Prenatal Diagnosis in Denmark | European Journal of Human Genetics
Prenatal Diagnosis in Denmark | European Journal of Human Genetics"
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Prenatal diagnosis (PND) in Denmark is covered by 5 genetic departments. More than 10% of all pregnancies are monitored by amniocentesis (AC) or chorionic villus sampling (CVS).
Prenatal cytogenetic analyses are recorded in the Danish Central Cytogenetic Register (DCCR), which provides information on individual cases for genetic counselling and allows the Health
Authorities to monitor prenatal diagnosis (PND). About 40% of trisomy 21 is diagnosed prenatally. The present procedures are AC, CVS, chordocentesis, and ultrasound scan. The methods include
a wide range of cytogenetic, molecular, and biochemical analyses. Fluorescent in situ hybridisation, comparative genomic hybridisation, and fetal cells in maternal blood are currently
investigated. PND is a public health service; the expenses are covered by the counties. The National Board of Health provides guidelines for indications for PND, while termination of
pregnancy because of abnormal findings after the 12th week is evaluated on an individual basis. The current legislation prevents pre-implantation diagnosis. This year, clinical genetics was
registered as a speciality in Denmark. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS DOWN SYNDROME SCREENING AND DIAGNOSIS
PRACTICES IN EUROPE, UNITED STATES, AUSTRALIA, AND NEW ZEALAND FROM 1990–2021 Article 16 March 2023 ADVANCING FETAL DIAGNOSIS AND PROGNOSTICATION USING COMPREHENSIVE PRENATAL PHENOTYPING AND
GENETIC TESTING Article 27 June 2024 NON-INVASIVE PRENATAL TESTING IN GERMANY: A UNIQUE ETHICAL AND POLICY LANDSCAPE Article Open access 12 December 2022 INTRODUCTION Clinical use of
amniocentesis (AC) and fetal chromosome analysis was introduced in Denmark in the early seventies. Up to 1978, the number of prenatal diagnoses (PND) carried out was limited and AC only
offered to selected high-risk groups of pregnant women. In 1978, the Danish legislation made resources available in order to increase the capacity of the genetic departments offering PND.
During the following years, AC and PND became accepted preventive procedures in the Danish population and today more than 10% of our pregnancies are monitored by PND. After the first
investigation on chorionic samples by Hahnemann and Mohr [1] in 1968, chorionic villus sampling (CVS) was introduced for clinical use in Denmark in 1983 and has now become a popular
alternative to AC among Danish women. Approximately half of all prenatal analyses are now carried out by CVS. Over the years, many techniques and procedures associated with PND have been
introduced in Denmark as in the other European countries. The use of DNA techniques in the diagnosis of monogenic diseases and fluorescent in situ hybridisation (FISH) as a supplement to
cytogenetic analysis has been important. Improved ultrasound equipment is used for fetal heart scanning and for guiding cordocentesis and filter AC [2]. This paper provides an overview of
the present state of PND in Denmark with special emphasis on prenatal cytogenetic analysis. NATIONAL ORGANISATION Prenatal chromosome analysis in Denmark is carried out by 5 genetic
departments: (1) Department of Clinical Genetics, Rigshospitalet, Copenhagen; (2) The John F. Kennedy Institute, Glostrup; (3) Department of Clinical Genetics, Vejle County Hospital; (4)
Department of Clinical Genetics, University Hospital of Aarhus, and (5) Department of Clinical Biochemistry and Genetics, Odense. Prenatal metabolic or DNA analyses are performed at 4
laboratories, analysis of biochemical markers in maternal serum at local laboratories or the State Serum Institute, and genetic counselling at 6 genetic departments. All 5 genetic institutes
are public. Each institute is servicing a certain part of the 16 Danish counties corresponding to certain geographical regions. All prenatal cytogenetic diagnoses are recorded in the Danish
Central Cytogenetic Register (DCCR). AC is performed at 17 and CVS at 12 obstetrical/ultrasound departments throughout the country. Very few samples were taken in private clinics (2-4 per
year), and they were all analysed at the public genetic institutes. Screening by the triple test or ultrasound scan is offered in one county. The expenses related to PND are covered by the
National Health Service. The number of live births per year in Denmark is given in table 1. SOURCES OF INFORMATION The sources of information on PND in Denmark are: Danish Central
Cytogenetic Register, which registers sampling technique (AC or CVS), prenatal chromosome diagnoses, maternal age, indication, terminations, county, hospital, and genetic laboratory. Danish
Register of Congenital Malformations worked until 1995; the information is since then included in the Danish Birth Register. During 2 years (1994–1996), a working group has investigated the
possibilities for a Danish Register of Genetic Diseases, but finally concluded that it is at present not possible. Local registers and research registers exist at e.g. Department of Medical
Genetics, Copenhagen University (muscular dystrophy), Department of Ophthalmology, Copenhagen (hereditary eye diseases), and Register on hereditary tumour syndromes. A complete survey was
attempted 1995–1996 without success. The EUCROMIC register at the John F. Kennedy Institute contains detailed information on ambiguous prenatal diagnoses (mosaicism and discordance) after
diagnostic CVS, AC, chordocentesis, coelocentesis, and/or fetal cells in maternal blood. By 1996, it included information from all Danish cytogenetic centres. A yearly report from the Danish
Cytogenetic Central Register makes it easy to follow the activity of PND from year to year, and it is possible to obtain information about individual cases to be used for genetic
counselling. Data for 1994 and 1995 are not yet available. The register has also proved useful for a large number of research projects [e.g. 3, 4]. There has been little interest among the
genetic institutes to record DNA and metabolic analyses for monogenic diseases in the register. Consequently, it has not been possible to include this activity. The data presented below are
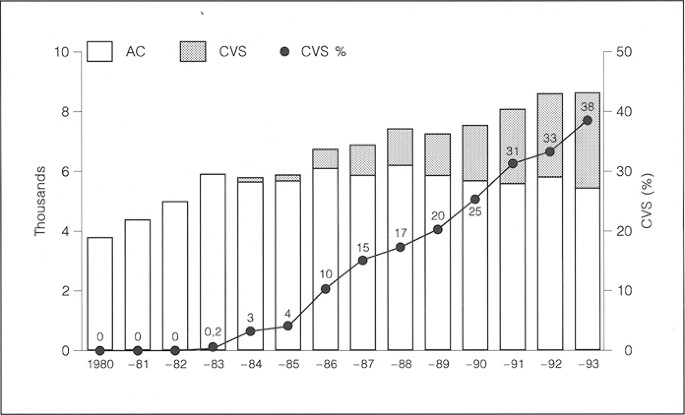
all obtained from the register and illustrate the kind of information that is recorded. Figure 1 gives an overview of the development of PND based on AC and CVS from 1980 to 1993. The
fraction of analyses based on CVS is rapidly increasing and has probably reached 50% by now. Figure 2 shows that the fraction of pregnancies that are monitored by PND has settled around 13%.
Note the increase of deliveries since 1983. Figure 3 shows that the fraction of women > 35 years who accepted PND has declined from 76% in 1983 to 65% in 1993. From the yearly reports of
the register it can be seen that the decrease has taken place mainly in the larger urban areas, which in the past showed great interest in PND; the fraction of women having PND is now more
or less the same all over the country. The number of deliveries by women of 35 years of age or more has doubled from 1980 to 1993. This increase of deliveries among older women is
significantly larger as compared to the smaller increase for all women as seen in figure 2. Whether this increase has something to do with the possibility of having PND or not is unknown.
Another explanation could be that an increasing fraction of women are employed outside home and for this reason decide to get children later in life. IMPACT OF PRENATAL DIAGNOSIS Tables 2
and 3 show indications, the number of analyses, and number of induced abortions because of abnormal findings at AC and CVS, respectively, for the period 1980–1993. Advanced maternal age is
clearly the largest group for PND by CVS or AC. Also the group with chromosomal disease or mental retardation in the close family and the group having the test for psychological reasons are
large. The fact that the frequency of induced abortions because of abnormal findings is the same in these last two groups is probably the reason that numerical chromosome aberration in the
close family is no longer regarded as a risk group requiring invasive PND. The guideline for this group is now only to offer the triple test (table 1). 1.4 and 2.4% of all AC and CVS,
respectively, result in induced abortions because of abnormal findings. Table 4 shows the number of different chromosome abnormalities detected prenatally after AC and CVS from 1980 to 1993
and the corresponding number of induced abortions. Autosomal trisomies constitute about 55% and unexpected structural aberrations about 8% of prenatally detected chromosome aberrations [5].
Almost all cases of autosomal trisomies, polyploidies and unbalanced translocations result in induced abortion. Most of those who do not have an induced abortion in these groups experienced
a spontaneous abortion before the result of the PND was available. There have been no cases of prenatally detected trisomy 21, where the women/couples decided to continue the pregnancy. The
picture is quite different for the sex chromosome aberrations, where 60–70% choose interruption of pregnancy. Figure 4 illustrates the impact of PND on the number of children born with
trisomy 21 [6]. It is assumed that all liveborn children with Down syndrome (DS) are karyotyped within the first year after birth. It is noticed that over the years about 40% of the trisomy
21 cases are detected prenatally. Increasing use of CVS raised expectations towards an increased fraction of prenatally detected trisomy 21 cases (tables 2 and 3). On the other hand, the
declining fraction of women ≥ 35 years having PND will influence the figure in the opposite direction (fig. 3). The triple test is not widely used in Denmark and may only slightly influence
the results. The changes in severe malformations in liveborns or stillbirths are listed in table 5. DIAGNOSTIC AND SCREENING PROCEDURES AVAILABLE The recommended indications for PND and
choice of method have been updated in 1994 by the National Health Service (table 6). They should only be regarded as guidelines, and it is stressed in the comments that genetic counselling
associated with PND should allow the women/couples to make their own choice of procedure according to their own wishes and to the choices they are given. SAMPLING PROCEDURES CVS was
previously performed in the 7th to 12th week [7–10], but is now usually carried out in the 10th to 12th week of gestation [11]. Second-trimester CVS is used to achieve a quicker result as
compared to AC or because of oligohydramnios [12]. As for AC, both standard and high-resolution banding techniques were developed [13, 14]. Lately, 2nd-trimester CVS or amniocentesis has
been used for obtaining a result within 24 h by using interphase FISH [15]. Amniocentesis is usually performed at the 15th to 16th week of gestation, however, a new technique, filter AC, has
been introduced where amniotic fluid is aspirated and reinjected after passage through a filter which keeps the amniotic cells [2]. This technique is performed at the 12th week of gestation
and the result of karyotyping is available within 10–12 days. Second-trimester CVS or AC in week 13 are not routine procedures in Denmark. The National Board of Health recommended, 1994,
that AC should be performed by professionals with a prior education of 100 samples and subsequent routine of 200 samples per year. For CVS the recommended number of samples was given as 250
(education) and 400 (routine). Cordocentesis is used on special indications and is normally carried out at about the 20th week. SCREENING PROCEDURES Ultrasound type I scanning is available
in all 29 obstetrical departments; 16 of these offer routine ultrasound examinations in early pregnancy and in 7 of these, the fetus is routinely screened for malformations (type II scan).
The most advanced type III scanning with Doppler technique, e.g. for congenital heart defects is only available at the larger university hospitals. Serum AFP screening for neural tube
defects combined with type II ultrasound scanning is offered routinely in a few hospitals. Triple test combined with type II ultrasound scanning is currently offered routinely in one of the
counties. CURRENT METHODS IN USE Fetal karyotyping using various conventional banding techniques (Q, G, R, C, AgNOR) is routinely performed in all cases of PND including monogenic diseases.
Special techniques were developed for the fragile X syndrome [16–19]. Recently FISH has been introduced to solve complicated structural rearrangements and to diagnose microdeletion syndromes
[20–23]. Interphase FISH for chromosomes 13, 18, 21, X, and Y is used in special cases, where a fast result is required [15]. Comparative genomic hybridisation (CGH) has also been used in
attempts to clarify complicated structural rearrangements [24]. A large number of inborn errors of metabolism are currently diagnosed by enzymological metabolic detection procedures [25–27]
and other monogenic diseases are diagnosed by various DNA techniques [28–30]. The current list of about 150 routine analyses is continuously updated. The Cu deficiency syndrome, Menkes’
disease, is diagnosed by analysis of the Cu content in chorionic villi or amniocytes [31–35]. All amniotic fluid samples are routinely analysed for AFP and most of them are also analysed for
AChE. AREAS UNDER DEVELOPMENT A large controlled study comparing interphase FISH with conventional CVS and AC, respectively, has recently been conducted in Denmark. Probes for chromosomes
13, 18, 21, X, and Y were used and the results are promising. It is not yet clear whether the FISH interphase technique will be used as an adjunct to conventional cytogenetics to achieve a
quick result (1–2 days) or whether the technique will be used as an alternative, relatively cheap, and fast stand-alone technique. Much developmental work in the prenatal genetic institutes
is devoted to metaphase FISH as to diagnose an increasing number of microdeletion syndromes and to disclose complicated structural rearrangements which in the past have been difficult or
even impossible to diagnose with conventional banding techniques [36]. As mentioned above, even CGH has proved to be usable both for detecting aneuploidies and for clarifying complicated
structural rearrangements [24]. It is still not clear whether the method will be available for routine purposes. At Rigshospitalet in Copenhagen, attempts to detect fetal nucleated
erythroblasts in maternal blood have been going on for some years, but a definitive breakthrough has not been made yet. As the Human Genome Project progresses, an increasing number of
monogenic diseases can be diagnosed prenatally by various kinds of DNA technology. Techniques for pre-implantation diagnosis are also investigated. Genetic screening for common monogenic
diseases like cystic fibrosis is under consideration. First-trimester biochemical screening and ultrasound screening for trisomy 21 is gradually coming up. The diagnostic and clinical
problems after chromosomal mosaicism, which is encountered both after AC [37] and CVS [38] are investigated in a European multicentre study funded by the EU Commission (EUCROMIC,
BMH1-CT93-1673). CURRENT LEGISLATION Termination of pregnancy is self-determined until 12 weeks. If severe disease is detected later in pregnancy, termination is accepted after approval by a
local committee. There is not yet any legislation defining severe disease. Pre-implantation diagnosis is not allowed at present. However, a new law is under debate in the Danish parliament.
PROBLEMS TO FACE IN THE FUTURE In the recent instructions from the National Board of Health on PND in Denmark, the indications have been tightened. The consequence is limited access to
prenatal diagnosis for women with DS in the close family and for women who want the test because they are afraid to get a DS child. One may fear that further limitations may be established.
During the years there has been intense debate between supporters of invasive PND and supporters of biochemical screening for DS (triple test). The supporters of the invasive procedure fear
that the National Board of Health may change its policy and reduce the access to CVS and AC for women > 35 years and offer this group the triple test instead. Most cytogeneticists feel
that this would be a step backwards. In the past, certain groups, e.g. The Ethical Council, attempted to introduce rules for specifying which prenatal detection is allowed and consequently,
for which diseases termination of pregnancy would be acceptable. We feel, that such limitations would be most unfortunate for pregnant women and would mean that they can no longer make their
own decisions. REFERENCES * Hahnemann N, Mohr J: Genetic diagnosis in the embryo by means of biopsy from extraembryonic membranes. Bull Eur Soc Hum Genet 1968;2:23. Google Scholar *
Sundberg K, Smidt-Jensen S, Lundsteen C, et al: Filtration and recirculation of early amniotic fluid. Evaluation of cell cultures from 100 diagnostic cases. Prenat Diagn 1993;13:1101–1110.
Article CAS Google Scholar * Macintosh MCM, Wald NJ, Chard T, et al: Selective miscarriage of Down’s syndrome fetuses in women aged 35 years and older. Br J Obstet Gynaecol
1995;102:798–801. Article CAS Google Scholar * Hasle H, Mellemgaard A, Nielsen J, et al: Cancer incidence in men with Klinefelter syndrome. Br J Cancer 1995;71:416–420. Article CAS
Google Scholar * Vejerslev LO, Friedrich U: Experiences with unexpected structural chromosome aberrations in prenatal diagnosis in a Danish series. Prenat Diagn 1984;4:181–186. Article CAS
Google Scholar * Mikkelsen M, Fischer G, Hansen J, et al: The impact of legal termination of pregnancy and of prenatal diagnosis on the birth prevalence of Down syndrome in Denmark. Am J
Hum Genet 1983;47:123–131. Article CAS Google Scholar * Lindsten J, Marsk L, Mikkelsen M, et al: Role of chorion villi biopsy in prenatal diagnosis of genetic disorders; in Medical
Genetics: Past, Present, Future. Liss, New York, 1985, pp 195–212. Google Scholar * Marsk L, Søndergaard F, Secher NJ, et al: Diagnostic transcervical chorionic biopsies in first trimester
pregnancies. Clin Genet 1984; 26:262–263. Article Google Scholar * Mikkelsen M, Søndergaard F, Tønnesen T, et al: First trimester biopsies of chorionic villi for prenatal diagnosis.
Experience of two laboratories. Clin Genet 1984;26:263–264. Article Google Scholar * Mikkelsen M: Cytogenetic findings in first trimester chorionic villi biopsies: A collaborative study;
in Fraccaro M (ed): First Trimester Fetal Diagnosis. Berlin, Springer, 1985. Google Scholar * Smidt-Jensen S, Permin M, Philip J, et al: Randomized comparison of transabdominal and
transcervical chorionic villus sampling and amniocentesis. Lancet 1992;340:1237–1244. Article CAS Google Scholar * Smidt-Jensen S, Lundsteen C, Lind AM, et al: Transabdominal chorionic
villus sampling in the second and third trimesters of pregnancy: Chromosome quality, reporting time, and fetomaternal bleeding. Prenat Diagn 1993; 13:957–969. Article CAS Google Scholar *
Mikkelsen M: Chromosome analysis on chorionic villi. Clin Obstet Gynecol 1987;1:533–546. CAS Google Scholar * Søndergaard F, Kristensen M, Tommerup N: High resolution chromosomes from
first trimester trophoblast cultures. Prenat Diagn 1985;5:291–294. Article Google Scholar * Bryndorf T, Christensen B, Yang X, et al: Rapid detection of numerical aberrations of
chromosomes 13, 18, and 21 in chorionic mesenchymal cells. Prenat Diagn 1993;13:815–823. Article CAS Google Scholar * Søndergaard F: First trimester diagnosis in a twin pregnancy in which
the mother is a proven carrier of the X-linked disorder Menkes’ syndrome; in Fraccaro M (ed): First Trimester Fetal Diagnosis. Berlin Springer, 1985. Google Scholar * Tommerup N, Aula P,
Gustavii B, et al: Second trimester prenatal diagnosis of the fragile X. Am J Med Genet 1986;23:313–324. Article CAS Google Scholar * Tommerup N, Søndergaard F, Tønnesen T, et al: Early
prenatal diagnosis of the fragile site at Xq27. Prenat Diagn 1991; 11:609–619. Article CAS Google Scholar * Tommerup N, Holmgren G, Steinbach P: Fragile X: Carrier detection in pregnancy.
J Med Genet 1986;23:527–530. CAS Google Scholar * Brandt CA, Hindkjær J, Strømkjær H, et al: Molecular cytogenetics: Applications in clinical genetics. Eur J Obstet Gynecol Reprod Biol
1993;50:235–242. Article CAS Google Scholar * Brandt CA, Djernes B, Strømkjær H, et al: Pseudodicentric chromosome 18 diagnosed by chromosome painting and primed in situ labelling
(PRINS). J Med Genet -102. * Hertz B, Brandt CA, Petersen MB, et al: Application of molecular and cytogenetic techniques to the detection of a de novo unbalanced t(11q; 21q) in a patient
previously diagnosed as having monosomy 21. Clin Genet 1993;44:89–94. Article CAS Google Scholar * Brandt CA, Lyngbye T, Pedersen S, et al: Value of chromosome painting in determining the
chromosomal outcome in offspring of a 12;16 translocation carrier. J Med Genet 1994; 31: 234–237. Article CAS Google Scholar * Bryndorf T, Kirchhoff M, Rose H, et al: Comparative genomic
hybridization in clinical cytogenetics. Am J Hum Genet 1995;57:1211–1220. CAS PubMed PubMed Central Google Scholar * Christensen E: Prenatal diagnosis of glutaryl-CoA dehydrogenase
deficiency: Experience using first-trimester chorionic villus sampling. Prenat Diagn 1994;14:333–336. Article CAS Google Scholar * Lykkelund C, Søndergaard F, Therkelsen AJ, et al: First
trimester prenatal diagnosis of the Hunter syndrome by direct determination of iduronate sulphatase activity in chorionic villi. Lancet 1983;i:1147. Article Google Scholar * Pedersen C,
Schwartz M, Güttler F, et al: Prenatal diagnosis of the Hurler syndrome. Dan Med Bull 1979;26:357–359. CAS PubMed Google Scholar * Lidsky AS, Güttier F, Woo SLC: Prenatal diagnosis of
classic phenylketonuria by DNA analysis. Lancet 1985;i:549–551. Google Scholar * Horn N: Menke’s X-linked disease: Prenatal diagnosis and carrier detection. J Inher Metab Dis
1996;6:159–162. Google Scholar * Tønnesen T, Søndergaard F, Mikkelsen M, et al: X-Chromosome specific probe DX13 for carrier detection and first trimester prenatal diagnosis in haemophilia
A. Lancet 1984;ii: 1269–1270. Article Google Scholar * Horn N, Søndergaard F, Damsgaard E, et al: Prenatal diagnosis of Menke’s syndrome by direct copper analysis of trophoblastic tissue;
in Fraccaro M (ed): First Trimester Fetal Diagnosis. Berlin, Springer 1985. Google Scholar * Horn N: Menke’s X-linked disease: Prenatal diagnosis of hemizygous males and heterozygous
females. J Prenat Diagn 1981;1:107–120. Article CAS Google Scholar * Tønnesen T, Gerdes A-M, Damsgaard E, et al: First trimester diagnosis of Menkes disease. Affected male fetus with low
copper values in chorionic villi. J Prenat Diagn 1989;9:159–165. Article Google Scholar * Tønnesen T, Horn N, Søndergaard F, et al: Experience with first trimester prenatal diagnosis of
Menkes disease. Prenat Diagn 1987;7: 497–509. Google Scholar * Tønnesen T, Horn N, Søndergaard F, et al: Measurement of copper in chorionic villi for first-trimester diagnosis of Menke’s
disease. Lancet 1985;i:1038–1039. Article Google Scholar * Lundsteen C, Maahr J, Christensen B, et al: Image analysis in comparative genomic hybridization. Cytometry 1995;19:42–50. Article
CAS Google Scholar * Vejerslev LO, Børlum KG, Jensen NK, et al: Prenatal diagnosis of trisomy 20 mosaicism indicating esophageal and rectal origin. Clin Genet 1985;27:263–268. Article
CAS Google Scholar * Vejerslev LO, Mikkelsen M: The European collaborative study on mosaicism in chorionic villus sampling. Data from 1986 to 1987. Prenat Diagn 1989;9:575–588. Article
CAS Google Scholar Download references ACKNOWLEDGMENT We want to thank Karen Brandum Nielsen for reviewing the manuscript. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Clinical Genetics, Juliane Marie Centre Rigshospitalet, Copenhagen, Denmark, 4032, Blegdamsvej 9, DK-2100 Claes Lundsteen * Department of Medical Genetics, John F. Kennedy Institute,
Glostrup, Denmark Lars O. Vejerslev * Department of Obstetrics and Gynaecology, Municipal Hospital, Holbaek, Denmark Lars O. Vejerslev Authors * Claes Lundsteen View author publications You
can also search for this author inPubMed Google Scholar * Lars O. Vejerslev View author publications You can also search for this author inPubMed Google Scholar RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Lundsteen, C., Vejerslev, L.O. Prenatal Diagnosis in Denmark. _Eur J Hum Genet_ 5 (Suppl 1), 14–21 (1997).
https://doi.org/10.1007/BF03405955 Download citation * Issue Date: January 1997 * DOI: https://doi.org/10.1007/BF03405955 SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative KEY WORDS * Prenatal diagnosis * Denmark * Amniocentesis * Chorionic villus biopsy * Screening
Trending News
Drought dries up copper canyon waterfall although some blame miningA waterfall in the Copper Canyon in Ocampo, Chihuahua, has dried up due to the severe drought affecting the area. The 24...
Small doses of alcohol affect driving skills | science newsScience News was founded in 1921 as an independent, nonprofit source of accurate information on the latest news of scien...
5 signs a house is a money pitThe spring home-buying season is in full swing, and if forecasts are correct it’s going to be a busy one. Despite mortga...
The bcl-2 pro-survival protein a1 is dispensable for t cell homeostasis on viral infectionABSTRACT The physiological role of the pro-survival BCL-2 family member A1 has been debated for a long time. Strong mRNA...
Kitkat introduces new flavour as chocolate lovers rush to get their hands on itTHE LATEST KITKAT CHUNKY RELEASE HAS SENT CHOCOLATE LOVERS INTO A FRENZY - AND IT'S NOT SURPRISING AFTER THE ICONIC...
Latests News
Prenatal Diagnosis in Denmark | European Journal of Human GeneticsABSTRACT Prenatal diagnosis (PND) in Denmark is covered by 5 genetic departments. More than 10% of all pregnancies are m...
Millions of aussies set for $1080 covid tax breakColin Brinsden, AAP Economics and Business CorrespondentAAP Millions of Australians may not lose a one-off COVID tax ben...
Commercial fishing, once a great lakes way of life, slips awayReporting from Milwaukee — It’s mid-April, and the gray-haired fisherman and his gray-haired son are not headed out for ...
Political cartoon u. S. Phone alert midterm election go voteSIGN UP FOR THE WEEK'S FREE NEWSLETTERS From our morning news briefing to a weekly Good News Newsletter, get the be...
Our activities | RSFFREEDOM OF INFORMATION IS FUNDAMENTAL IN ANY DEMOCRACY, BUT NEARLY HALF OF THE WORLD’S POPULATION DOES NOT HAVE ACCESS T...