax risk in birt–hogg–dubé syndrome; an analysis of 115 flcn mutation carriers from 35 bhd families
Renal cancer and pneumothorax risk in birt–hogg–dubé syndrome; an analysis of 115 flcn mutation carriers from 35 bhd families"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT BACKGROUND: Birt–Hogg–Dubé (BHD) syndrome is an autosomal dominant condition caused by germline _FLCN_ mutations, and characterised by fibrofolliculomas, pneumothorax and renal
cancer. The renal cancer risk, cancer phenotype and pneumothorax risk of BHD have not yet been fully clarified. The main focus of this study was to assess the risk of renal cancer, the
histological subtypes of renal tumours and the pneumothorax risk in BHD. METHODS: In this study we present the clinical data of 115 _FLCN_ mutation carriers from 35 BHD families. RESULTS:
Among 14 _FLCN_ mutation carriers who developed renal cancer 7 were <50 years at onset and/or had multifocal/bilateral tumours. Five symptomatic patients developed metastatic disease. Two
early-stage cases were diagnosed by surveillance. The majority of tumours showed characteristics of both eosinophilic variants of clear cell and chromophobe carcinoma. The estimated
penetrance for renal cancer and pneumothorax was 16% (95% minimal confidence interval: 6–26%) and 29% (95% minimal confidence interval: 9–49%) at 70 years of age, respectively. The most
frequent diagnosis in families without identified _FLCN_ mutations was familial multiple discoid fibromas. CONCLUSION: We confirmed a high yield of _FLCN_ mutations in clinically defined BHD
families, we found a substantially increased lifetime risk of renal cancer of 16% for _FLCN_ mutation carriers. The tumours were metastatic in 5 out of 14 patients and tumour histology was
not specific for BHD. We found a pneumothorax risk of 29%. We discuss the implications of our findings for diagnosis and management of BHD. SIMILAR CONTENT BEING VIEWED BY OTHERS A
SYSTEMATIC REVIEW ASSESSING THE EXISTENCE OF PNEUMOTHORAX-ONLY VARIANTS OF _FLCN_. IMPLICATIONS FOR LIFELONG SURVEILLANCE OF RENAL TUMOURS Article Open access 15 July 2021 ERN GENTURIS
CLINICAL PRACTICE GUIDELINES FOR THE DIAGNOSIS, SURVEILLANCE AND MANAGEMENT OF PEOPLE WITH BIRT-HOGG-DUBÉ SYNDROME Article Open access 31 July 2024 CHARACTERISTICS, AETIOLOGY AND
IMPLICATIONS FOR MANAGEMENT OF MULTIPLE PRIMARY RENAL TUMOURS: A SYSTEMATIC REVIEW Article Open access 27 May 2024 MAIN Birt–Hogg–Dubé syndrome (BHD, OMIM #135150) is an autosomal dominant
condition characterised by fibrofolliculomas, pneumothorax and renal tumours. BHD is caused by germline mutations in the _FLCN_ gene encoding folliculin (Nickerson et al, 2002). In the
original kindred skin lesions were the only clinical manifestation (Birt et al, 1977). Subsequently, renal cancer and pneumothorax were found to be part of the syndrome (Roth et al, 1993;
Toro et al, 1999). Furthermore, the risk for colorectal cancer might be slightly increased in _FLCN_ mutation carriers (Nahorski et al, 2010). The functions of folliculin have partly been
clarified and might include a role in the mammalian target of rapamycin pathway (Hasumi et al, 2009). Although many BHD kindreds exhibit all three components of the syndrome,
‘pneumothorax-only’ and ‘renal-cancer-only’ families have also been described (Graham et al, 2005; Painter et al, 2005; Woodward et al, 2008; Kunogi et al, 2010). Among 69 patients with
early-onset or familial clear cell renal cancer without further characteristics of BHD, germline _FLCN_ mutations were found in 4% of cases (Woodward _et al_, 2008). In recent reviews, the
variable clinical manifestations, molecular pathogenesis and management options for BHD were summarised (Schmidt et al, 2005; Toro et al, 2008; Menko et al, 2009). For optimal early
detection and treatment of BHD-associated renal cancer, insight into the renal cancer risk and the clinical picture of these tumours is essential. Among cohorts of BHD patients a wide range
of prevalence of kidney tumours has been observed, ranging from 6.5 to 34% (Toro _et al_, 2008). The differences in prevalence are probably due to ascertainment in dermatological _vs_
urological clinics and age at examination. Notably, the lifetime renal cancer risk for _FLCN_ mutation carriers has not yet been established. In BHD, renal cancer is generally diagnosed at a
relatively young age and commonly presents as bilateral and/or multifocal disease. The renal neoplasms typically found in BHD patients were described as hybrid tumours, containing elements
of different histological subtypes, in particular chromophobe tumours and oncocytoma. However, other subtypes including clear cell renal carcinoma have also been reported (Pavlovich et al,
2002, 2005; Schmidt et al, 2005; Woodward _et al_, 2008). A 50-fold increased risk of spontaneous pneumothorax in BHD was reported (Zbar et al, 2002). Among cohorts of BHD patients the
prevalence of pneumothorax ranged from 24 to 38% (Schmidt et al, 2005; Toro et al, 2007, 2008). Again, ascertainment has varied for cohorts of patients and the lifetime risk of pneumothorax
for _FLCN_ mutation carriers has not yet been established. On CT examination of the thorax, more than 80% of adult BHD patients had multiple lung cysts, most often in the basal lung regions.
The presence of lung cysts is probably related to the increased risk for pneumothorax, which is often recurrent in BHD patients (Toro et al, 2007). A positive family history for
pneumothorax was associated with an increased risk of pneumothorax and patients with a family history positive for renal cancer had an increased risk of having renal tumours. However, a
family history of renal cancer was not associated with an increased pneumothorax risk (Toro et al, 2008). Previously, we described 25 _FLCN_ germline mutation carriers from 11 BHD families
(Leter et al, 2008). Here, we present an update of this cohort and add the evaluation of 24 new kindreds with pathogenic _FLCN_ mutations. In total, the clinical histories of 115 _FLCN_
mutation carriers from 35 BHD families have been assessed. The main focus of this study was to assess the risk of renal cancer, the histological subtypes of renal tumours and the
pneumothorax risk in BHD. Furthermore, we consider the yield of _FLCN_ mutation analysis and the clinical phenotype in kindreds without _FLCN_ mutations. PATIENTS AND METHODS ASCERTAINMENT
OF PEDIGREES The BHD database at VU University Medical Center currently lists more than 65 Dutch families referred for suspected BHD; 53 of these kindreds with completed family studies are
considered in this report. In all, 40 of these 53 families were referred to our center, whereas other Dutch clinical genetics centers contributed an additional 13 families with pathogenic
_FLCN_ mutations (Table 1). The index patient of 48 out of the 53 families was referred by a dermatologist after fibrofolliculomas were diagnosed. In three BHD families the index patient had
renal cancer (BHD families 33, 35 and 63), in one kindred the proband had recurrent pneumothorax (BHD 29). One patient without an identifiable _FLCN_ mutation was referred for multiple
pulmonary cysts. For ascertainment of pedigrees, the proband was requested to inform family members by means of a written summary letter about BHD. After completion of the initial evaluation
reminders were sent to probands aimed at complete ascertainment of family members. MUTATION ANALYSIS After informed consent genomic DNA was extracted from blood samples. Primers for the
amplification and sequencing of the 14 exons were detailed previously by Nickerson et al (2002). PCR amplification was performed using a PE 9700 thermocycler (Applied Biosystems, Forster
City, CA, USA). Sequencing reactions were performed using Big Dye Terminator (Applied Biosystems) and run on an ABI 3100 genetic analyzer (Applied Biosystems). For the detection of deletions
and duplications of one or more exons the SALSA MLPA kit P256 obtained from MRC Holland was used (http://www.mrc-holland.com). STATISTICAL ANALYSIS Conditional on the mutation status for
different individuals, we assumed the various expressions of the BHD phenotype to be mutually independent and that for individual cases the risks for renal cancer and pneumothorax and the
ages at which these traits were expressed are independent. Finally, the penetrances of renal cancer and pneumothorax were assumed to be equal for male and female mutation carriers. For the
estimates of the penetrance of pneumothorax and renal cancer we included 21 out of 22 _FLCN_-positive pedigrees investigated at our center. For these families medical records of all mutation
carriers and information on untested relatives were available. Out of these 21 pedigrees, 20 were ascertained via a proband referred by a dermatologist. One proband (BHD 29) was referred by
a pulmonologist for analysis of recurrent pneumothorax. Therefore, we included the proband data in the estimation of renal cancer and pneumothorax risks, with the exception of the proband
referred for analysis of pneumothorax. Major problems of penetrance estimates are missing data and possible preferential testing of individuals affected with complications of BHD, that is,
renal cancer or pneumothorax. Indeed, if the mutation status and phenotype had been known for all individuals in all pedigrees the penetrance curves could have been assessed using the
Kaplan–Meier estimator. Unfortunately, however, the mutation status or phenotype was not known for all family members. Excluding the individuals for whom the mutation status was unknown
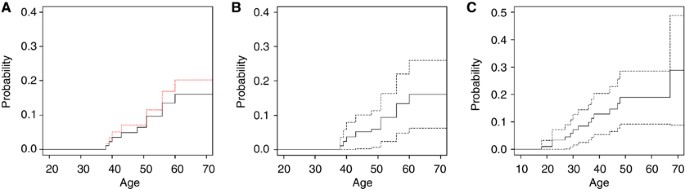
would likely lead to an overestimation of risk (see Figure 1A), assuming that non-affected individuals may be less willing to be genotyped. For our corrected risk estimation we assumed that
a negative family history for renal cancer or pneumothorax in a close relative indeed reflects the absence of these complications in the untested relative. We imputed the missing data as
follows: for every individual in the data set who was not genotyped the probability that he or she was a carrier was computed on the basis of the mutation status of his/her relatives.
Subsequently, using this carrier probability it was sampled whether he or she was a mutation carrier or not. As a result, for every individual the mutation status was assigned and in
combination with the phenotype Kaplan–Meier curves and confidence intervals were computed. This strategy of sampling the mutation status and estimating the penetrance functions by the
Kaplan–Meier estimator was repeated 10 000 times. Next, the mean of the 10 000 estimated curves and upper and lower bounds of the confidence intervals were computed. These curves are plotted
in Figure 1A and B for renal cancer and in Figure 1C for pneumothorax. By using this strategy the estimator will be asymptotically unbiased. The confidence interval found is slightly too
narrow because there is a greater degree of uncertainty than would have been the case if the missing mutation statuses had actually been observed (as assumed after imputation). Therefore,
the final confidence interval has a confidence of slightly less than 95%. Although the exact confidences of the intervals are not exactly known we included the calculated intervals in the
figures in order to make those who would use the figures for consultation aware of the uncertainty of the given risk estimates. RESULTS The characteristics of 53 families referred for
suspected BHD are presented in Table 1. The main features of the BHD kindreds with pathogenic _FLCN g_ermline mutations are listed in Table 2. The mutations detected are depicted in Figure
2. Data on the renal tumours and pneumothorax are given in Tables 3 and 4, respectively. Among the 27 families with clinical BHD based on dermatological evaluation at our center, 22 had
pathogenic _FLCN_ mutations (mutation detection rate 81%). Characteristics of the five families without a detectable _FLCN_ mutation are summarised in Table 5; they include two families with
an unclassified exon 1 deletion. Analysis of these exon 1 deletions is ongoing. In the cohort of our current study, no colorectal cancer was reported. Colorectal adenomas were diagnosed by
colonoscopy in four _FLCN_ mutation carriers (age 40, 42, 83, these patients were also included in our previous reports by Leter et al, 2008 and Nahorski et al, 2010 and age 44, not reported
previously). Other malignancies than renal cancer were reported in six patients previously documented in Leter et al (2008). In addition to the patients reported by Leter et al (2008) in
five patients without renal cancer, tumours were reported including non-melanoma skin cancer in two patients and single cases of melanoma, sarcoma, bladder and prostate cancer. The patient
diagnosed with melanoma was also diagnosed with sarcoma. Three patients with renal cancer were diagnosed with additional tumours. One patient had oncocytic pituitary adenoma at age 9,
astrocytoma at age 12, pheochromocytoma at age 34 and renal cancer at age 34 and 35 (BHD 63, Table 3). No evidence for other tumour susceptibility was found. The other two patients had
gastric carcinoma at age 55 and renal cancer at age 56 (BHD 43, M, Table 3) and prostate carcinoma and renal cancer at age 50 (BHD 46, Table 3), respectively. RENAL MANIFESTATIONS In all, 14
out of 115 (12%) _FLCN_ mutation carriers from 12 families were diagnosed with renal cancer. All available tumours were revised at our center by two pathologists. In addition, one mutation
carrier had renal oncocytoma (BHD 57). Five mutation carriers died of metastatic renal cancer (BHD 6, BHD 16, BHD 23, BHD 37 and BHD 44; Table 3). All were diagnosed with renal cancer after
symptoms had developed. The histological classification of the renal tumours according to the WHO criteria is shown in Table 3 (Lopez-Beltran et al, 2009). Most of the tumours showed cells
with granular/floccular eosinophilic cytoplasm, as can be seen in both clear cell carcinoma (formerly called the eosinophilic variant, Table 3) and chromophobe carcinoma. This eosinophilic
cell variation is also often seen in sporadic clear cell carcinoma (Kummerlin et al, 2009; Lopez-Beltran et al, 2009). As most tumours had mainly eosinophilic cytoplasm, with moderately
sharp cell borders, a vague perinuclear halo and moderately enlarged nuclei, we classified them as intermediate between clear cell and chromophobe carcinoma (CC/Cph) (Table 3 and Figure 3).
One of the tumours showed sarcomatoid changes, which can develop in both clear cell and chromophobe carcinoma (Table 3, BHD 16). One other tumour had papillary structures in combination with
clear cell changes (Table 3, BHD 6). Two additional patients from _FLCN_ positive families but with unknown mutation carrier status (BHD 1 and BHD 42) were diagnosed with renal cancer.
These two tumours also showed mixed chromophobe/clear cell histology. In all, 2 of the 14 renal tumours (BHD 1 and BHD 32, Table 3) were detected by surveillance. For one of these patients
renal cancer was detected on the first ultrasound performed after the diagnosis BHD was made (BHD 32, Table 3). For the other patient renal cancer was detected by ultrasound 4 years after
the preceding normal ultrasound/MRI (BHD 1, Table 3); the latter patient did not undergo standard yearly surveillance after the initial imaging. CUTANEOUS MANIFESTATIONS Most _FLCN_ mutation
carriers (91/115, 79%), underwent dermatological evaluation (68 of which were evaluated by dermatologists at our center). In all 19 (21%) cases, aged 23–72 years, had no cutaneous
abnormalities; 14 (74%) of the patients without cutaneous manifestations were over age 40. Notably, one patient who presented with metastatic renal cancer at age 51 (BHD 23) had no cutaneous
lesions. The youngest mutation carrier with histologically confirmed fibrofolliculomas was 25 years old (BHD 23). In five families without an identifiable _FLCN_ mutation (BHD 2, 5, 9, 25
and 28) the clinical diagnosis BHD was based on histologically confirmed multiple fibrofolliculomas; in one of these kindreds both pneumothorax and renal cancer occurred (BHD 25, Table 5).
In seven families without _FLCN_ mutations the skin lesions consisted of multiple discoid fibromas of childhood onset (families 11, 17, 20, 24, 38, 45 and 50). In two of these families (24
and 45) a genealogical study showed common ancestry. No renal or pulmonary signs were present in these seven families, except for one case with pneumothorax. For two of these families the
_FLCN_-locus was excluded by linkage analysis (Starink et al, 2011). PULMONARY MANIFESTATIONS Among the 115 _FLCN_ mutation carriers, 28 (24%) had a history of pneumothorax, recurrent in
eight patients (Table 4). In all, 4 out of 28 patients with a previous pneumothorax were confirmed (former) smokers. The medical records of the other patients did not state a history of
smoking. The mean age of the first pneumothorax was 36 years (range 18–74 years). We did not systematically subject mutation carriers to CT scanning of the lungs. For 12 _FLCN_ mutation
carriers the report of a CT-scan of the thorax was available. Scans were performed either to confirm suspected BHD or because of pulmonary complications of BHD. In five of these patients
(aged 25–46 years), multiple cysts were reported in one or both lungs. Of these, two had a history of recurrent or bilateral pneumothorax before the age of 30 years. In seven _FLCN_ mutation
carriers no pulmonary cysts were detected (age 23–71, four were over age 40). CUMULATIVE RENAL CANCER AND PNEUMOTHORAX RISK The estimated renal cancer penetrance based on assessment of
_FLCN_ mutation carriers only was 20% at age 70 (red dashed line, Figure 1A). In contrast, when considering both tested and untested relatives, the estimated renal cancer penetrance at age
70 was 16% (continuous line, Figure 1A and B). The estimated penetrance for the first episode of spontaneous pneumothorax was 29% (95% minimal confidence interval: 9–49%, Figure 1C) at 70
years, again considering information on both mutation carriers and their untested relatives. DISCUSSION An important aim of this study was the estimation of renal cancer and pneumothorax
penetrance in BHD. By incorporating data on relatives who did not undergo DNA testing we found an estimated penetrance for renal cancer of 16% and a penetrance for pneumothorax of 29% at the
age of 70 years. The wide range of prevalence for renal cancer among cohorts of BHD reported in literature is 6.5–34% (Toro et al, 2007, 2008; Kunogi et al, 2010). The renal cancer risk we
found of around 16% at age 70 years is important for counselling of _FLCN_ mutation carriers and their families ascertained in cancer family clinics. Future studies with larger patient
groups and comparison between cohorts investigated in different populations may lead to further specification of the renal cancer risk. The clinical presentation, histological pattern and
biological behaviour of renal cancer in _FLCN_ mutation carriers are important for several reasons. First, a pathognomonic histological pattern would be helpful for early diagnosis.
Previously, The European BHD Consortium proposed clinical diagnostic criteria for BHD, which included early-onset, bilateral and multifocal renal tumours and a mixed chromophobe and
oncocytic histological pattern. In addition, _FLCN_ mutation analysis should be considered for patients who have familial cystic lung disease, familial pneumothorax, familial renal cancer,
or any combination of spontaneous pneumothorax and kidney cancer (Menko _et al_, 2009). Notably, among 14 BHD patients in the current study who developed renal cancer, clinical signs of
hereditary disease (age at onset <50 years and/or multifocal/bilateral tumours) were present in only seven cases. In addition, the histological picture of BHD-associated renal cancer in
this cohort was not typical for this syndrome. In all, 10 out of 14 renal tumours revised in this series were difficult to classify. None of them showed classical features of chromophobe
renal cell carcinoma. Instead, they mainly exhibited characteristics of both eosinophilic variants of clear cell cancer and chromophobe carcinoma. One of the tumours was a hybrid form of
clear cell and papillary carcinoma and one showed sarcomatoid changes. These histological patterns can also be found in sporadic RCC. Therefore, late-onset unilateral, unifocal clear cell
renal cancer does not exclude BHD. Furthermore, although BHD-associated renal tumours were reported to metastasise rarely (Toro _et al_, 2008), 5 of the 14 patients with renal cancer in our
cohort developed metastatic disease underlining the importance of early detection of these renal tumours by surveillance. In recently diagnosed families not included in this report, we
observed two BHD patients with renal cancer at the ages of 30 and in the early twenties, respectively, underlining that surveillance for renal cancer should be offered to BHD patients from
early age onward. Of the 115 _FLCN_ mutation carriers 28 had a history of pneumothorax, frequently recurrent and bilateral. The mean ages at which pneumothorax and renal cancer occurred in
our cohort were 36 and 49 years, respectively. Among the 14 renal cancer patients described five had a history of pneumothorax (Tables 3 and (4), preceding renal cancer by several years in
three patients (BHD 32, 37, 43, Table 4). Although an increased risk for renal cancer in BHD families with a positive history for pneumothorax has not been observed (Toro _et al_, 2008),
bilateral, recurrent or familial pneumothorax may serve as an early indicator of BHD syndrome (Johannesma et al, 2009). Ever since Hornstein and Knickenberg (1975) described the combination
of skin fibrofolliculomas and colorectal polyps it is a matter of debate whether BHD is associated with an increased risk of colorectal neoplasia. Although Zbar et al (2002) found no
significantly increased risk Khoo et al (2002) proposed that the risk might apply to specific subgroups only. Nahorski et al (2010) found evidence that the risk may be dependent on the
_FLCN_ genotype. Recently, in family BHD15, one of the _FLCN_ mutation carriers developed symptomatic colonic cancer at age 62 years. Late-onset colorectal cancer has been diagnosed in
several other _FLCN_ mutation carriers from our BHD cohort not included in the present study. Although colorectal cancer may well be coincidental in these cases the current data call for
further evaluation of the colorectal neoplasia risk in BHD. Among 27 families with clinical BHD (multiple fibrofolliculomas) evaluated at our center 22 had pathogenic _FLCN_ mutations,
resulting in a 81% yield for _FLCN_ mutation analysis. Four patients referred for suspected BHD declined genetic testing. In two of the families (BHD 2 and 25) with clinical BHD but without
a mutation in the coding region of _FLCN_, a deletion of exon 1 was observed. Exon 1 is the first of three non-coding exons. The exact size and the effect of these deletions remain to be
determined. Recently, after completion of our study, intragenic deletions and a duplication were reported in patients with BHD (Benhammou et al, 2011). Using a luciferase reporter assay,
this study also showed that the expression was strongly reduced when exon 1 was deleted. Analysis of the pathogenicity and co-segregation of the deletions detected in our families are
currently ongoing to prove pathogenicity. Therefore, these families were not included in the calculation of the penetrance for renal cancer and pneumothorax, although the deletions are very
likely to be pathogenic. In the current study, intragenic deletions were detected in two additional BHD families (BHD 57, 62), underlining the importance of MLPA or CGH analysis in patients
with a clinical suspicion of BHD without an identifiable _FLCN_ mutation. Nine patients referred for possible BHD were diagnosed with other conditions. One patient had probable tuberous
sclerosis and one patient had pulmonary emphysema. Seven of the families were diagnosed with familial multiple discoid fibromas (FMDF). In 1985, one of the authors described this entity as a
dominant condition distinct from BHD, showing childhood onset, preferential localisation of lesions on the ears and distinct histology, which mimics the trichodiscomas in BHD (Starink et
al, 1985). Thus far no systemic complications have been noted for FMDF except for one patient with pneumothorax. We have now excluded involvement of the _FLCN_ locus in two FMDF kindreds
using linkage analysis (Starink et al, 2011). Currently, we use the renal cancer risk of around 16% by age 70 years for the counselling of patients to emphasise the importance of
surveillance for renal cancer. As according to our histological data, the renal cancers found in BHD were not evidently different from sporadic tumours, future studies aimed at the
classification of BHD-associated renal cancer in comparison with sporadic disease are essential. Both the renal cancer risk and the pneumothorax risk (about 16% and 29% at age 70 years,
respectively) are based on a large set of data using a model incorporating available data of family members not subjected to DNA testing. Evaluation of larger patient groups and patients
from other populations may yield other penetrance figures in the future. The European BHD Consortium (Menko et al, 2009) proposed _FLCN_ mutation testing in patients with early-onset renal
cancer (<50 years), in particular with multifocal or bilateral disease (or both) with chromophobe or oncocytic histology and in familial renal cancer cases. Age at diagnosis of (the
first) renal cancer in our patient group was at or above 50 years of age in half of the patients and the tumour histology was mixed in most patients but included clear cell elements in all
cases. Therefore, it will be important to study the yield of _FLCN_ mutation testing using a wider set of criteria than proposed previously. The histology and molecular pathology of renal
tumours are associated with their biological behaviour and reaction to systemic treatment of metastatic disease. Therefore, additional studies are needed to monitor the success of
surveillance for renal cancer, the results of surgical or other forms of local treatment such as radiofrequency ablation and response to targeted therapies. CHANGE HISTORY * _ 29 MARCH 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication _ REFERENCES * Benhammou JN, Vocke CD, Santani A, Schmidt LS,
Baba M, Seyama K, Wu X, Korolevich S, Nathanson KL, Stolle CA, Linehan WM (2011) Identification of intragenic deletions and duplication in the _FLCN_ gene in Birt-Hogg-Dubé syndrome. _Genes
Chromosomes Cancer_ 50 (6): 466–477 Article CAS PubMed PubMed Central Google Scholar * Birt AR, Hogg GR, Dubé WJ (1977) Hereditary multiple fibrofolliculomas with trichodiscomas and
acrochordons. _Arch Dermatol_ 113 (12): 1674–1677 Article CAS PubMed Google Scholar * Gatalica Z, Lilleberg SL, Vranic S, Eyzaguirre E, Orihuela E, Velagaleti G (2009) Novel intronic
germline _FLCN_ gene mutation in a patient with multiple ipsilateral renal neoplasms. _Hum Pathol_ 40 (12): 1813–1819 Article CAS PubMed Google Scholar * Graham RB, Nolasco M, Peterlin
B, Garcia CK (2005) Nonsense mutations in folliculin presenting as isolated familial spontaneous pneumothorax in adults. _Am J Respir Crit Care Med_ 172 (1): 39–44 Article PubMed Google
Scholar * Hasumi Y, Baba M, Ajima R, Hasumi H, Valera VA, Klein ME, Haines DC, Merino MJ, Hong SB, Yamaguchi TP, Schmidt LS, Linehan WM (2009) Homozygous loss of BHD causes early embryonic
lethality and kidney tumor development with activation of mTORC1 and mTORC2. _Proc Natl Acad Sci_ 106 (44): 18722–18727 Article CAS PubMed PubMed Central Google Scholar * Hornstein OP,
Knickenberg M (1975) Perifollicular fibromatosis cutis with polyps of the colon – a cutaneo-intestinal syndrome sui generis. _Arch Dermatol Res_ 253 (2): 161–175 Article CAS PubMed Google
Scholar * Johannesma PC, Lammers JW, van Moorselaar RJ, Starink TM, Postmus PE, Menko FH (2009) Spontaneous pneumothorax as the first manifestation of a hereditary condition with an
increased renal cancer risk. _Ned Tijdschr Geneeskd_ 153: A581 (in Dutch) PubMed Google Scholar * Khoo SK, Giraud S, Kahnoski K, Chen J, Motorna O, Nickolov R, Binet O, Lambert D, Friedel
J, Lévy R, Ferlicot S, Wolkenstein P, Hammel P, Bergerheim U, Hedblad MA, Bradley M, Teh BT, Nordenskjöld M, Richard S (2002) Clinical and genetic studies of Birt-Hogg-Dubé syndrome. _J Med
Genet_ 39 (12): 906–912 Article CAS PubMed PubMed Central Google Scholar * Kummerlin I, ten Kate F, Smedts F, Horn T, Algaba F, Trias I, de la Rosette J, Laguna MP (2009) Diagnostic
problems in the subtyping of renal tumors encountered by five pathologists. _Pathol Res Pract_ 205 (1): 27–34 Article PubMed Google Scholar * Kunogi M, Kurihara M, Ikegami TS, Kobayashi
T, Shindo N, Kumasaka T, Gunji Y, Kikkawa M, Iwakami S, Hino O, Takahashi K, Seyama K (2010) Clinical and genetic spectrum of Birt-Hogg-Dubé syndrome patients in whom pneumothorax and/or
multiple lung cysts are the presenting feature. _J Med Genet_ 47 (4): 281–287 Article CAS PubMed Google Scholar * Leter EM, Koopmans AK, Gille JJP, Van Os TAM, Vittoz GG, David EFL,
Jaspars EH, Postmus PE, van Moorselaar RJA, Craanen ME, Starink TM, Menko FH (2008) Birt-Hogg-Dubé syndrome: clinical and genetic studies of 20 families. _J Invest Dermatol_ 128 (1): 45–49
Article CAS PubMed Google Scholar * Lopez-Beltran A, Carrasco JC, Cheng L, Scarpelli M, Kirkali Z, Montironi R (2009) 2009 update on the classification of renal epithelial tumors in
adults. _Int J Urol_ 16 (5): 432–443 Article PubMed Google Scholar * Menko FH, van Steensel MAM, Giraud S, Friis-Hansen L, Richard S, Ungari S, Nordenskjöld M, Hansen TV, Solly J, Maher
ER (2009) Birt-Hogg-Dubé syndrome: diagnosis and management. _Lancet Oncol_ 10 (12): 1199–1206 Article CAS PubMed Google Scholar * Nahorski M, Lim DHK, Martin L, Gille JP, Mckay K, Rehal
PK, Ploeger HM, van Steensel M, Tomlinson IP, Latif F, Menko FH, Maher ER (2010) Investigation of the Birt-Hogg-Dubé tumour suppressor gene (_FLCN_) in familial and sporadic colorectal
cancer. _J Med Genet_ 47 (6): 385–390 Article CAS PubMed Google Scholar * Nickerson ML, Warren MB, Toro JR, Matrosova V, Glenn G, Turner ML, Duray P, Merino M, Choyke P, Pavlovich CP,
Sharma N, Walther M, Munroe D, Hill R, Maher E, Greenberg C, Lerman MI, Linehan WM, Zbar B, Schmidt LS (2002) Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign
tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. _Cancer Cell_ 2 (2): 157–164 Article CAS PubMed Google Scholar * Painter JN, Tapanainen H, Somer M, Tukiainen P,
Aittomäki K (2005) A 4-bp deletion in the Birt-Hogg-Dubé gene (_FLCN_) causes dominantly inherited spontaneous pneumothorax. _Am J Hum Genet_ 76 (3): 522–527 Article CAS PubMed PubMed
Central Google Scholar * Pavlovich CP, Grubb III RL, Hurley K, Glenn GM, Toro J, Schmidt LS, Torres-Cabala C, Merino MJ, Zbar B, Choyke P, Walther MM, Linehan WM (2005) Evaluation and
management of renal tumors in the Birt-Hogg-Dubé syndrome. _J Urol_ 173 (5): 1482–1486 Article PubMed Google Scholar * Pavlovich CP, Walther MA, Eyler RA, Hewitt SM, Zbar B, Linehan WM,
Merino MJ (2002) Renal tumors in the Birt-Hogg-Dubé syndrome. _Am J Surg Pathol_ 26 (12): 1542–1552 Article PubMed Google Scholar * Roth JS, Rabinowitz AD, Benson M, Grossman ME (1993)
Bilateral renal cell carcinoma in the Birt-Hogg-Dubé syndrome. _J Am Acad Dermatol_ 29 (6): 1055–1056 Article CAS PubMed Google Scholar * Schmidt LS, Nickerson ML, Warren MB, Glenn GM,
Toro JR, Merino MJ, Turner ML, Choyke PL, Sharma N, Peterson J, Morrison P, Maher ER, Walther MM, Zbar B, Linehan WM (2005) Germline _BHD_-mutation spectrum and phenotype analysis of a large
cohort of families with Birt-Hogg-Dubé syndrome. _Am J Hum Genet_ 76 (6): 1023–1033 Article CAS PubMed PubMed Central Google Scholar * Starink TM, Houweling AC, van Doorn MBA, Leter
EM, Jaspars EH, van Moorselaar RJA, Postmus PE, Johannesma PC, van Waesberghe JH, Ploeger MH, Kramer MT, Gille JJP, Waisfisz Q, Menko FH (2011) Familial multiple discoid fibromas: a
look-alike of Birt-Hogg-Dubé syndrome not linked to the _FLCN_ locus. _J Am Acad Dermatol_; doi:10.1016/j.jaad.2010.11.039 (in press) * Starink TM, Kisch LS, Meijer CJLM (1985) Familial
multiple trichodiscomas – a clinicopathologic study. _Arch Dermatol_ 121 (7): 888–891 Article CAS PubMed Google Scholar * Toro JR, Glenn G, Duray P, Darling T, Weirich G, Zbar B, Linehan
M, Turner ML (1999) Birt-Hogg-Dubé syndrome – a novel marker of kidney neoplasia. _Arch Dermatol_ 135 (10): 1195–1202 Article CAS PubMed Google Scholar * Toro JR, Pautler SE, Stewart L,
Glenn GM, Weinreich M, Toure O, Wei MH, Schmidt LS, Davis L, Zbar B, Choyke P, Steinberg SM, Nguyen DM, Linehan WM (2007) Lung cysts, spontaneous pneumothorax, and genetic associations in
89 families with Birt-Hogg-Dubé syndrome. _Am J Respir Crit Care Med_ 175 (10): 1044–1053 Article CAS PubMed PubMed Central Google Scholar * Toro JR, Wei MH, Glenn GM, Weinreich M,
Toure O, Vocke C, Turner M, Choyke P, Merino MJ, Pinto PA, Steinberg SM, Schmidt LS, Linehan WM (2008) _BHD_ mutations, clinical and molecular genetic investigations of Birt-Hogg-Dubé
syndrome: a new series of 50 families and a review of published reports. _J Med Genet_ 45 (6): 321–331 Article CAS PubMed Google Scholar * Woodward ER, Ricketts C, Killick P, Gad S,
Morris MR, Kavalier F, Hodgson SV, Giraud S, Bressac-de Paillerets B, Chapman C, Escudier B, Latif F, Richard S, Maher ER (2008) Familial non-VHL clear cell (conventional) renal cell
carcinoma: clinical features, segregation analysis, and mutation analysis of _FLCN_. _Clin Cancer Res_ 14 (18): 5925–5930 Article CAS PubMed Google Scholar * Zbar B, Alvord WG, Glenn G,
Turner M, Pavlovich CP, Schmidt L, Walther M, Choyke P, Weirich G, Hewitt SM, Duray P, Gabril F, Greenberg C, Merino MJ, Toro J, Linehan WM (2002) Risk of renal and colonic neoplasms and
spontaneous pneumothorax in the Birt-Hogg-Dubé syndrome. _Cancer Epidemiol Biomarkers Prev_ 11 (4): 393–400 PubMed Google Scholar Download references ACKNOWLEDGEMENTS We are grateful for
the comments and suggestions given by Professor Eamonn Maher, Department of Medical and Molecular Genetics, University of Birmingham, United Kingdom and Professor Hanne Meijers, Department
of Clinical Genetics, VU University Medical Center, the Netherlands. We thank Marieke T Kramer and Martijn H Ploeger for their contributions in collecting patient data. LM Geijzen was
supported by the Myrovlytis Trust. MAM van Steensel was supported by a Grant from the Dutch Cancer Society KWF (UM2009-4352). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Clinical Genetics, VU University Medical Center, Amsterdam, PO Box 7057, 1007 MB, The Netherlands A C Houweling, E M Leter, J J P Gille & F H Menko * Department of Dermatology, GROW
School for Oncology and Developmental Biology, Maastricht University Medical Center, Maastricht, The Netherlands L M Gijezen & M A M van Steensel * Department of Mathematics, VU
University, Amsterdam, The Netherlands M A Jonker * Department of Dermatology, VU University Medical Center, The Netherlands M B A van Doorn & T M Starink * Department of Clinical
Genetics, Erasmus University Medical Center, Rotterdam, The Netherlands R A Oldenburg * Department of Genetics, University Medical Center Groningen, University of Groningen, Groningen, The
Netherlands K Y van Spaendonck-Zwarts & M M de Jong * Department of Clinical Genetics, Academic Medical Center, Amsterdam, The Netherlands T A van Os * Department of Pathology, VU
University Medical Center, The Netherlands N C T van Grieken & E H Jaspars * Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands E M H F
Bongers * Department of Pulmonology, VU University Medical Center, the Netherlands P C Johannesma & P E Postmus * Department of Urology, VU University Medical Center, The Netherlands R J
A van Moorselaar * Department of Radiology, VU University Medical Center, The Netherlands J-Htm van Waesberghe Authors * A C Houweling View author publications You can also search for this
author inPubMed Google Scholar * L M Gijezen View author publications You can also search for this author inPubMed Google Scholar * M A Jonker View author publications You can also search
for this author inPubMed Google Scholar * M B A van Doorn View author publications You can also search for this author inPubMed Google Scholar * R A Oldenburg View author publications You
can also search for this author inPubMed Google Scholar * K Y van Spaendonck-Zwarts View author publications You can also search for this author inPubMed Google Scholar * E M Leter View
author publications You can also search for this author inPubMed Google Scholar * T A van Os View author publications You can also search for this author inPubMed Google Scholar * N C T van
Grieken View author publications You can also search for this author inPubMed Google Scholar * E H Jaspars View author publications You can also search for this author inPubMed Google
Scholar * M M de Jong View author publications You can also search for this author inPubMed Google Scholar * E M H F Bongers View author publications You can also search for this author
inPubMed Google Scholar * P C Johannesma View author publications You can also search for this author inPubMed Google Scholar * P E Postmus View author publications You can also search for
this author inPubMed Google Scholar * R J A van Moorselaar View author publications You can also search for this author inPubMed Google Scholar * J-Htm van Waesberghe View author
publications You can also search for this author inPubMed Google Scholar * T M Starink View author publications You can also search for this author inPubMed Google Scholar * M A M van
Steensel View author publications You can also search for this author inPubMed Google Scholar * J J P Gille View author publications You can also search for this author inPubMed Google
Scholar * F H Menko View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to F H Menko. ADDITIONAL INFORMATION This work is
published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons
Attribution-NonCommercial-Share Alike 3.0 Unported License. RIGHTS AND PERMISSIONS From twelve months after its original publication, this work is licensed under the Creative Commons
Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/ Reprints and permissions ABOUT THIS
ARTICLE CITE THIS ARTICLE Houweling, A., Gijezen, L., Jonker, M. _et al._ Renal cancer and pneumothorax risk in Birt–Hogg–Dubé syndrome; an analysis of 115 _FLCN_ mutation carriers from 35
BHD families. _Br J Cancer_ 105, 1912–1919 (2011). https://doi.org/10.1038/bjc.2011.463 Download citation * Received: 23 May 2011 * Revised: 15 September 2011 * Accepted: 10 October 2011 *
Published: 06 December 2011 * Issue Date: 06 December 2011 * DOI: https://doi.org/10.1038/bjc.2011.463 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this
content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
KEYWORDS * Birt–Hogg–Dubé syndrome * folliculin * fibrofolliculoma * renal cancer * discoid fibroma * pneumothorax
Trending News
Chemical burn to the skin: a systematic review of first aid impacts on clinical outcomesBURNS Volume 48, Issue 7, November 2022, Pages 1527-1543 https://doi.org/10.1016/j.burns.2022.05.006Get rights and conte...
Major Talbot Green shooting update as another murder arrest madeMajor Talbot Green shooting update as another murder arrest madeSix people have now been arrested on suspicion of murder...
'kiplinger' lists u. S. Bank as the best bank for retireesMemorial Day Sale! Join AARP for just $11 per year with a 5-year membership Join now and get a FREE gift. Expires 6/4 G...
Page Not Found很抱歉,你所访问的页面已不存在了。如有疑问,请电邮[email protected]你仍然可选择浏览首页或以下栏目内容 :新闻生活娱乐财经体育视频播客新报业媒体有限公司版权所有(公司登记号:202120748H)...
Server Error500 Server Error...
Latests News
Renal cancer and pneumothorax risk in birt–hogg–dubé syndrome; an analysis of 115 flcn mutation carriers from 35 bhd familiesABSTRACT BACKGROUND: Birt–Hogg–Dubé (BHD) syndrome is an autosomal dominant condition caused by germline _FLCN_ mutation...
Bharat chawda: movies, photos, videos, news, biography & birthday | times of india_Bharat Chawda_'s 'Maru Mann Taru Thayu' to hit the big screens on April 12; check out the latest poster ...
Error 404Error 404 No encontramos la página que buscas....
Coroner 'very concerned' at lack of measures at beach where boy diedTHE CORONER HAS QUESTIONED WHY MORE IS NOT BEING DONE TO PREVENT FUTURE INCIDENTS AFTER DAVID EJIMOFOR DIED AFTER JUMPIN...
Dad who suffered 'migraines' saved as eye test spots cancerRichard Brannan, 34, had been prescribed painkillers by his GP who mistakenly thought he was suffering from migraines tr...